It is easy to be overwhelmed when faced with the hundreds of cataloged anomalies of the head and neck region. For any individual defect there may be variation in phenotype, associated anomalies, and cause. To help organize these various disorders, dysmorphologists have grouped them into “syndromes”, “sequences” and “associations” based on our level of understanding of their etiologies. Recently, completion of the human genome project has added a new level of complexity to the study of human malformations by providing a flood of new information about the genetic origins of established syndromes. The article describes the dysmorphologist’s approach to the child with one or more anomalies and provides a glimpse into the future of human genetics.
Dysmorphology
Identifying a child as different or “funny looking” is a useful first step in the approach to anomalies of the head and neck. It is insufficient, however, to stop at this point. The field of dysmorphology has grown, in large part, from an appreciation that defects in development often have repeatable and identifiable patterns . Knowledge of these patterns and an understanding of the developmental events that produce them have made medical genetics a science. Why bother to catalog such anomalies? As is the case with neoplasms or infectious diseases, if the clinician has “seen one of these before,” he or she is more likely to arrive at an accurate diagnosis, to the search for other related defects, and to make useful statements about the future ( Fig. 1 ).
Normality
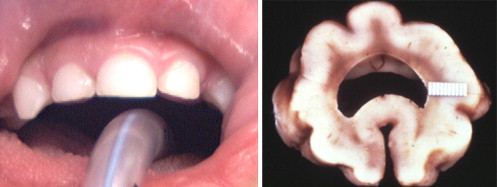
What is normal? We accept a broad range of human variation within the definition of normal. Noses are big and small, straight and curved. By the same token, having no nose at all would be considered an anomaly by almost everyone . Thus, defects in the head and neck can be separated into those that are gross malformations and those that are defects by degree ( Fig. 2 ). It is important, therefore, to define the range of normal and to apply objective parameters to it. An example in the head–neck region is hypertelorism. Measurements of intraorbital distance are cataloged, starting in the fetal period . Measurements for an individual patient can be compared with these charts, and normality defined for any particular age group .

Normality of some other physical properties is more difficult to define. What is intelligence? How many colors should a normal adult perceive? What variations in the shape of the antihelix are acceptable? Students of human development strive to establish useful tests and norms for each of these important characteristics.
Normality
What is normal? We accept a broad range of human variation within the definition of normal. Noses are big and small, straight and curved. By the same token, having no nose at all would be considered an anomaly by almost everyone . Thus, defects in the head and neck can be separated into those that are gross malformations and those that are defects by degree ( Fig. 2 ). It is important, therefore, to define the range of normal and to apply objective parameters to it. An example in the head–neck region is hypertelorism. Measurements of intraorbital distance are cataloged, starting in the fetal period . Measurements for an individual patient can be compared with these charts, and normality defined for any particular age group .
Normality of some other physical properties is more difficult to define. What is intelligence? How many colors should a normal adult perceive? What variations in the shape of the antihelix are acceptable? Students of human development strive to establish useful tests and norms for each of these important characteristics.
Patterns of anomalies
The clinical diagnosis of a malformation is rarely made on the basis of a single defect. Once one has identified a defect, it is important to know what other important or subtle defects might tend to occur in the same individual ( Fig. 3 ). Some of this information comes from the collective experience of observers over the years, and some of it can be reasoned, if one appreciates the genetic and morphogenic processes that lead to the normal formation of individual features. Children with preauricular pits or tags are more likely to be deaf than children without such minor defects . Starting with this basic information, a well-trained clinician knows to test hearing in any child with such a defect. More important, the dysmorphologist is aware of the existence of the branchio-oto-renal syndrome and recognizes that the development of the outer, middle, and inner ears are related ( Fig. 4 ). Armed with such knowledge, he/she can look for the rest of the pattern and, finding it, make informed statements about the child’s future and the probability that related family members or offspring will have the same disorder. Finally, awareness that ear and kidney anomalies occur together in a nonrandom fashion can lead the clinician to diagnose a hidden renal anomaly that might otherwise have been missed .




