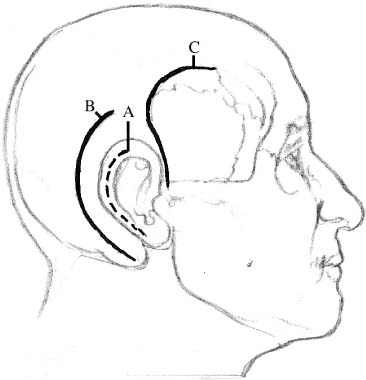
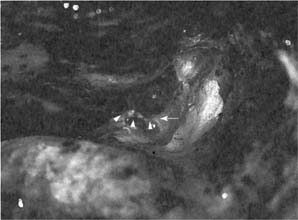
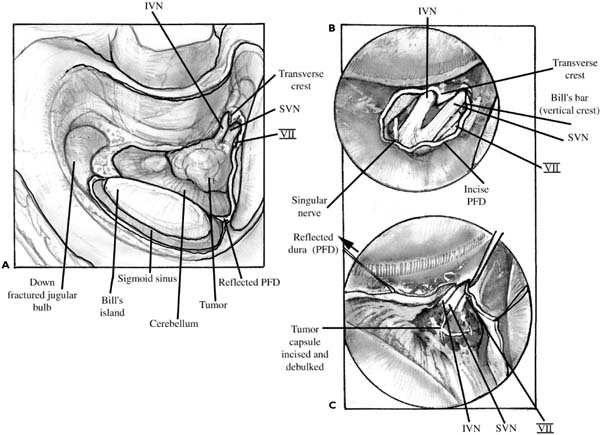
Chapter 27 This chapter provides a brief overview of approaches to the internal auditory canal, posterior fossa, and petrous apex. This discussion is not intended as a detailed reference for the neurotologic subspecialist. There are a number of approaches to the posterior and middle cranial base, which are not addressed here. The reader is referred to other extensive discussions of these procedures in the literature.1,2 The most common indication for TL surgery is a vestibular schwannoma of any size in an ear with nonserviceable hearing. Existing classification schemes for hearing include those described by Gardner and Robertson3 and Samii and Matthies.4 Controversy persists in approach selection for patients with larger tumors (greater than 2 cm of cerebellopontine angle tumor component) who have good hearing. Some institutions may favor a TL approach for these tumors because the rate of hearing preservation is low. At my institution, I offer a hearing preservation approach even in patients with larger (up to 3 cm in diameter) tumors who have Gardner class 1 hearing preoperatively. A number of variables including patient characteristics, tumor size and location, patient preference, and the results of preoperative studies determine the feasibility of hearing preservation. All of these factors must be taken into consideration when deciding on a TL approach. The TL route is frequently combined with other bone flap craniotomies performed in conjunction with neurosurgery. Retrolabyrinthine and TL bone work is frequently performed as part of the transpetrosal approach for other lesions of the middle and posterior cranial base. The TL approach is also used in total facial nerve decompression for trauma when the patient has lost hearing. There are several advantages to the TL approach when compared to other routes to the posterior cranial base. In comparison to the retrosigmoid approach, it offers direct complete exposure of the internal auditory canal (IAC). The TL approach also offers better anterior and superior exposure than the classical retrosigmoid approach. Facial nerve decompression or mobilization is facilitated through this approach. The TL route offers excellent exposure for placement of an auditory brainstem implant if required.5 There is less cerebellar retraction, and all bone work is performed extracranially, which may limit postoperative headache. Cerebrospinal fluid (CSF) leak is almost nonexistent in the TL approach.6 The primary disadvantage of this approach is the obvious loss of hearing. In larger tumors, with a wide inferior brainstem attachment, a high jugular bulb can limit the approach. This route is contra-indicated in patients with active chronic otitis media and mastoiditis. A thorough otologic and neurotologic history and physical examination should be performed on all patients. The patient’s subjective assessment of dysequilibrium, imbalance, and tinnitus intensity are reviewed. A comprehensive neurologic review of systems should be included, with particular attention to any cranial nerve symptoms. A past medical history of chronic ear disease or prior otologic surgery should be elicited. A family history of intracranial neoplasm or neurofibromatosis is of obvious importance. In addition to the standard otologic and head and neck examination, cranial nerve function and vestibular function should be assessed. Subtle physical findings may include a diminished corneal reflex, and drift and past pointing to the ipsilateral side. All patients undergo complete audiometric testing including pure tone and speech audiometry. Electrocochleography (ECoG) and auditory brainstem response (ABR) testing are performed as a preoperative baseline if hearing preservation is being considered. Preoperative vestibular testing, including electronystagmography (ENG), is also useful. Preoperative evaluation by the balance physical therapy team, including platform posturography, may prove useful in selected patients who require vestibular retraining postoperatively. All patients have undergone magnetic resonance imaging (MRI) with contrast enhancement. High-resolution computed tomography (HRCT) of the temporal bone is not required but may delineate anatomic abnormalities including a high jugular bulb, sclerotic mastoid, or anteriorly placed sigmoid sinus. Widening of the IAC also correlates negatively with hearing preser-vation. All options, including observation and radio-surgery, must be thoroughly discussed with the patient. All elements of informed consent are included in a surgery-specific consent form for TL surgery, and the external canal is painted with gentian violet preoperatively. The TL procedure should be performed in a larger operating suite. This provides ample room for equipment including the operating microscope, intraoperative monitoring systems, dissection tools including pneumatic drills, and cavitating ultrasonic aspirators. Increased room size is also needed for added personnel including neuroanesthesia, nursing staff, the multidisciplinary surgical team, intraoperative monitoring personnel, and observers. For the routine TL approach, the head is rotated 30 to 45 degrees to the contralateral side with the chin gently flexed toward the shoulder. The surgeon is seated on the same side as the anesthesia service, which is located toward the feet. The operating room nurse is positioned directly across from the surgeon. The first assistant and microscope base are positioned at the head of the table. Arterial line placement and facial nerve monitoring are always performed. Intravenous mannitol (0.5 g/kg) and dexamethasone are given for larger tumors. A limited hair shave is done, and adhesive drapes are applied. A previous abdominal incision or the left lower quadrant is also prepared for harvesting an abdominal fat graft. The head is secured with tape and an incision is outlined (Fig. 27–1). The incision is infiltrated with 1% Xylocaine with 1:100,000 epinephrine prior to the skin prep. The incision is made with a knife or an electro-cautery device. The incision is normally beveled anteriorly to provide increased surface area for closure. Muscle and periosteum are incised and elevated using the cautery or periosteal elevators. All soft tissue is removed from the lateral cranial base to completely expose the mastoid process, digastric ridge, external auditory canal, and retrosigmoid region. The anteriorly based flap is retracted and held in position with fishhook retractors. FIGURE 27–1 Outline of incisions for the translabyrinthine (A), retrosigmoid/transmeatal (B), and middle cranial fossa (C) approaches. Bone work is begun with an extended mastoidectomy. Initial drilling may be done without microscopic control. The sigmoid sinus and a limited amount of retrosigmoid dura are completely skeletonized. The mastoid tip is removed and the facial nerve, jugular bulb, and superior petrosal sinus are identified. All bone is removed from the middle cranial fossa dura. The inferior limit of the dissection is the jugular bulb, which is completely exposed or down-fractured. Usually the upper limit is the superior petrosal sinus and middle fossa dura, but the TL approach can be extended superiorly if needed. A modified labyrinthectomy is performed. The posterior cranial fossa dura and the superior petrosal sinus are traced medially, followed by removal of the posterior canal, common crus, and superior canal. In this way the facial nerve is protected and the lateral semicircular canal is removed in the final portion of the labyrinthectomy. The vestibule is widely opened and the ampullated ends of the lateral and superior semicircular canals are removed. During anterior dissection, care must be taken to avoid injury to the tympanic segment of the facial nerve. Skeletonization of the facial nerve significantly improves exposure, and the shoulder of a large diamond bur and continuous suction irrigation are used. FIGURE 27–2 Photograph of left translabyrinthine approach demonstrating remaining superior meatal bone (arrow). The asterisk indicates internal auditory canal (IAC) with tumor, and arrowheads show posterior fossa dura (PFD). The next step in the bone work is the identification of the porus acusticus. A large trough is created between the jugular bulb inferiorly and the IAC superiorly. The cochlear aqueduct is located in this region and is widely opened to allow egress of cerebrospinal fluid. Once the inferior aspect of the IAC is identified, dissection is continued superiorly with identification of the superior portion of the porus acusticus. There is a dense wedge of bone located between the superior aspect of the internal canal and the posterior fossa dura (Fig. 27–2). Bone removal in this area is important to provide adequate exposure and facilitate dissection of the facial nerve. The lateral dissection of the IAC is carried out last. This includes identification of the vertical and horizontal crest as well as the labyrinthine segment of the facial nerve. The egg-shelled bone is removed from the dura. An island of bone may be left over the sigmoid sinus. Once all of the bone work is completed, the dura of the internal auditory meatus is opened. This incision can be extended posteriorly toward the sigmoid sinus. Superior and inferior extensions of this incision can then be made toward the jugular bulb and petrosal sinus. Wide reflection of the posterior fossa dura provides complete exposure of the cerebellopontine angle. Dissection within the IAC is begun laterally. The superior and inferior vestibular nerves are sectioned sharply. The facial and cochlear nerves are identified. Facial nerve dissection is facilitated with the use of stimulus dissecting instruments. I leave the cochlear nerve intact as the tumor is dissected from lateral to medial (Fig. 27–3). This results in less traction on the facial nerve. Hemostasis is controlled with bipolar cautery and small pledgets of absorbable gelatin and thrombin. Care must be taken to dissect any vascular loops located within the IAC. Small tumors can usually be removed in an en-bloc fashion. Larger tumors require debulking using microinstruments or a cavitating ultrasonic aspirator. The role of the neurosurgeon varies based on tumor size, but at my institution all cases of vestibular schwannoma are done in a multidisciplinary manner. Once tumor removal is complete and hemostasis has been assured, the abdominal fat graft is har-vested. I also perform closure of the eustachian tube via the facial recess during the fat graft harvest. The middle ear and attic are closed with a muscle graft followed by bone wax, closing the facial recess. The abdominal fat graft is cut into bilobed strips. These strips are layered together to serially close the defect in the posterior fossa dura. A compressive mastoid dressing is placed for 48 hours. Bleeding during temporal bone dissection is usually easily controlled with bone wax, bipolar cautery, or a diamond drill. Hemorrhage from the sigmoid sinus and jugular bulb or superior petrosal sinus can be troublesome, however. Bleeding from the sinus can often be controlled with a large pledget of absorbable gelatin sponge moistened with topical thrombin and placement of a cottonoid followed by gentle pressure. The complex can be left in place and held with the arm of a self-retaining retractor while dissection is allowed to continue. Bleeding from the jugular bulb may require a firm oxidized cellulose pack. Care must be taken to avoid embolization of the packing material. Ligation of the internal jugular vein or complete occlusion of the sigmoid sinus has not been required in my experience. Bleeding from the petrosal sinus may be controlled with small clips posteriorly and with packing anteriorly. Bleeding from the subarcuate artery is easily controlled with the diamond drill. During tumor work, I have found that a suction bipolar is very effective for controlling bleeding and facilitating tumor dissection. FIGURE 27–3 (A C) Illustrations of tumor dissection from internal auditory canal. PFD, Posterior fossa dura; IVN, inferior vestibular nerve; SVN, superior vestibular nerve.
BASIC NEUROTOLOGIC PROCEDURES
TRANSLABYRINTHINE (TL) APPROACH
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree