Anatomy and Physiology of the Salivary Glands
Rohan R. Walvekar
Bridget C. Loehn
Meghan N. Wilson
The major salivary glands of the head and neck consist of the parotid glands, submandibular glands, and sublingual glands. There are also hundreds to thousands of minor salivary glands located throughout the upper aerodigestive tract concentrated mainly in the buccal, labial, palatal, and lingual regions. The main function of the salivary glands is the production of saliva for lubrication and protection, buffering action and clearance of food, maintenance of tooth integrity, antibacterial activity, taste, and digestion. It is important for a head and neck surgeon to understand the anatomy, embryology, function, and imaging of salivary glands to assist in the diagnosis and surgical management of benign and malignant disease of the salivary gland.
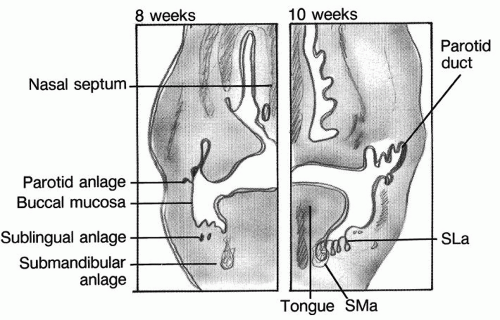
EMBRYOLOGY
The salivary glands share an overall common embryogenesis in that they all develop from outpouchings of oral ectoderm into the surrounding mesenchyme and they have a similar anatomic structure (Fig. 47.1). The major salivary glands develop during the sixth to eighth weeks of embryonic life. The parotid anlagen are the first to develop, followed by the submandibular glands, and then the sublingual glands. The primordia originate at the site of the eventual ductal orifice and the gland develops into an elaborate tubuloacinar system. The parotid gland is unique in that as its epithelial buds are growing and branching, they extend between the divisions of the facial nerve, eventually surrounding the nerve. This phenomenon has clinical and surgical relevance, explaining why neoplastic processes may often extend both superficial and deep to the facial nerve rather than honoring traditional definitions of superficial and deep parotid lobes. During development, all three of the major salivary glands become encapsulated. Although the parotid gland is the first to develop, it is the last to become encapsulated in loose connective tissue. This becomes important in the adult parotid anatomy as the lymphatic system develops prior to the encapsulation of the parotid but after the encapsulation of the submandibular and sublingual glands. Therefore at the completion of embryogenesis, the parotid gland has lymph nodes and lymphatic channels within the capsule whereas the submandibular and sublingual glands do not. This fact has driven recent studies that examined the feasibility of submandibular gland preservation in patients with oral cancer, demonstrating a lack of direct metastasis to the submandibular glands in neck dissection specimens (1,2). The minor salivary glands develop from oral ectoderm and nasopharyngeal endoderm in the 12th week of intrauterine life.
Parotid Gland Anatomy
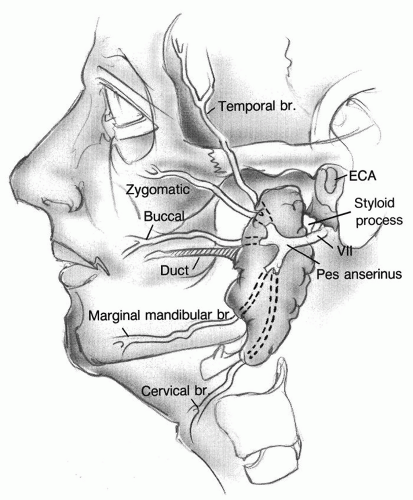
The parotid gland is the largest of the three major salivary glands with an average weight of 25 g. The parotid gland is an irregular, wedge-shaped, unilobular gland found overlying the mandibular ramus and anterior inferior to the external ear (Fig. 47.2). It is located within the parotid space. This space is bound superiorly by the zygomatic arch, posteriorly by the external auditory canal, inferiorly by the styloid process, styloid muscles, internal carotid artery and jugular vein, medially by the lateral parapharyngeal space and laterally by the dermis of the skin. Anteriorly, the parotid gland extends superficial to the masseter muscle. This space not only contains the parotid gland but also the parotid lymphatics, blood vessels, and nerve supply. A small tail of parotid extends posteroinferior toward the mastoid process and overlies the sternocleidomastoid. Histologically, the parotid gland contains purely serous secreting acinar cells. The serous secreting cells are mainly spherical in shape and secrete a protein-rich fluid.
The parotid gland is encapsulated in its own dense connective tissue, which is continuous with the superficial layer of the deep cervical fascia. The parotid fascia consists of a superficial and deep layer. The superficial layer extends from the sternocleidomastoid and masseter muscles to the zygoma. This fascia sends septae into the glandular tissue. These septations make it difficult to separate the parotid gland from its investing fascia. The deep layer extends from the fascia of the posterior belly of the digastric muscle and forms the stylomandibular membrane, which separates the parotid and submandibular glands (Fig. 47.3). Occasionally the parotid tissue can herniate through the stylomandibular ligament and present as a parapharyngeal space mass.
The main parotid duct (Stensen duct) arises from the anterior border of the gland and runs parallel to the zygomatic arch. It is located approximately 1.5 cm below the zygomatic arch. The duct travels superficial to the masseter muscle, then turns 90 degrees and pierces the buccinator muscle to enter the oral cavity at the level of the second maxillary molar. The buccal branch of the facial nerve normally travels along with the parotid duct (Fig. 47.4). The parotid duct is approximately 4 to 6 cm in length. The diameter of the duct is approximately 0.5 to 1.4 mm and the narrowest portion is located at the ostium (3). The parotid duct tends to be more readily amenable to dilation and access. However, its course around the masseter can be difficult to navigate from the perspective of performing endoscopic procedures like salivary endoscopy. This curve has also been termed the “masseteric bend” in sialendoscopy literature (4).
Accessory parotid gland tissue is present in 21% of the population. It is salivary tissue adjacent to Stensen duct that is separate from the main body of the parotid gland (5). The duct of this accessory tissue empties directly into the parotid (Stensen) duct. Its histology is comprised of mucinous acinar glands in addition to the serous acinar gland that dominate in the parotid gland. The accessory parotid gland can be present and may be asymptomatic (Fig. 47.5) or be a site for neoplastic transformation similar to other major salivary glands (6).
The arterial blood supply to the parotid gland is from the external carotid artery. The external carotid artery terminates into two branches (maxillary and superficial temporal artery) in the deep aspect of the parotid gland behind the neck of the mandible. The transverse facial artery, a branch of the superficial temporal artery, supplies the parotid gland, Stensen duct, and the masseter muscle. This artery travels anteriorly between the zygomatic arch and Stensen duct accompanied by the transverse facial vein.
The venous drainage is located in the middle section of the parotid gland, deep to the facial nerve. The venous drainage is provided by the retromandibular (posterior facial) vein. The retromandibular vein, formed by the joining of the superficial temporal vein and the maxillary vein, exits the parotid gland lateral to the carotid artery and joins the postauricular vein to form the external jugular vein, which eventually drains into the internal jugular vein.
The superficial compartment of the parotid gland contains the neural structures including the facial nerve (cranial nerve VII), the great auricular nerve, and the auriculotemporal nerve.
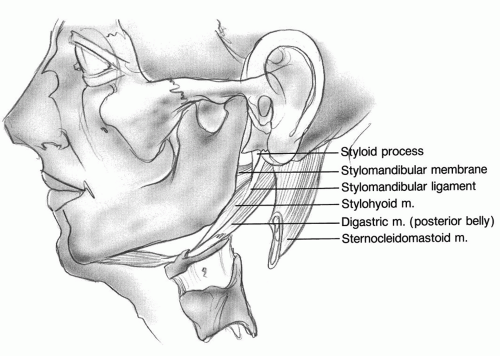 Figure 47.3 Stylomandibular membrane (deep layer of parotid fascia). Herniations of parotid tissue through this membrane can result in a parapharyngeal mass. |
The facial nerve, as previously stated, is intimately associated with the parotid gland. It divides the gland into two surgical zones (superficial and deep lobes). The facial nerve exits the skull base through the stylomastoid foramen. It immediately gives off three motor branches: the nerve to the stylohyoid muscle, the nerve to the postauricular muscle, and the nerve to the posterior belly of the digastric muscle. Once these branches are given off, the nerve turns laterally to enter the posterior aspect of the parotid gland. Approximately 8.56 to 10.20 mm from the stylomastoid foramen, the facial nerve divides at the pes anserinus into the superiorly directed temporofacial and inferiorly directed cervicofacial branches (7). The nerve finally terminates into five branches: temporal, zygomatic, buccal, marginal mandibular, and cervical branches. The number of branches immediately after the pes anserinus and the number of terminal branches are variable dependent on the individual patient. The main trunk bifurcates into two branches at the pes anserinus in 86.7% and into three branches in 13.3%. The branching
pattern of the facial nerve is variable, and communicating or internerve branches are frequently present. Numerous variation patterns have been published. The buccal branch is the most variable and communicates with the zygomatic branch in 62% of cases and the marginal mandibular nerve in nearly 35% (8).
pattern of the facial nerve is variable, and communicating or internerve branches are frequently present. Numerous variation patterns have been published. The buccal branch is the most variable and communicates with the zygomatic branch in 62% of cases and the marginal mandibular nerve in nearly 35% (8).
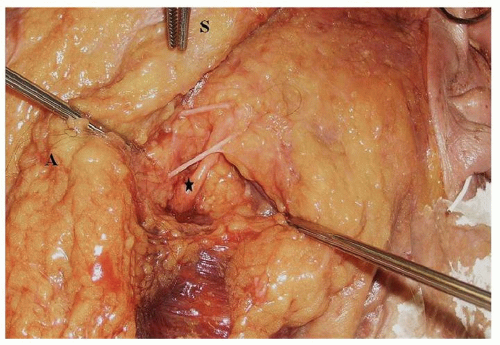 Figure 47.4 Cadaveric dissection showing the relationship of the buccal division of the facial nerve to the Stenson duct (the black star denotes the Stenson duct). |
 Figure 47.5 Axial MRI scan showing accessory left parotid lobe. (Black arrow points to left accessory parotid lobe; asterisk denote right and left parotid glands.) |
During parotidectomy, the localization of the facial nerve is critical. When the normal parotid anatomy is distorted as with a tumor, there are several constant relationships that will aid in finding the facial nerve. The tragal pointer is a projection of conchal cartilage that points toward the main trunk of the facial nerve. The facial nerve lies less than 1 cm medial and inferior to the tragal pointer (5). The nerve can also be found approximately 6 to 8 mm deep to the tympanomastoid suture line at the stylomastoid foramen. The styloid process is another constant landmark and the facial nerve lies on the posterolateral aspect of the styloid process near its base. The facial nerve is also located superior, posterior and deep to the cephalic portion of the posterior belly of the digastric muscle. After the nerve is identified at the stylomastoid foramen, anterograde dissection is required to continue surgical extirpation of the parotid glands. The surgical exposure of the nerve at this stage can be restricted and consequently care must be taken to avoid traction injury to the nerve at this juncture. Once the main divisions of the nerve are exposed, the plane of surgical dissection becomes more obtuse along the direction of the branches of the nerve (Fig. 47.6). Retrograde dissection of the buccal branch and temporal branch can be used to localize the main trunk. The buccal branch usually runs parallel to the parotid duct. The temporal branch can be roughly located along a line extending from the attachment of the ear lobule anterosuperior to a point 1.5 cm above the lateral aspect of the eyebrow (9). If the facial nerve cannot be identified using the above landmarks, a mastoidectomy may be performed and the facial nerve may be located in the mastoid (vertical) segment and thus may be traced to the stylomastoid foramen.
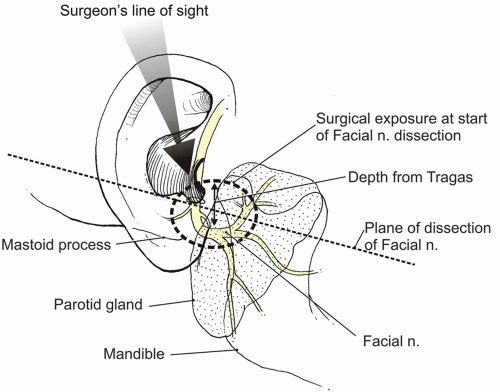 Figure 47.6 Illustrations depicting the depth of nerve at its point of entry into the parotid gland and surgical planes of dissection as compared to surgeon’s line of sight. |
The great auricular nerve (C2, 3), a branch of the cervical plexus passes around the posterior border of the sternocleidomastoid muscle, ascends diagonally across
the sternocleidomastoid muscle onto the parotid gland. It supplies sensation to the skin over the parotid gland, the posterior aspect if the auricle, and an area of skin from the angle of the mandible to the mastoid process. The nerve divides into an anterior and posterior division. This nerve is often damaged or intentionally sacrificed during parotidectomy causing numbness over the earlobe and skin over the parotid gland. Meticulous intraglandular dissection of the nerve can allow the nerve to be preserved if the location of the tumor permits such a dissection (10). Alternatively, in the author’s experience, in most cases the posterior division of the nerve can be preserved avoiding complete anesthesia over the distribution of the nerve.
the sternocleidomastoid muscle onto the parotid gland. It supplies sensation to the skin over the parotid gland, the posterior aspect if the auricle, and an area of skin from the angle of the mandible to the mastoid process. The nerve divides into an anterior and posterior division. This nerve is often damaged or intentionally sacrificed during parotidectomy causing numbness over the earlobe and skin over the parotid gland. Meticulous intraglandular dissection of the nerve can allow the nerve to be preserved if the location of the tumor permits such a dissection (10). Alternatively, in the author’s experience, in most cases the posterior division of the nerve can be preserved avoiding complete anesthesia over the distribution of the nerve.
The auriculotemporal nerve is a branch of the mandibular division of the trigeminal nerve (V3). This nerve exits the skull base via foramen ovale, turns and runs anterior to the external auditory canal, and parallels the superficial temporal vessels. Its functions include supplying sensation to the scalp and carrying postganglionic parasympathetic fibers from the otic ganglion to the parotid gland. The auriculotemporal nerve and the facial nerve are intimately associated as communications between the auriculotemporal nerve and the facial nerve were observed in 93.3% of patients in one study (8).
The salivary glands receive their secretomotor innervation from the parasympathetic and sympathetic nervous systems. The parotid gland receives its parasympathetic stimulation by the glossopharyngeal nerve. The preganglionic parasympathetic fibers originate in the inferior salivatory nucleus, join the glossopharyngeal nerve, course through the lesser superficial petrosal nerve, and then travel through the foramen ovale to synapse in the otic ganglion. The postganglionic fibers then join the auriculotemporal nerve and thus are projected to the parotid tissue. The sympathetic stimulation is by the superior cervical ganglion. Sympathetic fibers begin in the thoracic spinal cord and synapse in the superior cervical ganglion. The postganglionic fibers form a plexus and travel on the external carotid artery to the parotid gland.
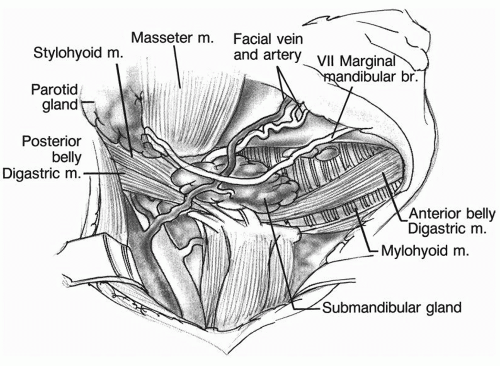 Figure 47.7 The submandibular triangle. Note the relationship of the marginal mandibular nerve to the mandible and facial vessels. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree