Chapter 15 This chapter deals exclusively with the evaluation of a patient who has pupils of unequal size (anisocoria). By simply noting the shape of each pupil and checking its response to a bright light, anisocoria can be classified into four broad categories: (1) pupils with irregular or distorted shape; (2) pupils of normal shape but the larger pupil constricts poorly to light; (3) the smaller pupil reacts poorly to light; (4) an anisocoria in which both pupils have normal shape and equal constriction to light. The reader is referred to the appropriate broad category based on the results of this cursory examination of the pupils. The fifth broad category of anisocoria is for the situation where a history of transient anisocoria is given by the patient, yet a complete pupillary examination is normal. Within the text corresponding to each broad category, the most common diagnostic possibilities are given. The classical presentation of each disease is described with emphasis on diagnostic clues. “Red flags” alert the clinician to common diagnostic errors or to the possibility of other diagnoses. As a quick reference guide, Table 15–1 provides an overview of specific disease states in each of the five broad categories of anisocoria. Additional information on pupil testing can be found in Chapter 2. 1. Distortion of pupillary shape is most often due to damage to the iris stroma (pigment epithelium, connective tissue, iris dilator, and sphincter muscles). 2. Ask specifically about past or recent ocular trauma, and look for tears in the iris sphincter with a slit lamp. 3. Ask about prior intraocular surgery, such as cataract extraction or repair of a retinal detachment. Mechanical distortion or wound scarring can deform the shape of the pupil. 4. Ask about prior ocular inflammation such as iritis or ophthalmic herpes zoster. Postinflammatory synechiae and fibrosis can peak the pupil at points of iris adhesions. 5. Ischemia of the iris muscles rarely causes focal damage and pupillary distortion. However, this may occasionally occur with vasculitis, giant cell arteritis, severe atherosclerosis, or acute angle-closure glaucoma. 6. A few idiopathic syndromes cause progressive iris atrophy and pupillary distortion in young persons. These include the iridocorneal-endothelial (ICE) syndromes and pigment dispersion syndrome (Fig. 15–1). 7. Any of the above situations can be evaluated with a slit lamp. 1. Careful history taking and slit-lamp examination should evaluate for iris sphincter damage due to past or recent trauma, inflammation, ischemia, atrophy, etc. (see Broad Category 1). 2. The pupillary light reflex is best viewed in a darkened room, with a focal bright light source. This maximizes the amplitude and velocity of the pupillary contraction so that small or slow movements of the iris sphincter can be detected with the naked eye. If a pupil reacts poorly to light stimulation, then the near reflex (the triad of accommodation, convergence, and pupilloconstriction) should be checked. 3. The near reflex is best viewed in moderate room lighting. The patient should be encouraged to try and focus as hard as possible on an accommodative target such as a near acuity card or a small picture. The amplitude and velocity of the pupillary contraction from the near reflex is normally equal to or less than the light reflex. 4. If the contraction to light is poor and pupillary contraction from the near reflex exceeds the light response, this is called light-near dissociation (Fig. 15–2). Light-near dissociation may be unilateral or bilateral. It never occurs in normal patients. 5. Examination of the lids, ocular motility, and external orbit is important to determine if the anisocoria is an isolated abnormality or one part of a clinical syndrome.
ANISOCORIA
BROAD CATEGORY 1: ANISOCORIA IN WHICH ONE OR BOTH PUPILS HAVE IRREGULAR OR DISTORTED SHAPE
QUESTIONS TO ASK AND POINTS TO KEEP IN MIND
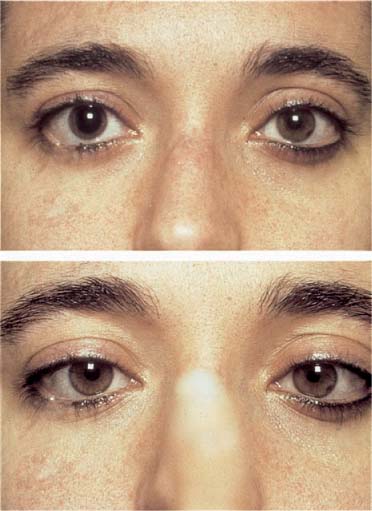
BROAD CATEGORY 2: ANISOCORIA IN WHICH THE PUPILS ARE ROUND AND THE LARGER PUPIL REACTS POORLY TO LIGHT
QUESTIONS TO ASK AND POINTS TO KEEP IN MIND
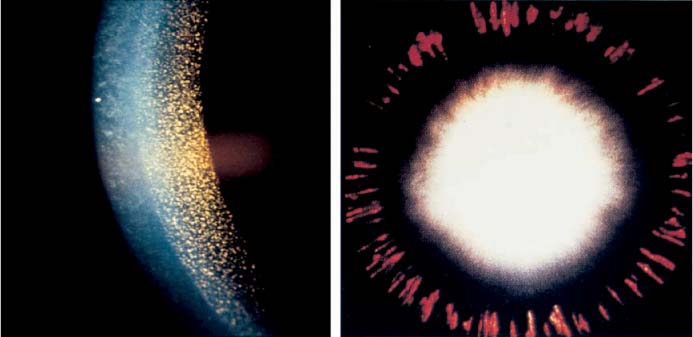
Broad Category | Diagnoses |
|---|---|
1: One or both pupils have irregular shape | Trauma, sphincter tear, ocular inflammation, acute angle closure glaucoma, intraocular surgery, ICE, pigment dispersion syndrome |
2: Anisocoria in which both pupils are round and the larger pupil reacts poorly to light | Oculomotor nerve palsy, tonic pupil, structural damage to the iris sphincter, pharmacologic mydriasis |
3: Anisocoria in which both pupils are round and the smaller pupil reacts poorly to light | Old tonic pupil, aberrant regeneration of an oculomotor nerve palsy, iris adhesions and synechiae, pharmacologic miosis |
4: Anisocoria in which both pupils are round and react normally to light | Horner’s syndrome, physiologic anisocoria |
5: Transient anisocoria | Acute glaucoma, ophthalmoplegic migraine, cluster headache, tadpole-shaped pupil, benign episodic mydriasis |
ICE, iridocorneal endothelial syndrome.
FIGURE 15–1 Slit lamp view of the iris in a patient with pigment dispersion syndrome. Left: Pigment deposits are visible on the corneal endothelium. Right: Marked transillumination defects are consistent with areas of iris atrophy.
FIGURE 15–2 Example of pupillary light-near dissociation in the right eye. Top: The anisocoria is easily visible in room light. In dim lighting, when a focal light was shone directly at the right eye, the right pupil showed a minimal contraction; that is, poor light reflex (not pictured). Bottom: In dim lighting, the patient is focusing on a close target (accommodative effort) to initiate the near reflex. The eyes are converging and the right pupil is markedly constricted now. Thus, the right pupil has a poor light response with a better near reflex, which is light-near dissociation. Further examination revealed other features confirming a right tonic pupil.
PERIPHERAL OCULOMOTOR NERVE PALSY
Classic Presentation
• The pupil is large with a poor light reflex (small contraction amplitude and slow velocity) compared to the normal pupil. The pupillary near response is equally poor.
• The large pupil constricts as well as the contra-lateral normal pupil to full miotic strength 1% pilocarpine. It may also constrict to dilute 0.1% pilocarpine due to cholinergic supersensitivity.
• The ipsilateral ptosis may be partial or complete.
• There is limited ocular motility in supraduction, infraduction, and/or adduction of the eye with the larger pupil.
• Abduction is normal.
Red Flags
 Rarely, an oculomotor nerve palsy presents as an isolated anisocoria; that is, only pupillary fibers are involved, while ocular motility and levator function are otherwise normal.1 In this rare circumstance, the pupil is large and a weak light and near reflex is preserved.
Rarely, an oculomotor nerve palsy presents as an isolated anisocoria; that is, only pupillary fibers are involved, while ocular motility and levator function are otherwise normal.1 In this rare circumstance, the pupil is large and a weak light and near reflex is preserved.
 In contrast, a completely dilated pupil that exhibits no movement to light or near stimulation in presence of normal ocular motility and levator function is almost never an oculomotor nerve palsy. It is more commonly due to pharmacologic “manipulation” or acute denervation such as in Adie’s tonic pupil (see section later in this chapter).
In contrast, a completely dilated pupil that exhibits no movement to light or near stimulation in presence of normal ocular motility and levator function is almost never an oculomotor nerve palsy. It is more commonly due to pharmacologic “manipulation” or acute denervation such as in Adie’s tonic pupil (see section later in this chapter).
 A dilated pupil with distorted shape or segmental palsy is not an oculomotor nerve palsy.
A dilated pupil with distorted shape or segmental palsy is not an oculomotor nerve palsy.
FASCICULAR (MIDBRAIN) OCULOMOTOR NERVE PALSY
Classic Presentation
• Clinical features of a fascicular oculomotor nerve palsy are essentially the same as a peripheral palsy.
• Consider the midbrain whenever the oculomotor nerve palsy demonstrates only partial weakness because the somatic and parasympathetic functions of the oculomotor nerve are still in separated fiber bundles as they traverse the midbrain tegmentum.
• Other neurologic deficits are often present because adjacent midbrain nuclei and fascicles are frequently affected by the same lesion. For example, a unilateral oculomotor nerve palsy and contra-lateral hemiparesis (Weber syndrome) is due to a lesion involving the fascicular oculomotor nerve and ipsilateral cerebral peduncle.
TONIC PUPIL (ADIE’S)
Classic Presentation
• Most cases are idiopathic and occur in women between the ages of 20 and 50 years.
• An acute tonic pupil is very dilated with no or poor reaction to light or near stimulation.
• The pupillary light reflex often appears to be absent with the naked eye, but closer examination with high magnification at the slit lamp will reveal focal areas of weak contraction interspersed with areas of segmental palsy within the iris sphincter.
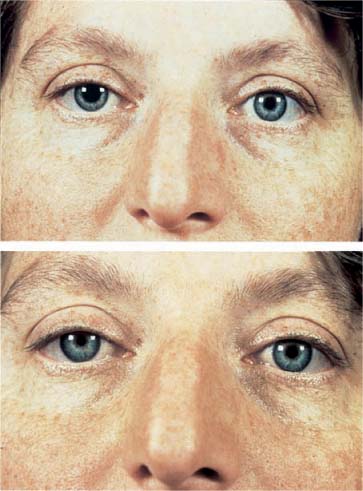
• An acute tonic pupil constricts better than the normal pupil to dilute 0.1% pilocarpine because of denervation cholinergic supersensitivity (Fig. 15–3).
• In the chronic phase, the pupillary contraction to a near stimulus is greater than to light; that is, there is light-near dissociation. However, the contraction velocity is slow and sustained (tonic).
• The redilation movement of the pupil is also slow and sustained.
Red Flags
 An acute tonic pupil that is freshly denervated has almost no response to light or near stimulation. Thus, it is easily mistaken for a pharmacologically dilated pupil. The presence of segmental areas of weak, low-amplitude contractions and marked constriction to dilute (0.1%) pilocarpine help distinguish a tonic pupil (see sidebar). Cholinergic supersensitivity may take weeks to develop but can occur in as little as 4 to 5 days (see Chapter 37) following denervation.
An acute tonic pupil that is freshly denervated has almost no response to light or near stimulation. Thus, it is easily mistaken for a pharmacologically dilated pupil. The presence of segmental areas of weak, low-amplitude contractions and marked constriction to dilute (0.1%) pilocarpine help distinguish a tonic pupil (see sidebar). Cholinergic supersensitivity may take weeks to develop but can occur in as little as 4 to 5 days (see Chapter 37) following denervation.
FIGURE 15–3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree