5 Allergic Eye Diseases, Episcleritis and Scleritis
ALLERGIC EYE DISEASE
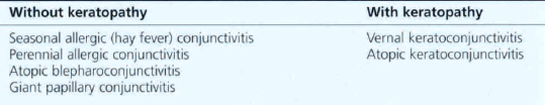
Allergic eye disease in its various forms is a common cause of ocular morbidity in both primary care and specialist practice. The external eye is under constant immunological challenge from a wide variety of substances; this may lead to the development of one of many conditions that can be loosely grouped as ‘allergic eye disease’. The chief factors determining the outcome of such challenges are the severity and duration of the antigenic load and the immunological status of the individual. Local or systemic immune mechanisms may be involved to produce immediate hypersensitivity, complement-mediated or delayed hypersensitivity reactions. The spectrum of allergic conjunctivitis (Table 5.1) ranges from mild self-limiting seasonal conjunctivitis to atopic keratoconjunctivis in which vision is threatened by corneal vascularization, herpetic epithelial infection and the long-term complications of topical corticosteroid therapy. Although patients complain of red, sore and discharging eyes, itchiness is the characteristic symptom of allergic eye disease. Patients also have an increased risk of keratoconus and atopic cataract. Increased levels of IgE and eosinophils are found in the conjunctiva and a wide range of inflammatory mediators have been shown to be involved in the pathogenesis.
IMMEDIATE HYPERSENSITIVITY REACTIONS

Fig. 5.1 Acute periorbital oedema is a common manifestation of immediate hypersensitivity and appears within minutes of exposure. It may follow the systemic administration of antigen in a sensitized individual such as the ingestion of foods or drugs. The reaction is frequently associated with high titres of circulating IgE antibody, being mediated by the release of histamine and other pharmacologically active substances from mast cells in the skin and mucosal tissues. It usually produces symmetrical bilateral lid oedema which may also be accompanied by conjunctival chemosis and urticarial skin rashes. The onset is rapid but the signs usually improve within a few hours. Acute unilateral signs may result from local inoculation and histamine release in the skin, as in this patient where the reaction followed an insect bite.

Fig. 5.2 Acute conjunctival chemosis may occur in the absence of lid swelling as an immediate hypersensitivity response to local inoculation of antigenic substances (frequently pollens) directly on to the conjunctiva of a sensitized individual. The level of response depends on the degree of previous sensitization and the dose of antigen. In this patient, although both conjunctiva are chemotic and slightly hyperaemic, the signs are more pronounced in the left eye.
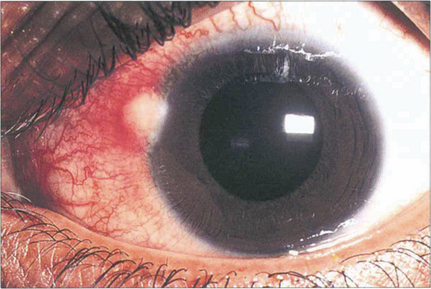
Fig. 5.3 Phlyctens are inflammatory nodules usually seen on the nasal limbus with an associated hyperaemia. They are bilateral and are usually seen in children and young adults. Phlyctens represent a lymphocyte cell-mediated response in a previously sensitized individual. They are associated with a variety of antigens; staphlococci are now the commonest cause, but in the past the main cause was tuberculosis.
ALLERGIC CONJUNCTIVITIS
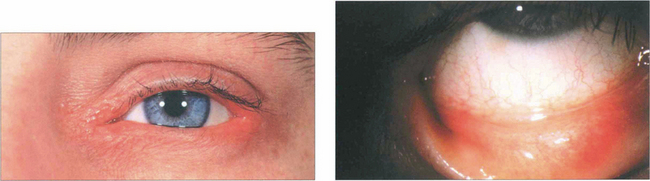
Fig. 5.4 Atopic blepharoconjunctivitis is typified by thickening of eyelid and periocular skin. Conjunctival inflammation is moderate and keratopathy is absent.
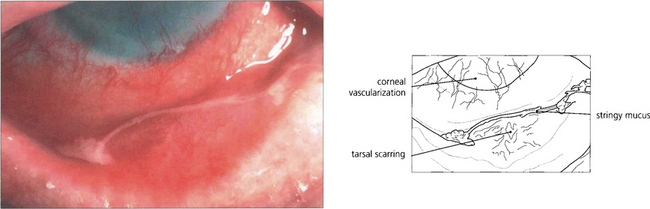
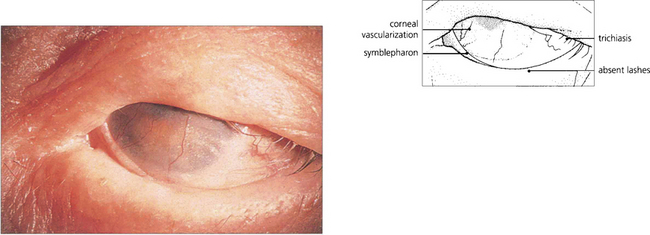
Fig. 5.5 Atopic keratoconjunctivitis is uncommon and is usually seen in young men with atopic dermatitis and a history of childhood eczema. The ocular changes are seen in early adult life; they are bilateral, symmetrical and persistent for many years. The conjunctival changes carry a significant risk of sight-threatening complications which include corneal vascularization, herpes simplex viral keratitis and steroid-induced glaucoma. Cicatrizing conjunctivitis and fornix shortening results from progressive subepithelial scarring.
VERNAL KERATOCONJUNCTIVITIS

Fig. 5.6 This boy, who suffers from VKC, shows a typical eczematous rash on his forehead and cheeks. There is an associated slight bilateral ptosis reflecting the chronic inflammation on the upper tarsal conjunctiva.
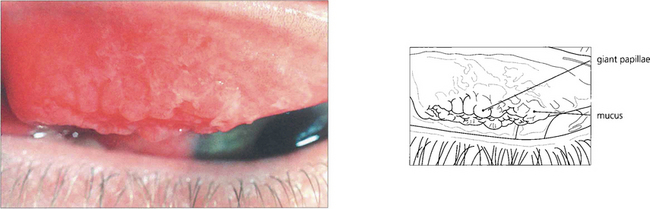
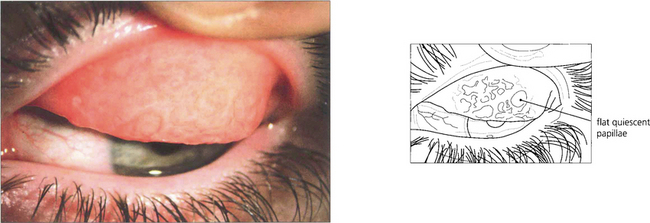
Fig. 5.7 Giant papillae on the upper tarsus, typically described as having a ‘cobblestone’ appearance, are the hallmark of VKC. Although these papillae persist during quiescent phases they become swollen and infiltrated by oedema and inflammatory cells with abundant abnormal mucus both on the surface and in the crevices between the papillae when the disease becomes active, as in this example.
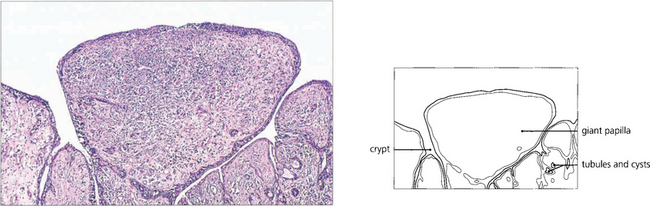
Fig. 5.9 A histological section of VKC shows typical papillae with epithelial downgrowth to form tubules and cysts. The papillae have a loose stroma in which inflammatory cells are seen. Eosinophils and basophils are present in large numbers during the active phase of the disease.
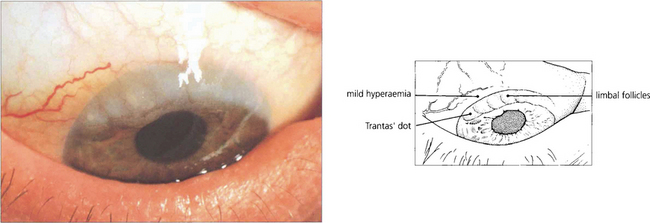
Fig. 5.10 Limbal follicles may occur in VKC and are seen more commonly in black patients in the absence of marked tarsal papillae. This is sometimes known as the ‘limbal’ form of the disease. These limbal lesions are heavily infiltrated with inflammatory cells and appear as greyish, gelatinous swellings, especially around the superior limbus. The blood vessels are not unduly prominent and no mucus is visible.
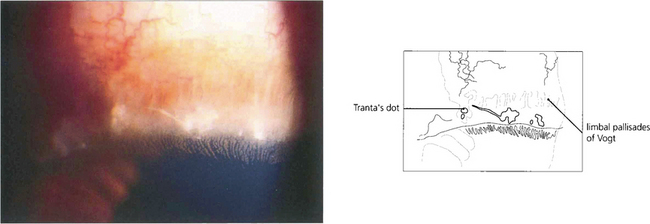
Fig. 5.11 Trantas’ dots are a feature of VKC. They are small, white, elevated, epithelial lesions seen on the limbal lesions at the superior limbus and contain eosinophils. In this example they are associated with a greyish corneal infiltrate.
By courtesy of Professor R J Buckley.
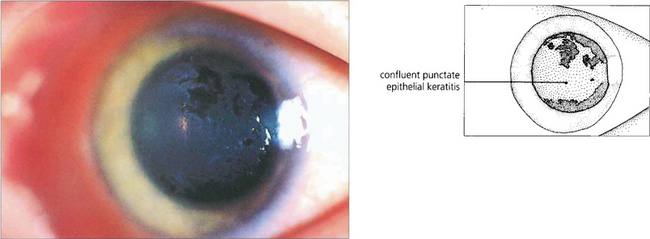
Fig. 5.12 This patient illustrates the early corneal changes seen in vernal disease. There is a fine punctate epithelial keratopathy consisting of fine grey dots which has become confluent in some areas. Eosinophilic major basic protein from disrupted eosinophils is cytotoxic and thought to play a major role in vernal keratopathy.
By courtesy of Professor R J Buckley.
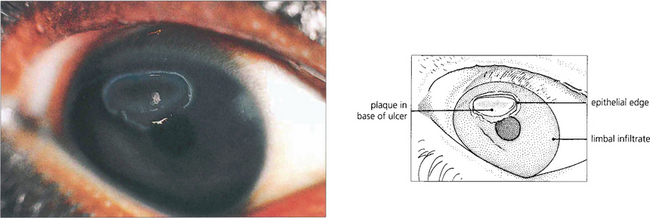
Fig. 5.13 A vernal ulcer characteristically develops in the upper half of the cornea during active phases of tarsal disease and is shown here stained with fluorescein. The edge of the ulcer is surrounded by whitish, heaped-up epithelium. The base is composed of abnormal mucus that is deposited with fibrin and other serum constituents as a grey plaque. When established, this plaque prevents healing from occurring. An area of superficial corneal infiltration can be seen nearer the limbus on the nasal side of the cornea.
By courtesy of Professor R J Buckley.
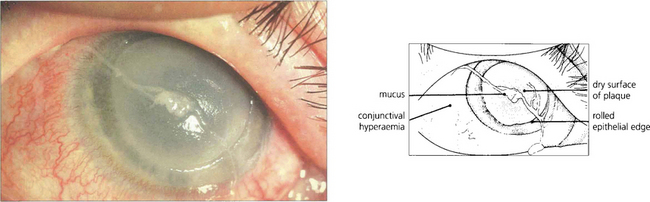
Fig. 5.14 This is a more severe example of a vernal ulcer showing a large area of central ulceration with established plaque formation. This image illustrates the nonwetting properties of the plaque and the raised epithelial edge, which is indicative of poor healing in the presence of plaque. Peripheral to the ulcer, the cornea is relatively clear although corneal vascularization from the limbus has commenced. The conjunctiva is hyperaemic and a strand of typically ‘stringy’ mucus lies on the surface of the eye.
GIANT PAPILLARY CONJUNCTIVITIS
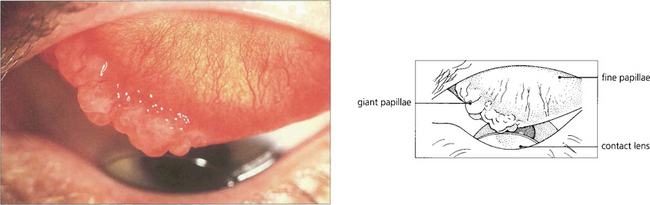
Fig. 5.15 Giant papillary conjunctivitis is a chronic condition affecting the upper tarsal conjunctiva; it is caused by mechanical irritation. The condition is seen, for example, in patients wearing contact lenses, ocular prostheses or in association with protruding nylon suture ends following corneal or cataract surgery. Patients complain of itching, ocular discomfort and a stringy discharge. The aetiology appears to be mast cell degranulation initiated by mechanical trauma. In this example, a hard contact lens has produced giant papillae at the medial end of the upper border of the tarsus with a fine papillary reaction elsewhere. The condition is clinically distinguishable from vernal conjunctivitis by the lack of changes elsewhere in the conjunctiva, absence of an atopic history, and the presence of an associated foreign body. The conjunctival changes resolve with removal of the irritating stimulus.
OCULOCUTANEOUS CICATRICIAL DISORDERS
OCULAR CICATRICIAL PEMPHIGOID
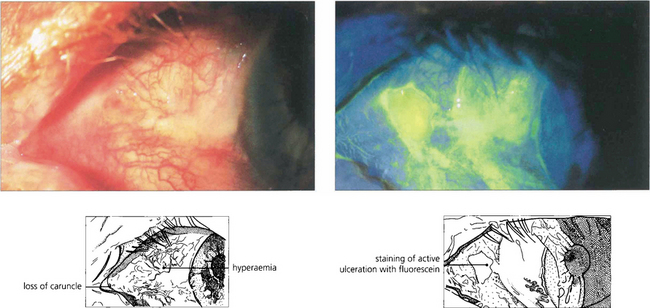
Fig. 5.16 Ulceration of the conjunctiva in active mucous membrane pemphigoid is clearly delineated in this case following instillation of fluorescein.
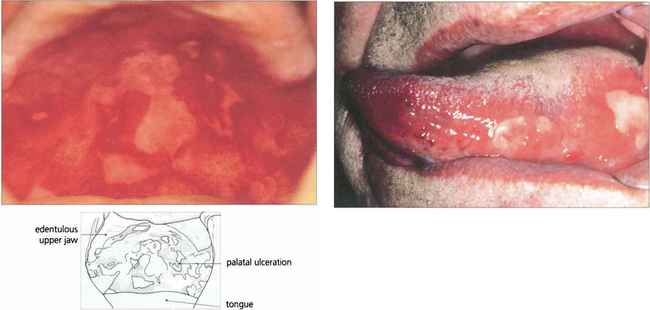
Fig. 5.17 Extensive palatal ulceration is visible in this edentulous patient (left). The painful mouth ulcers had been erroneously attributed by the patient to poorly fitting dentures. Buccal mucous membrane pemphigoid (right) is also characterized by tongue involvement, as in this patient in whom blisters are seen alongside sloughing ulcers, which indicate the site of a previous blister.
By courtesy of Dr F M Tatnall.
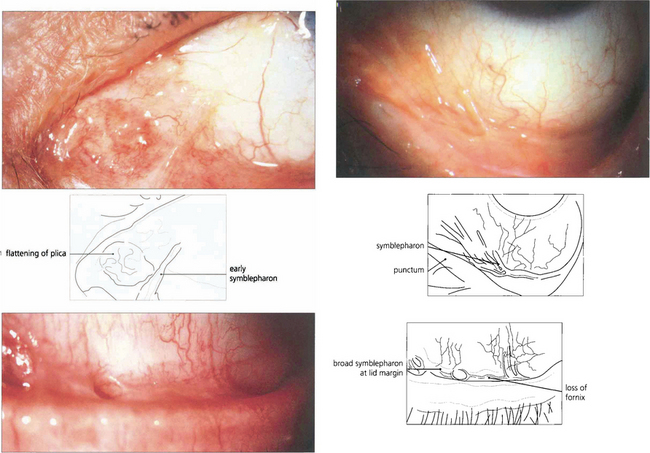
Fig. 5.18 In early pemphigoid, conjunctival cicatrization usually obliterates the caruncle (top left), producing progressive loss of the fornices and symblepharon formation. This example (top right) shows symblepharon formation in early disease which has been arrested by therapy. Inexorable progression to late disease is associated with scarring that almost obliterates the inferior fornix (bottom left).