Pediatric Ophthalmology
Edited by P. F. Gallin
Thieme Medical Publishers, Inc.
New York ©2000

4

Amblyopia
Amblyopia is defined as a two-Snellen line difference of acuity (best corrected) from one eye to another. According to Duke-Elder,1 amblyopia is classified as
I. Amblyopia ex anopsia (anterior segment)
II. Congenital (organic; posterior segment)
III. Strabismic amblyopia
IV. Anisometropic amblyopia
Predominantly, strabismus and anisometropia (greater than a spherical equivalent of 1.5 diopters in general) are the most frequent causes of amblyopia. Structural anomalies contribute to amblyopia also.
In a nonstrabismic child it is difficult to diagnose amblyopia. In a preliterate child, amblyopia is often inferred from retinoscopy, fixation preference, and an intraocular examination. The determination of fixation preference in an infant is exceedingly difficult to assess, thus requiring judgment from an examiner schooled in assessment of vision in preliterate children.
When a child is able to read a Snellen chart of any type, one can appreciate the large or subtle differences of acuity. When the acuity differences become minimal, it is important that the second or nonseeing eye be evaluated on more than one occasion to determine that these are real lab data. Often children are less cooperative when their second eye is tested. Conversely, they are sometimes skittish when the first or initial eye is examined.
 Etiology
Etiology
The exact etiology of the amblyopia determines the treatment. In the case of structural problems, it is imperative that these anomalies such as a cataract be removed prior to the onset of the amblyopia treatment. In the case of strabismus, it is imperative that the amblyopia be resolved prior to any surgical procedures (with some exceptions). In the case of anisometropia, spectacle correction is necessary to ensure a focused image on the eye that has the greatest refractive error.
Our practical treatment of amblyopia is based on the work of Doctors Hubel and Wiesel, for which they won the Nobel Prize in 1981. Through their work with macaques and kittens they were able to determine that amblyopia is a structural change in the cerebral cortex at a microcellular level. These authors concluded that there is an initial window following birth at which time vision is formed in the occipital cortex in the absence of structural anomalies. If there is asymmetry in the presentation of a clear image to one retina, then on a cellular level the occipital cortex layers correlating with that eye become severely disorganized. If there is bilateral masking of the maculae and thus cerebral cortex, when this mask is removed, the vision in fact can turn on equally and at an excellent (but not perfect) level. When there is asymmetry in the vision beginning from birth and the occlusion is removed from one eye (lid unsutured), there can be reformatting on a microcellular basis of the occipital cells; however, this is never identical to the preferred eye but can yield excellent vision.2–7
There are numerous windows of time in the development of vision. The first window, which determines the onset of vision, is within days and weeks. This is the determining factor in the urgency of congenital cataract extraction. If the vision then goes unopposed for many structural, strabismus, or refractive etiologies, the poor vision will become entrenched within a few months’ time. However, if there is a bilaterally symmetric obstacle such as those listed previously, then the vision in the cortical cells is “suppressed,” and reorganization begins anew when the obstacle is reversed.
The amylogenic window for all children exists from birth to approximately 7.5 to 9 years of age. This end point is not crisp but is the clinically accepted end point at this time.
The basis for amblyopia treatment is to take away vision from the preferred eye and thus make the second eye (poorly seeing eye) work harder. Through the use of this added effort, the cells reorganize in the occipital cortex. This assumes a perfectly focused image on the macula of the poorly seeing eye.
 Treatment
Treatment
Classic (Occlusion)
The classic amblyopia therapy is that of an occlusive patch of which there are two types readily available in the United States, Elastoplast and Coverlet (Fig. 4-1). The initial treatment regimen is for full-time occlusion. This means that the child wears the occluder on a full-time basis during waking hours except for 1 hour per day. The child is patched 1 week per year of life. In the event that the child does not return for examination following this interval, the possibility of occlusion amblyopia occurs. Occlusion amblyopia is an amblyopia that develops in the previously preferred eye due to over-patching the preferred eye such that the poorly seeing eye then becomes the preferred eye. All patients undergoing occlusion therapy must be warned to remove the patch if they miss the follow-up visits. Full-time occlusion has numerous difficulties, most significantly including occlusion amblyopia and cooperation.
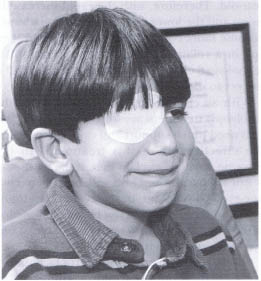
FIGURE 4-1. Occlusive patch on child.
One of the many difficulties in patients who occlude full time is that functionally they cannot see the field in the patched eye. Children are forced to use a relatively nonseeing eye to fulfill their daily tasks. This is quite difficult for children and their families. In addition, at times, the adhesive from the patch can become quite irritating to the skin, thus requiring either cessation of patching or at times medical treatment to excoriated skin.
However, full-time occlusion in almost all amblyopia treatment is the initial treatment of choice. This treatment will yield the largest improvement in acuity in the smallest time interval due to the fact that the less preferred eye must be used to function on a full-time basis. It is quite extraordinary that the occipital cortex is plastic up until the advanced age of at least 7 ½ to 9 years of age.
For example, a 6-month-old infant who has a fixation preference due to an esotropia will be patched only 3 days prior to the next visit for fear of an occlusion amblyopia. The fixation in young children is extraordinarily plastic such that fixation can change within hours, thus requiring short-term follow-up. A baby’s visual demands are less significant than those of a 5-year-old. Therefore, with the rapid increase in vision and the lower visual demands, a baby will become more comfortable with occlusion therapy in a relatively short interval than will a school-aged child who is learning to read and is subject to social comments (Fig. 4-2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


