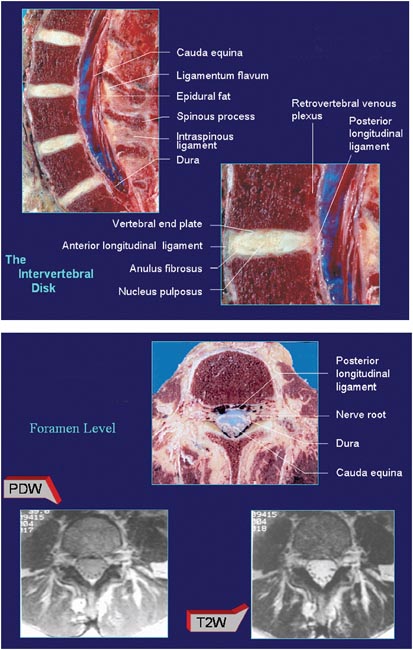
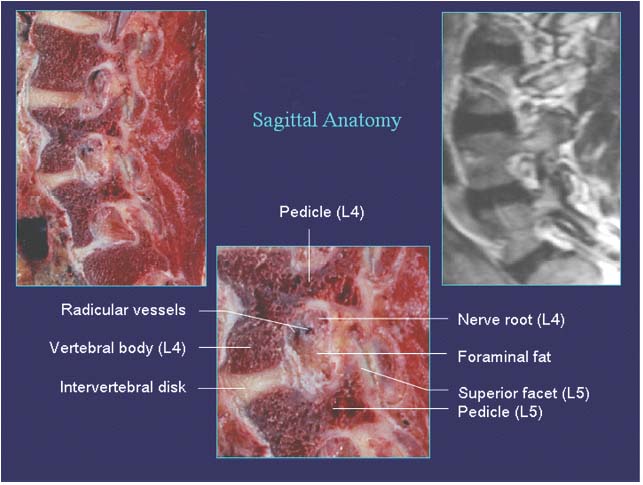
13 Applied Anatomy and Percutaneous Approaches to the Lumbar Spine After careful review of the anatomy of the spine in humans and in various primates, Putz and MüllerGerbl concluded in 1996 that the lumbar portion of the vertebral column has the ideal structure to simultaneously optimize the functions of mobility and stability.1 However, low back pain is the predominant cause for seeking medical advice in the modern era. It is necessary for a spine surgeon to have a thorough knowledge of clinical and surgical anatomy of this region. Because the present text focuses on the percutaneous endoscopic disk surgeries, here we have tried to restrict the discussion to the anatomy relevant to endoscopic spine surgery. • Although identifying the appropriate vertebral level for a percutaneous procedure can be easily accomplished by fluoroscopy, knowledge of the surface anatomy is necessary for a better topographical orientation for surgery. • The most prominent and possibly the only palpable landmarks of the lower back are the lumbar spinous processes. They present a flatter surface at the posterior tip as compared with the thoracic region. • The L4 and L5 spinous processes are shorter than other lumbar segments and are sometimes difficult to pal-pate; especially the L5 spinous process. The L4 spinous process is the last spinous process that shows movement on palpation during flexion–extension range of motion (ROM). • Generally the L4 spinous process is in a horizontal plane with the superior boundary of the iliac crest; in 20% of the population, however, the iliac crest is in line with the L5 spinous process.2 • The tips of the transverse processes are located ~5 cm from the midline and are not palpable. • The level of the superior border of the iliac crest in relation to the corresponding disk space is important in the surgeon’s decision-making process. • When viewed from above, the vertebral bodies of the lumbar spine are large and kidney shaped. • They are larger in males than in females. • The pedicles of the lumbar vertebrae are short and stout. • The superior vertebral notch is less distinct than in the cervical region, but the deep inferior vertebral notch forms the roof of the neural foramen. • The transverse process projects posterolaterally after originating from the junction of the lamina and pedicle on the same side. • They lie anterior to the articular process but posterior to the intervertebral foramen (IVF). • The lumbar transverse processes are quite long, with those of L3 being the longest. • The intertransverse distance at L4-L5 is much smaller than at L3-L4 and even smaller at L5-S1. • The accessory process projects from the posteroinferior part of the transverse process with the corresponding lamina. • Two superior articular processes are found for each lumbar vertebra, with a hyaline cartilage covered facet at the end of the process. • The facets are oriented in a vertical plane. Each lumbar articular facet faces posteromedially. • The orientation of the superior articular facet varies with different vertebral levels; for example, the L4 superior facets (L3-L4 joint) are more sagittally oriented than the L5 facets (L4-L5 joint). Also the L5-S1 joint is more coronally oriented than the L5 facet (L4-L5 joint). • There are two inferior articular processes with a facet that exactly conforms to the superior facet of the vertebral body below. • The facets of the superior and inferior articular processes of a vertebra form a zygapophyseal joint. • The facet joint is a synovial type of joint with a joint capsule surrounding it (Fig. 13.1). The IVF is an area of great surgical importance for percutaneous endoscopic procedures both because it harbors the exiting nerve root and other vascular structures and because it is the area of entry for endoscopic spinal access (Fig. 13.2). Fig. 13.1 General anatomy of the spine. (From Laser Anatomy videodisc series Clinical and Imaging Anatomy of the Lumbar Spine and Sacrum by Wolfgang Rauschning, MD, PhD.) Fig. 13.2 Anatomy of the intervertebral foramen and its boundary. (From Laser Anatomy videodisc series Clinical and Imaging Anatomy of the Lumbar Spine and Sacrum by Wolfgang Rauschning, MD, PhD.) The most unique feature of the boundaries of the foramen is that it contains two mobile types of joints—intervertebral disk (IVD) and zygapophyseal joints. Because of the mobility of these joints, the dimensions of the foramen change dynamically. The boundaries are as follows: • Roof: inferior vertebral notch of the pedicle of the superior vertebrae, ligamentum flavum at its outer free edge • Floor: superior vertebral notch of the pedicle of the inferior vertebrae, posterosuperior margin of the inferior vertebral body • Anterior wall: include the posterior aspect of the adjacent vertebral bodies, the IVD, lateral expansion of the posterior longitudinal ligament, and the anterior longitudinal venous sinus • Posterior wall: posteriorly bounded by the superior and inferior articular process of the facet joint at the same level as the foramen, and the lateral prolongation of the ligamentum flavum • Medial wall: dural sleeve • Lateral wall: a fascial sheet and overlying psoas muscle • Spinal nerves (combined ventral and dorsal root into the root sheath) • Dural root sleeve, which becomes continuous with the epineurium of the spinal nerve at the distal end of the foramen • Lymphatic channels • The spinal branch of a segmental artery, which after entering the foramen divides into three branches to supply the posterior arch, neural and intracanal structures, and posterior part of the vertebral bodies • Communicating veins between internal and external vertebral venous plexus • Two to four recurrent meningeal (sinuvertebral) nerves • Adipose tissue surrounds all the listed structures. • The greatest superoinferior dimension of the IVF is at L2-L3, and the dimension decreases from superior to inferior, which means it is smallest at L5-S1. • The anteroposterior dimension remains more or less constant at all levels in the lumbar spine and is less than the superoinferior dimensions (at L5-S1, however, the anteroposterior dimension is greater than the supero-inferior dimension). • From L1 to L4, IVF has a shape similar to an inverted pear, whereas at L5 the foramen is more oval. • IVF dimensions in the male are slightly larger than in the female. • With aging and degeneration, the foraminal dimensions change. • More recent knowledge of the ligaments suggests that ligaments are found mainly at three locations in the foramen: internal, intraforaminal, and external zones. • Internal ligaments are found in the inferior aspect of the medical portion of the foramen attaching the posterolateral aspect of the disk to the anterior surface of the superior articular process, bridging the superior vertebral notch of the inferior vertebra and converting the notch into a compartment through which veins are commonly found. • The intraforaminal ligaments have three basic types: —The first type runs from the base of the pedicle to the inferior border of the same vertebral body. The recurrent meningeal nerve and a branch of the spinal artery are commonly found in the compartment formed by this ligament. —The second type of ligament attaches to the angle formed by the posterior end of the pedicle with the base of the transverse process and extends to the posterolateral part of the same vertebral body. Through this anterosuperior compartment, a large branch of segmental artery was observed to travel. —The third type of ligament was found to originate from the upper anterior portion of the superior articular facet extending to the posterolateral body of the vertebra above. The exiting root lies directly over this ligament. • External ligaments have a common attachment to the base of the transverse process. From this they fan out in three different directions: superior, inferior, and transverse, attaching to the vertebral body of the same or a lower vertebra. They also form many small compartments through which neurovascular elements pass to or from the spinal canal. • During the percutaneous endoscopic lumbar diskectomy procedure, these ligaments are not distinguished separately because they have a minimal effect on the success of the operation. • The plexus of veins surrounding the external aspect of the vertebral column is called the external venous plexus. • They can be divided into anterior and posterior depending on the location in relation to the vertebral body. • They communicate with segmental veins and also with the internal venous plexus through IVF and transosseous channels. • Those veins located beneath the bony elements of the vertebral foramina (e.g., laminae, spinous processes, pedicles, and bodies) and embedded in a layer of loose adipose tissue. • They contain many interconnected longitudinal channels coursing anteriorly and posteriorly to the canal forming the Batson plexus. • The peculiarity of this plexus is that it is a valveless plexus. • Most of the bleeding is from the venous plexus around the foraminal area. This can be a potential mine in the foraminal adipose tissue, so pay attention during dissection around here. It is essential to avoid or control bleeding for successful surgery. • External arterial supply to the lumbar spine comes from the lumbar segmental arteries. • The lumbar segmental arteries send spinal branches to the vertebral canal through the IVF. • On entering the IVF, each spinal branch further divides into three branches. • One branch courses posteriorly to supply the laminae, ligamentum flavum, spinous process, articular processes, posterior epidural tissue, and dura. • The anterior branch supplies the posterior aspect of the vertebral body. • A third branch (neural branch) courses to the spinal nerve and supplies the ventral and dorsal roots. • It is important to review the foraminal sagittal magnetic resonance imaging (MRI) to find any abnormal arteries at the lower part of the foramen at the entry site for this procedure. Such an abnormal artery can be a contraindication. Important nervous structures related to percutaneous procedures are described here. • The spinal cord generally ends at or around the lower level of the L1 lumbar vertebra due to differential growth of the spinal cord and vertebral somites. • Dorsal and ventral roots, originating around the level of the thoracolumbar junction, travel through the lumbar cistern as the cauda equina before entering the dural sheath. • The lumbar nerve root has to travel a considerable distance into the nerve root canal (the region in which the nerve splits from the dura to the lateral boundary of the relevant IVF) with a more oblique course before reaching the destined IVF. • There is an enlargement at the end of the dorsal root just proximal to the point at which it joins the ventral root called the dorsal root ganglion (DRG). • The DRG increases in diameter from L1 to L5. • Because the S1 root canal is short, the DRG for S1 mostly lies intraspinally. • Topographically, Hasegawa et al (1996) categorized the ganglia as being intraspinal (within the canal), foraminal (within the IVF), and extraforaminal.3 • The DRG of the L1 to L5 root lies mostly inside the IVF with the upper ganglia more laterally and lower ganglia more medially into the IVF. • As mentioned earlier, the S1 root ganglion is mostly intraspinal. • Care must be taken to prevent manipulation or heat injury to the DRG because the most frequent complication is a postoperative dysesthesia.
Surface Anatomy
Osseous Anatomy
Vertebral Bodies
Pedicles
Transverse Process
Articular Process
Superior Articular Processes
Inferior Articular Processes
Facet Joints
Anatomy of the Intervertebral Foramen
Boundaries of the Foramen
Structures in the Intervertebral Foramen
Characteristics of the Intervertebral Foramen
Accessory Ligaments of the Intervertebral Foramen
Vascular Anatomy in Relation to the Foraminal Region
Venous Supply
External Venous Plexus
Internal Venous Plexus
Arterial Supply
External
Internal
Nerves of the Lumbar Spine in Relation to the Intervertebral Foramen
Dorsal and Ventral Roots and Spinal Nerves
Dorsal Root Ganglia
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree