Audiologic Testing: Introduction
Otolaryngologists often rely on audiologic test results to determine the course of treatment for a given patient. Many of the tests constituting the diagnostic audiologic battery of 20 years ago have now been replaced with newer procedures with greater specificity, sensitivity, and site of lesion accuracy. This is exemplified by the fact that the terms “sensory” or “neural” can now frequently replace the term “sensorineural.” In addition, audiologic tests have gone beyond the realm of identifying anomalies in structure to identifying anomalies in function. The logical extension of this advancement is to provide the audiologist and otolaryngologist with information related to prognosis and rehabilitation.
Audiologic tests can be classified according to measures of hearing threshold, suprathreshold recognition of speech, assessment of middle ear function, assessment of cochlear function, determination of neural synchrony and evaluation of vestibular function. The test correlates associated with these measures are pure-tone audiometry, speech recognition, the immittance battery, otoacoustic emissions, electrophysiology, videonystagmography, and rotary chair assessment. The latter two procedures are discussed elsewhere in this textbook.
Audiologic test results should always be interpreted in the context of a battery of tests because no single test can provide a clear picture of a specific patient. In addition, the combination of objective and subjective (behavioral) tests provides a cross-check of the results. There are no age restrictions for audiologic testing; it is now possible and recommended to test newborns within days of birth.
Audiometry
The audiogram is a graph that depicts threshold as a function of frequency. Threshold is defined as the softest intensity level that a pure tone (single frequency) can be detected 50% of the time. Intensity is designated on a normalized decibel hearing level (HL) scale that takes into account the differences in human sensitivity as a function of frequency. The typical range of frequencies tested does not cover the entire range of human hearing (20–20,000 Hz). Instead, the range includes the frequencies considered to be essential for understanding speech (250–8000 Hz). Most testing is administered at discrete octave frequencies. However, when threshold differences between adjacent octaves exceed 15 dB, inter-octave frequencies should be tested. This is particularly true at 3000 and 6000 Hz, where “notches” in audiometric configuration often typify noise-induced hearing loss. Thresholds are measured clinically in 5-dB steps. There is a test-retest variability of ±5 dB. Therefore, a change of 10 dB may not necessarily represent a true threshold shift.
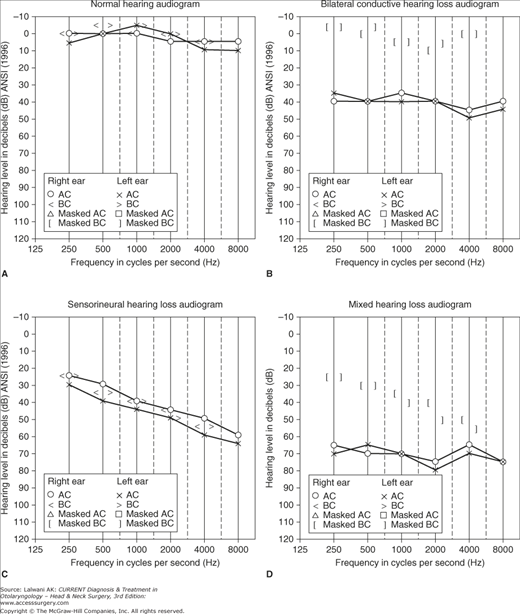
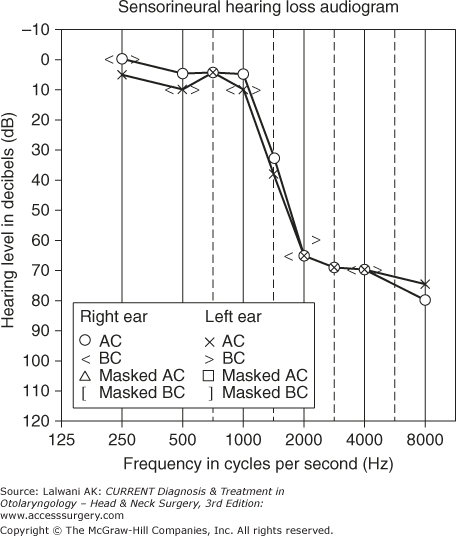
Thresholds can be obtained using air conduction (AC) or bone conduction (BC). Sound transmission via earphones, foam inserts, or loudspeakers requires the movement of air molecules; therefore, it is termed air conduction. This testing assesses the entire auditory system from the outer ear to the auditory cortex. Testing through loudspeakers (sound field) cannot isolate differences between ears. The advantages of insert earphones over over-the-ear (supra-aural) earphones include the prevention of collapsing ear canals, greater attenuation from ambient noise, and greater interaural attenuation (the loss of sound energy that occurs as the signal travels from one ear to the other either around the head or through the bones of the skull). Interaural attenuation is also referred to as “crossover.” The amount of interaural attenuation varies as a function of the transducer type and frequency; it is typically 0 dB for bone conduction, 40–60 dB for supra-aural earphones, and 55–70 dB for insert earphones. AC thresholds are marked on the audiogram with an “O” for the right ear and an “X” for the left ear. BC thresholds are obtained using a small vibrator placed on the forehead or on the mastoid bone. Thresholds are typically indicated on the audiogram with the symbols “<” and “>” (unmasked) or “[” and “]” (masked). Because the skull vibrates as a whole, BC thresholds primarily reflect the contribution of the inner ear, mostly bypassing the function of the outer and the middle ear. The comparison of AC thresholds and BC thresholds provides an initial differentiation between conductive, mixed, and sensorineural involvement. Sensorineural hearing loss is characterized by equivalent air and bone conduction (ie, air–bone gaps of less than 10 dB). Conductive hearing loss is characterized by BC thresholds within normal limits, with a concurrent gap between the poorer AC and better BC thresholds of 10 dB or more. A mixed hearing loss contains air–bone gaps with the bone conduction thresholds outside of the normal range. Figure 45–1 (A–D) shows audiograms depicting normal hearing and these three types of hearing loss.
Both air and bone conduction thresholds may be obtained using an approach that ascends or descends in intensity but are typically determined using a bracketing technique. If tones are presented at high intensity levels, both air- and bone-conducted stimuli can evoke vibrotactile sensations. For AC, vibrotactile thresholds may occur at 90 dB HL at 250 Hz, and at 110 dB HL at 500 and 1000 Hz. For BC, vibrotactile thresholds may occur at 30–35 dB HL at 250 Hz, 55 dB HL at 500 Hz, and 65–70 dB at 1000 Hz. Therefore, patients with severe hearing loss may appear to respond at lower (softer) levels than their true auditory thresholds. For that reason, the tester should ask the patient whether the stimulus was heard or felt when approaching the aforementioned intensity levels. Furthermore, BC greater than approximately 45–60 dB HL in the lower frequencies and 70–75 dB HL in the mid and higher frequencies cannot be measured due to equipment output limits for bone-conducted stimuli. Thus, listeners with severe or profound losses may have real, but nonmeasurable, air–bone gaps, and one must not automatically assume that a profound hearing loss is exclusively sensorineural. This is one of several reasons why a battery of diagnostic test results should always be considered, as opposed to any single measure.
One of the most important yet confusing aspects of hearing testing is to ensure that the auditory function of each ear is measured independently. In some situations, a noise is presented to the non-test ear to prevent it from responding to a signal presented to the test ear. This is referred to as masking. Masking is required for AC whenever the difference between the air conduction presentation level and the non-test ear BC thresholds exceeds approximately 40 dB for the lower frequencies and 60 dB for the higher frequencies. For BC testing, masking should be used whenever there is any difference in the AC and BC thresholds, since there is essentially no interaural attenuation by bone conduction. When the masking presented to the non-test ear crosses over to the test ear, a masking dilemma results. Usually, this occurs when a patient has a large bilateral conductive hearing loss. The use of insert earphones greatly minimizes these occurrences because of the greater interaural attenuation they provide. Failure to mask appropriately may have potentially serious medical and audiologic consequences.
Table 45–1 provides a general guideline for interpreting degrees of hearing loss based on audiometric findings. Levels should be categorized somewhat more stringently for children.
| Hearing Threshold | Interpretation |
|---|---|
| 0–25 dB | Hearing within normal limits |
| 26–50 dB—Mild hearing loss | Has difficulty with soft sounds, background noise, and when at a distance from the source of the sound |
| 51–70 dB—Moderate hearing loss | Has significant difficulties with normal conversational level speech and relies on visual cues |
| 71–90 dB—Severe hearing loss | Cannot hear conversational speech and misses all speech sounds |
| Can hear environmental sounds, such as dogs barking and loud music | |
| 91+ dB—Profound hearing loss | Hears only loud environmental sounds, such as jackhammers, airplane engines, and firecrackers |
Speech Testing
One commonly used speech measure is the speech reception threshold (SRT). The SRT is the lowest intensity level at which a patient can correctly repeat 50% of common bisyllabic words such as “hotdog” or “baseball.” These results should correspond with pure tone thresholds. However, caution must be exercised in using the SRT as the only indication of hearing sensitivity. An example of how the SRT can provide misleading information is shown in Figure 45–2. Note that for this patient, the SRT is 5 dB, well within the range of normal hearing. This value reflects the normal auditory sensitivity at 500 and 1000 Hz. Further inspection of the audiogram illustrates that this patient has a moderate hearing loss above 1000 Hz and will have considerable difficulty hearing in many acoustic environments. The only true purpose of the SRT is to validate the pure-tone findings. A variation of the SRT is the speech detection threshold (SDT) or speech awareness threshold (SAT), which is the softest level at which a person detects (as opposed to understands) the presence of speech sounds. Pure-tone testing and SRT, SAT, or SDT yield information about hearing sensitivity. Most listening is actually done at suprathreshold levels. Therefore, to define a person’s true auditory capacity, measures reflecting suprathreshold listening and clarity must be included. Word recognition testing (formerly referred to as speech discrimination testing) assesses a patient’s ability to identify monosyllabic words. A list of words are typically presented to the patient at approximately 40 dB above the SRT, or at a comfortable listening level if 40 dB is either too loud for the patient or incongruous with the audiometric configuration.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree