24

Anesthesia for Sinus Surgery
The success of endoscopic sinus surgery is greatly dependent upon properly administered anesthesia. The physical and emotional well-being of the patient, not to mention a safe field for the surgeon to work, can be positively or negatively influenced by the anesthetic. Disastrous anesthesia-related complications have been reported in patients undergoing endoscopic sinus surgery.1–5 The goal of the anesthesiologist must be to minimize the chances for complications while providing the best surgical field possible.
 Preoperative Evaluation
Preoperative Evaluation
The goal of the preoperative evaluation of a patient should be to eliminate negative outcomes as much as possible. Every patient must have an appropriate history and physical examination documenting the major medical problems and reasons for the surgery. Ideally, laboratory tests would be ordered based on the history and physical of the specific patient. This would be possible where the preadmission testing process is part of an anesthesia pre-operative clinic. However, when this is not possible, the laboratory testing is usually done by a predetermined protocol. The protocol successfully used by our ambulatory surgery facility in several thousand patients is as follows:
1. Under age 16: – no laboratory tests required
2. 16 to 40 years: hemoglobin/hematocrit for women
3. 40 to 59 years: in addition to the above, blood urea nitrogen (BUN), glucose, and electrocardiogram
4. 60 years and older: in addition to the above, hemoglobin/hematocrit for men
5. Pregnancy test for women of childbearing age
For those patients with a history of pulmonary disease, a chest x-ray is obtained.
Most of our ESS is done in a freestanding ambulatory surgery center. Because the surgery center is not attached to the hospital, some patients with certain medical problems are not candidates for surgery and anesthesia at the freestanding ambulatory surgery center. If, as part of the preoperative evaluation, a patient is found to have one of these conditions, the surgery is scheduled for the hospital setting. There are very few patients in this category. In our practice, where 200 to 300 ESS procedures are done in the ambulatory surgery center each year, fewer than 1% are done in the hospital. Often the sicker patients will still have ambulatory surgery, but their conditions dictate a setting where more intense medical resources are easily available. Many of these patients will stay 1 or more nights in the hospital to be treated or observed for problems related to their underlying medical conditions. These underlying medical conditions include
1. Serious cardiac conditions where congestive heart failure or angina is a significant possibility
2. Severe pulmonary compromise where extubation after general anesthesia or intubation for respiratory failure is a significant possibility
3. Documented malignant hyperthermia (MH) or a first-degree relative with MH
4. Known or significant suspicion that the patient will present a difficult endotracheal intubation
5. Massive obesity (greater than twice ideal weight), mainly because of respiratory and airway problems
 Anesthetic Management
Anesthetic Management
There are two main choices in anesthetic management for ESS: general anesthesia or monitored anesthesia care (MAC). The decision in favor of one type of anesthetic over another is based on many factors. The anesthesiologist and surgeon must work together to provide the best conditions for the surgery in this area of shared responsibility. Those who favor MAC cite the simplicity and safety that have been demonstrated for this modality.6–8 In addition, some nasal and sinus surgeons believe that MAC decreases the chances of the surgeon going through the upper segment of the ethmoid sinus through the cribriform plate into the cranium because of patient feedback. Thus, if the patient suddenly feels pain while working on the ethmoid sinus, the surgeon would be instantly alerted to the possibility of being too close to the cribriform plate. At least one study has found lower blood loss in MAC compared with general anesthesia.9 The average blood loss for MAC compared with general anesthesia was not dramatically lower and would not have significant clinical consequences.
Practitioners who favor general anesthesia do so for several reasons. Airway control is easier under general anesthesia. This is especially important for patients with asthma, chronic obstructive pulmonary disease (COPD), bronchitis, or bronchiectasis. Patients who have had previous sinus surgery may be difficult to regionally block with local anesthesia because of the difficulty of the anesthetic flowing through the scar tissue. Anxious patients are also difficult patients for MAC, requiring a great deal of sedation, obtunding the patient, and limiting the patient’s ability to manage secretions.
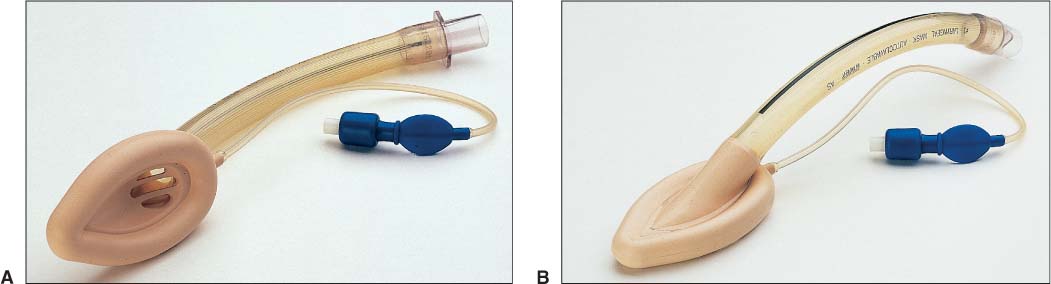
A general anesthetic requires either an endotracheal tube placement or laryngeal mask airway (LMA) (Fig. 24–1).
CONTROVERSY
LMA is now the surgeon’s (HLL) choice for nearly all ESS patients. No patient has had aspiration of blood or secretions. Blood pressure is easier to control. There is less chance of bronchospasm at the time of anesthetic emergence and in the immediate postoperative period.
Thus, concerns with MAC of inadequate spontaneous respiration or aspiration of blood that might come down from the sinuses are largely eliminated with general anesthesia. The general anesthetic is also often believed to allow better control over physiological parameters such as blood pressure. No clear-cut advantage of general anesthesia over MAC has been demonstrated,10 but our practice favors the general anesthetic for the reasons mentioned above.
Whatever the anesthetic choice, adequate monitoring is required. Minimally, each patient must be monitored with electrocardiogram, noninvasive blood pressure, pulse oximetry, inhaled oxygen concentration, and exhaled CO2 concentration. In addition, if temperature is not monitored, the ability to monitor temperature must be readily available. These monitoring standards are outlined in the American Society of Anesthesiologists’s Standards, Guidelines and Statements.11 The ability to monitor breath-by-breath major inhalation anesthetic concentration, although not required, certainly adds useful information. Watching the decline of anesthetic concentration on emergence from general anesthesia is helpful to the clinician. For example, if a patient is slow to emerge and the exhaled inhalation anesthetic has reached a concentration near zero, we know to look for other reasons and do not need to speculate about the degree of retained inhalation agent.
FIGURE 24–1 (A,B) Views of the laryngeal mask airway (LMA).
Typically, the drugs used for MAC include a tranquilizer (midazolam, diazepam, lorazepam, etc.) a narcotic (morphine, meperidine, fentanyl, alfentanyl, etc.), and a sedative (almost always propofol). The key is the judicious use of these drugs so that the patient is sedated and calm but easily arousable, breathing adequately, and able to protect his or her own airway.11 We do not have extensive experience with MAC for ESS, but we commonly use it for other elective procedures in this area of the body. Our usual regimen includes midazolam, fentanyl, and propofol in small incremental doses until the patient reaches the desired level of sedation. Then the sedation is maintained with a low dose (25–100 μg/kg/min) of propofol and small intermittent doses of fentanyl (0.5–1.0 mL). Supplemental oxygen is supplied through a nasal cannula that is placed in the mouth. The patient is continually reminded to breathe through his or her mouth. While the anesthesiologist is sedating the patient, the surgeon uses a combination of injected and topical local anesthetics to make the nasal tissue insensitive to the surgical stimulus. Usually 1% lidocaine with diluted epinephrine (1:100,000) is injected into specific sites, and 4% cocaine-soaked pledgets are strategically placed in the nose to produce numbness and vasoconstriction.
The usual principles for any general anesthetic in the head and neck region apply to anesthesia for ESS. After induction of the anesthetic, the patient’s trachea is intubated or an LMA is inserted through the mouth for airway protection and ventilatory support. Induction is accomplished with an ultra-short-acting barbiturate (usually thiopental) or propofol. We prefer propofol because it is eliminated faster. A muscle relaxant facilitates the intubation. Often succinylcholine is used for this purpose, but an intermediate-acting nondepolarizing muscle relaxant (atracurium, cisatracurium, mivacurium, rocuronium, or vecuronium) can be used. If succinylcholine is used for intubation, it usually will need to be followed with a nondepolarizing muscle relaxant for maintenance of the anesthetic. If an LMA is used, no muscle relaxant is required for either insertion of the LMA or maintenance of anesthesia, and the patient is allowed to breathe spontaneously with assistance (if needed) throughout the case.
PEARL
LMA insertion can be accomplished using many different techniques, but the one that works the best for us is to extend the neck as if going to intubate the patient, use a tongue depressor to retract the tongue as far out of the oropharynx as possible, and slide the lubricated, partially inflated LMA into position (Fig. 24–2). Occasionally, the tip of the LMA curves cephalad, and we need to insert a finger into the oropharynx to guide it into position.