History
The history of intubation is much more recent than that of tracheotomy. Up until the 19th century, tracheotomy, although considered to be dangerous, was also the most reliable method of achieving tracheal intubation.
The human glottis was first viewed in 1854 by Manuel Garcia, a Spanish vocal pedagogue, with a tool he developed using two mirrors and the sun as an external light source (
1,
2).
In 1858, a Parisian pediatrician, Eugene Bouchut, reported on a small straight metal tube he had developed that could be advanced into the larynx. He used this new nonsurgical orotracheal intubation device to bypass laryngeal obstruction resulting from diphtheria in seven cases. He went on to develop a set of tubes that could be used as an alternative to tracheotomy for cases of diphtheria, despite severe criticism from his colleague Armand Trousseau (
3).
In 1878, Wilhelm Hack of Freiburg published two papers describing the use of nonsurgical orotracheal intubation (a) in the removal of vocal fold polyps and (b) to secure the airway in a patient with acute glottic edema (
4). Visualization of the glottis had been indirect, through the use of mirrors, until 1895 when Alfred Kirstein performed the first direct laryngoscopy, using a modified esophagoscope he called an “autoscope” (
5).
In 1913, Chevalier Jackson developed a new laryngoscope. It included a sliding removable portion for introduction of an endotracheal (ET) tube or bronchoscope as well as a light source at its distal tip (
6). In the same year, Henry Janeway, an American anesthetist, designed a laryngoscope with several modifications specifically for tracheal intubation. His goal was to deliver volatile anesthetics through direct intratracheal insufflation. The intubating laryngoscope he developed had batteries within the handle to power the distal light source, a notched blade for keeping the tracheal tube midline during intubation and a slight curve at the distal tip of the blade. His work is largely credited with the subsequent incorporation of direct laryngoscopy and tracheal intubation into the specialty of anesthesia (
7).
Subsequent noteworthy contributions included the work of Sir Ivan Whiteside Magill, who introduced the technique of awake blind nasotracheal intubation. The Magill forceps he designed for this purpose continue to be widely used in many hospitals across North America (
8,
9). In 1943, Sir Robert MacIntosh developed the Macintosh curved laryngoscope, which has withstood the test of time as the most popular laryngoscope blade for orotracheal intubation (
10). MacIntosh also developed the precursor to the current ET tube introducer (often referred to as a “stylet”), used for difficult intubations.
Orotracheal Intubation
The most widely used route for intubation is orotracheal, in which an ET tube is passed through the mouth and vocal folds into the trachea. It is the simplest technique and that with which anesthetists and critical care physicians have the greatest experience and familiarity. It is appropriate for many operative otolaryngology cases including sinonasal and otologic procedures. It may also be used
for parotidectomy, excision of neck masses, and neck dissections provided the tube is secured away from the surgical side and access to the oral cavity is not required. Orotracheal intubation may be accomplished blindly or with the help of fiberoptic scopes. In the majority of cases, however, a rigid curved MacIntosh laryngoscope is used to facilitate the intubation.
Prior to initiating the intubation, the patient should be positioned with the neck slightly flexed on the chest and the head slightly extended on the neck. The patient should be preoxygenated by delivering O2 through a well-fitted mask. The pharynx and oral cavity should be thoroughly suctioned. The right-handed physician stands at the head of the bed, and holds the MacIntosh laryngoscope in the left hand. The right hand gently opens the mouth, being careful not to impale the lips on the teeth, and the left hand introduces the laryngoscope into the right side of the mouth, displacing the tongue over to the left as the tip is advanced into the vallecula. The larynx is lifted anteriorly to expose the glottis. The ET tube, held in the right hand, is advanced into and through the glottis. Pressure on the cricoid cartilage may be used to facilitate intubation in an anteriorly positioned larynx and has the added advantage of decreasing the risk of aspiration by closing the opening to the esophagus. Following intubation, air entry into both lungs is verified and the tube is secured in position with tapes.
In difficult cases where the first few intubation attempts fail, a different approach should be considered. This may include using intubation aids such as the GlideScope, or switching to a different technique altogether, such as intubation over a flexible fiberoptic bronchoscope.
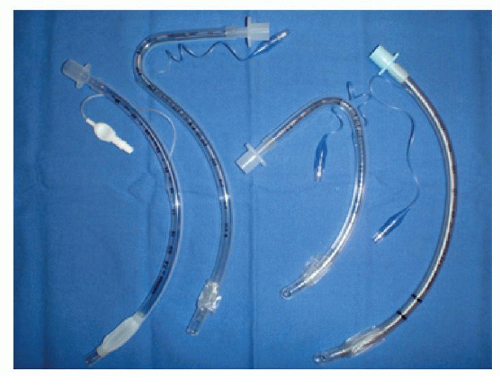
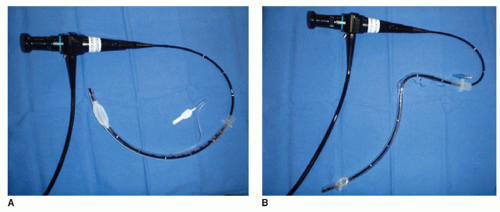
In patients with limited mouth opening, or a narrow airway from whatever reason, awake intubation over a flexible fiberoptic bronchoscope (
Fig. 64.3) provides direct visualization of the glottis and adds a measure of safety. This technique is one of the cornerstones of difficult airway management. Patient comfort is greatly improved with good topical anesthesia of the oral cavity and pharynx and the addition of a superior laryngeal nerve block. Use of an oral airway prevents biting on the ET tube and bronchoscope. Flexible fiberoptic intubation is very useful in cases of laryngeal edema, deep neck space infections, laryngeal papillomatosis, and other neoplasms.
Nasotracheal Intubation
Nasotracheal intubation is another means by which the airway can be protected. It is very useful and provides unhindered access for major head and neck oncologic procedures involving the oral cavity and oropharynx. It may also be used when orotracheal intubation is not possible or otherwise contraindicated. Nasotracheal intubation is
best used for short-term airway protection because of the high incidence of sinusitis, serous otitis media, acute otitis media, and the risk of alar necrosis associated with the more prolonged use of these tubes. It is contraindicated in patients with midface fractures involving the cribriform plate or fovea ethmoidalis because of the risk of entering the brain.
Nasotracheal intubation may be performed blindly, or with the use of rigid or flexible laryngoscopes. Retrograde techniques are also described but are beyond the scope of this chapter.
In the awake patient, nasotracheal intubation is better tolerated than orotracheal intubation. Adequate preparation of the patient is a wise investment in time and will ensure a smooth procedure. A quick look at the nose with a nasal speculum will help identify septal deviations or other anatomic abnormalities that may interfere with the intubation. Good topical anesthesia and vasoconstriction can be achieved by packing the nose with cotton wool impregnated with lidocaine and a decongestant. Alternatively, topical sprays may be used. Topical anesthesia of the pharynx can be obtained by using lidocaine which is either gargled or nebulized. A superior laryngeal nerve block can also be a helpful adjunct. With good topical anesthesia and vasoconstriction, the nasal cavity can be dilated with progressively larger nasal “trumpets.” Ideally the tube should be warmed prior to use to make it more pliable. The warmed, lubricated nasotracheal tube is inserted into the nasal cavity and advanced to the pharynx. At this point, an intubating laryngoscope in the left hand is placed in the right side of the oral cavity and advanced to the vallecula. The tip of the nasotracheal tube, visible on the posterior pharyngeal wall, is grasped with a Magill forceps held in the right hand, and advanced through the glottis. Good air entry to both lungs is verified, and the tube is secured.
When a difficult intubation is anticipated, fiberoptic nasotracheal intubation (
Fig. 64.3) is a good choice. It is an extremely important and successful technique in patients with difficult airways. In particular, it should be considered in patients with limited neck mobility, limited mouth opening, and a short thyromental space. Intubating patients having received prior radiotherapy or surgery to the head and neck can be extraordinarily difficult. In these cases, fiberoptic nasotracheal intubation is likely to be successful, and is especially attractive because it can be performed on the awake, spontaneously breathing patient. The nose and upper airway are prepared with topical anesthesia as previously described. The nasotracheal tube is threaded over the fiberoptic bronchoscope. A size 7 ET tube is the smallest size that will accommodate an adult bronchoscope. A pediatric bronchoscope must be used with size 6 or 6.5 ET tubes. The bronchoscope is introduced into the nose and advanced through the glottis. The nasotracheal tube then follows over the bronchoscope down through the glottis and into the trachea.
Blind nasotracheal intubation is a rarely used “rescue technique” when advancing the tube with the help of a laryngoscope or when fiberoptic intubation or orotracheal intubation is not possible. Patients must be breathing spontaneously. Topical anesthesia is used as much as the situation permits. The tube is introduced through the nose, and advanced into the hypopharynx, with the operator listening for breath sounds as the tube approaches the glottis. The tube is advanced through the glottis just as the next inspiration is begun. Air entry is verified, and the tube is secured. Tips to facilitate passage through the glottis include external pressure on the neck and use of a stylet through the ET tube after it has passed through the nasopharynx. It must be emphasized that this technique is difficult, requires skill and experience, and is associated with higher complication rates than other techniques.
Intubation Aids in the Difficult Airway
In difficult cases where the first few intubation attempts fail, a different approach should be considered. This may include using intubation aids (
Table 64.6) such as the GlideScope, or switching to a different technique altogether, such as intubation over a flexible fiberoptic bronchoscope. Repeatedly attempting to intubate orotracheally after a few failed attempts may lead to airway edema, trauma, and bleeding, rendering both visualization and ventilation by any means difficult. What started as a routine intubation becomes a potentially life-threatening emergency.
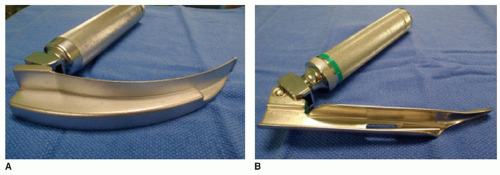
The most frequently used intubating instrument is the MacIntosh laryngoscope (
Fig. 64.4) with the curved blade. This laryngoscope, in its original design, is intended to be held in the left hand. A mirror image of the MacIntosh blade is available for left-handed operators to hold in the right hand leaving the dominant hand for intubation. It is introduced into the left side of the mouth and may also be used in patients with right-sided facial abnormalities or injuries. The English MacIntosh laryngoscope has become the preferred instrument in many centers, because of the continuous curve along the entire length of the blade, and the distal extension of the vertical step and flange. Considered together, these modifications provide a better view of the glottis in many cases. A very large number of subtly modified curved blades, all with intended specific uses, have also been developed (
11).
An impressive variety of straight blades also exists, of which one of the earliest and still most commonly used is the Miller laryngoscope blade (
Fig. 64.4). It is straight, with a gradual curve 5 cm from its narrow tip, and a smaller vertical step compared to the MacIntosh blade. Straight blades are intended to “entrap” and lift the epiglottis, in contrast to the curved blades. Straight blades are especially useful in patients with limited mouth opening as is often the case in previously operated or radiated necks. In these situations, the slimmer blade fits more easily between the teeth, and the distal curved tip allows visualization of the laryngeal inlet. Because the space for maneuvering the ET tube is limited with this type of blade, use of a stylet is recommended (
11).
A number of stylets are available to facilitate intubation. They are long, thin, malleable devices that are inserted into ET tubes and bent or adjusted to a desired shape and curvature. They may be entirely within or extend beyond the ET tube. Some even have a small light at the distal end. The curve of the ET tube afforded by the stylet is helpful when the larynx rests in an anterior position.
The occasional failure of direct laryngoscopy to provide an adequate view for tracheal intubation in the difficult airway led to the development of alternative devices such as the lighted stylet, and a number of indirect fiberoptic viewing laryngoscopes, such as the fiberscope, Bullard scope, Upsher scope, and the WuScope. A detailed discussion of each of these devices is beyond the scope of this chapter. Though these devices can be effective alternatives to direct laryngoscopy, they each have certain limitations, and none of them is effective under all circumstances. One important limitation commonly associated with these devices is fogging of the lens.
The introduction of digital technology has led to the development of several video laryngoscopes designed to facilitate tracheal intubation. The GlideScope emerged in 1991 as the first of several similar devices. The GlideScope incorporates a high-resolution digital camera, which is connected by a video cable to a high-resolution light crystal display monitor (
Fig. 64.5). The high degree of success in intubating difficult airways with the GlideScope is the result of five special features. (a) The sharp 60-degree angulation of the blade reduces the need for displacing the tongue anteriorly, thereby improving the view of the glottis. (b) Instead of being at the tip of the blade, the CMOS APS digital camera is located at the point of angulation of the blade, providing a better view of the field in
front of the camera. (c) The recessed position of the video camera shields it from blood and secretions that might otherwise obstruct the view. (d) The video camera has a relatively wide viewing angle of 50 degrees. (e) The incorporated heated lens helps prevent troublesome fogging of the lens. The blade of the GlideScope is introduced as for a MacIntosh blade, and advanced through the oropharynx with the operator viewing the procedure on the monitor. When the optimal view is achieved, the ET tube is introduced and guided into the larynx, with the help of the image from the monitor. The use of a stylet precurved at approximately 60 degrees facilitates access to the glottic opening.
The GlideScope has been shown to improve laryngeal views compared with direct laryngoscopy with high success rates of intubation in normal airways, following failed direct laryngoscopy, and in predicted difficult airways (
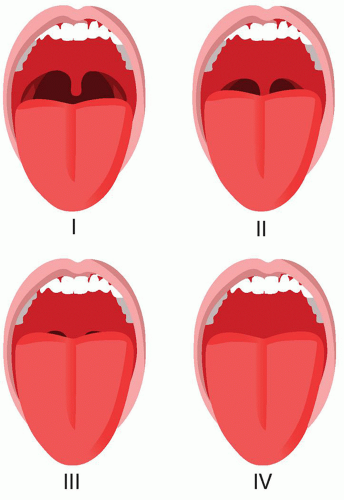
12). In the latter situation, the success of the GlideScope is approximately 92% on the first attempt, and increases from 96% to 100% after more than one attempt. In contrast, increased laryngoscopy attempts are associated with increased morbidity. The most important predictors for failure with the GlideScope include a thyromental distance of less than 6 cm and abnormal neck anatomy such as a neck mass or history of prior irradiation. Important predictors of failure for direct laryngoscopy include the combination of a high Mallampati score and reduced thyromental distance, as well as abnormal neck anatomy (
12). This highlights the importance of careful preoperative patient assessment, and discussion between the anesthesiologist and surgeon to come up with a thoughtful plan that includes alternative techniques such as flexible fiberoptic intubation.
In summary, there exists a large and ever-expanding array of intubating aids and devices for management of the difficult airway. Although each has its place and utility, it should be emphasized that fiberoptic orotracheal or nasotracheal intubation remains a cornerstone in the management of the patient with a difficult airway.
The Hunsaker Tube and Jet Ventilation in Microlaryngeal Surgery
Microlaryngeal surgery involves sharing the airway. A balance must be achieved between airway control and ventilation and the need for adequate laryngeal visualization and exposure.
In 1967, Sanders introduced jet ventilation for use during rigid bronchoscopy (
13). In the 1970s, the concept was adapted for use in microlaryngeal surgery as a means of providing adequate ventilation and maximizing exposure. The technique involves positioning and suspending a laryngoscope to expose the glottis. An injector cannula, tightened to the laryngoscope, allows for the high-pressure delivery of air from above the vocal folds. Exhalation is passive, and requires an unobstructed airway. The technique offers excellent exposure of the larynx at the expense of airway control. The technology has been further modified for supraglottic, subglottic, and transtracheal jet ventilation.
Several tubes have been developed for subglottic ventilation, but their use was limited by problems such as misalignment, inadequate ventilation, inability to monitor airway pressures, and the risk of airway fires with laser use.
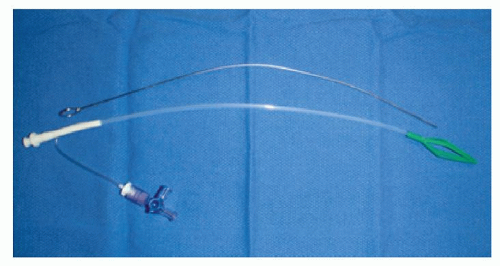
In 1994, Hunsaker introduced a special laser-safe subglottic tube designed specifically for microlaryngeal surgery (
14). Airway pressures and end-tidal CO2 could be monitored through the tube that was attached to a dedicated jet ventilator.
The Hunsaker Mon-Jet tube offers excellent laryngeal visualization and anesthetic safety. It is very versatile and can be used in patients with comorbidities, obesity, and difficult airways (
Table 64.7). It provides excellent laryngeal exposure for a wide range of endolaryngeal procedures using laser, cold steel, or the microdebrider (
15,
16). When used with the laser, it is important to keep oxygen concentrations as close to room air as possible in order to prevent airway fires. In addition, the subglottic position minimizes vocal fold movement during surgery.
The tube itself is 35.5 cm long with an inner diameter of 2.7 mm and an outer diameter of 4.3 mm. Because it is made with a nonflammable fluoroplastic material, it can be safely used with lasers. A metal stylet adds some rigidity to the tube, thereby facilitating intubation. The green basket at the end of the tube helps center the tube within the trachea, and prevents the jet port from coming into direct contact with the mucosa (
Fig. 64.6). There is a 1-mm port for monitoring airway pressures and end-tidal CO2 that opens 3.2 cm above the jet port.
The intubation technique is the same as for orotracheal intubation with a MacIntosh laryngoscope. Once in proper
position, the jet port and monitoring port of the tube are attached to the jet ventilator. An automated jet ventilator is preferred because of the automatic “shut-off” if airway pressures exceed preset limits. The tube should be secured at the corner of the mouth and supported in order to avoid kinking. When the laryngoscope is not in position or the patient’s mouth is closed, an oral airway should be used to allow passive exhalation.
Complications from this technique (
Table 64.8) are seen in less than 2% of cases and consist mostly of hypoxia and/or hypercarbia and rare bleeding down the trachea from the surgical procedure. In all these cases, the Hunsaker may be exchanged for a laser-safe ET tube. Appropriately securing the tube is important to avoid kinking. Barotrauma can be largely prevented with an automated jet ventilator (
16).
The Laryngeal Mask Airway
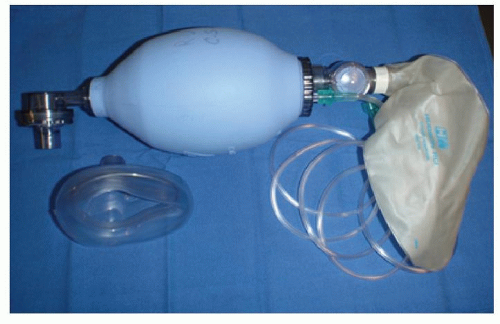
The laryngeal mask airway (LMA) was developed in the 1980s by Dr. Archie Brain as a supraglottic airway device that could be used as an alternative to (a) the more invasive ET intubation, or (b) face-mask ventilation, which is difficult to control. The LMA consists of an inflatable mask attached to a tube that exits through the mouth and can be connected to a ventilator (
Fig. 64.7). The mask contours the periglottic tissues while occupying the hypopharyngeal space. Once inflated, it forms a seal above the glottis in contrast to an ET tube, which forms a seal within the trachea. It requires some training, but is relatively easy to insert, can be used blindly without accessory instruments, and is associated with infrequent complications. An important limitation is that it does not protect against abdominal contents and aspiration. Many modifications of the original device have emerged to adapt to particular clinical situations and expand the indications for use. The LMA, or one of its modifications, can be used in the following situations: (a) as a routine airway or ventilation device, (b) in emergency cases with a “cannot intubate, cannot ventilate” scenario, and (c) with the modified LMA Fastrach, as a conduit for ET intubation (
17).
The original device, the “LMA Classic,” is useful for short, elective, nonotolaryngology cases requiring general anesthesia in the supine position. Because a fiberoptic endoscope can easily be passed through the LMA, it is useful in otolaryngology for diagnostic evaluation of the larynx and during percutaneous tracheotomy. The LMA Classic has also been shown to be very useful in the emergency or nonemergency management of patients with difficult airways. Examples include patients with the following conditions: (a) cervical spine immobility or instability; (b) morbid obesity; (c) micrognathia; (d) congenital syndromes such as Treacher-Collins, Pierre-Robin, and Down syndrome; and (e) unexpected failed intubation with difficult face-mask ventilation (
Table 64.9). Indeed, the LMA has been incorporated into the “Practice Guidelines for the Management of the Difficult Airway” by the American Society of Anesthesia (ASA) Task Force on Management of the Difficult Airway (
17).
A modified version, the intubating LMA Fastrach, was introduced in 1997 and is intended to facilitate blind or fiberoptically guided ET intubation in difficult airways such as C-spine injuries, where head position must remain neutral (
18). It consists of a hollow 13-mm stainless steel tube connected distally to the laryngeal mask. Proximally, a handle helps with insertion and placement. Once it is positioned, a special ET tube can be advanced through the
lumen into the trachea either blindly or over a fiberoptic bronchoscope. The intubating LMA Fastrach is a well-recognized “rescue device” for difficult airways. The C-Trach represents an additional modification with a camera integrated into the LMA, allowing the operator to visualize the ET tube being introduced through the glottis (
18).
Complications of Intubation
Many if not most complications are preventable with careful planning, selection of the appropriate intubation technique, and attention to technical detail. Not surprisingly, complications are much more frequent following difficult or traumatic intubations (
Table 64.10).
Nasal trauma may occur during nasotracheal intubation with possible injury to the mucosa, septum, turbinates, and adenoids. Nasotracheal tubes kept in situ postoperatively increase the risk of nasal alar injury, sinusitis, and otitis media. Long-term sequelae include nasal synechia as well as scarring and distortion of the nasal tip and/or ala. Although some epistaxis is common with nasotracheal intubation, it is usually self-limited. Nasal trauma can be minimized by maximally decongesting the nose, using nasal trumpets for dilatation, and warming and lubricating the nasotracheal tube.
Lip trauma usually occurs on the right upper lip as a result of inattentive laryngoscopy during intubation. It is usually self-limited and requires only comfort measures.
Dental injuries occur in approximately 1 in 4,500 cases and usually involve the maxillary central incisors. These injuries are most common in young children, in patients with preexisting periodontal disease, and in cases where intubation is difficult. Chipped or cracked teeth should be located and removed to prevent tooth aspiration.
Macroglossia, or massive tongue swelling, has been reported, and is thought to result from venous and lymphatic obstruction of the tongue. It is associated with prolonged procedures and compression of the tongue by the ET tube. Less commonly, it may be seen with angiotensinconverting enzymes. In extreme cases the airway may need to be secured with a long nasal trumpet or nasotracheal tube.
Mucosal injury to all areas of the oral cavity and pharynx is possible and may occur from the laryngoscope, oral airway, ET tube or any other device that is used. Up to 40% of patients complain of sore throat following intubation, with even larger numbers in cases of traumatic intubation. Fortunately, most symptoms resolve in 24 to 48 hours.
Laryngeal trauma from intubation may occur in up to 6% of cases and is most likely following traumatic intubation. Injuries may include vocal fold lacerations or hematoma, arytenoid dislocation or subluxation, vocal fold paralysis, and granuloma formation. Use of large tubes, particularly in females, results in tissue ulceration of the posterior larynx and increases the risk of posterior glottic stenosis. The risk is even greater in agitated patients with nasogastric tubes and gastroesophageal reflux.
Tracheal trauma may be related to several factors. An overinflated cuff that exceeds capillary perfusion pressures
results in local tissue hypoxia, necrosis, and eventual healing with malacia or stenosis. Use of large ET tubes, especially in females, may similarly result in stenosis. Intubating stylets, tube exchangers, and malpositioned tubes may also result in tracheal injury. In young children, edema in the subglottic area following extubation increases airway resistance and may result in croup-like symptoms.
Bronchial intubation, especially of the right mainstem bronchus, is relatively common and may manifest as absence of breath sounds on the left side and asymmetric chest expansion. It is even more common in children and may be undetected until hypoxia, atelectasis, or even pulmonary edema further complicate the situation.
Inadvertent esophageal intubation is not uncommon, and, provided it is recognized, can be quickly rectified without adverse effects such as hypoxia. Preoxygenation prior to intubation provides a “safety cushion” of 6 to 9 minutes before hypoxemia occurs. Presence of an endtidal CO2 is crucial in confirming placement of the ET tube.
Perforation of the esophagus, pharynx, and pyriform sinus are all possible, particularly with difficult intubations. These are serious complications that may progress to neck abscesses, subcutaneous emphysema, pneumothorax, mediastinitis, sepsis, and death. Early recognition and treatment are important because the mortality associated with mediastinitis is at least 50%.
Intracranial intubation is a rare but disastrous complication that usually results from attempted nasotracheal intubation in the presence of skull base fractures or facial trauma.
Pulmonary edema may occur following sudden relief of chronic airway obstruction. It may manifest in the operating room (OR), or later in the recovery room following extubation. Hypoxia, difficulty ventilating the patient, and pink foamy fluid in the ET tube should arouse suspicion as to the cause. The diagnosis is confirmed with a chest radiograph. Treatment usually consists of mechanical ventilation with positive end-expiratory pressure (PEEP) and diuretics.
Barotrauma is usually associated with jet ventilation techniques such as those used in microlaryngeal surgery. High-flow insufflation through catheters distal to the glottis may result in air tracking into peribronchial tissues. Unrecognized, the situation may progress to pneumomediastinum or tension pneumothorax. As discussed previously, use of Hunsaker tubes with automated jet ventilators is helpful in minimizing the risk of these injuries.
Airway obstruction may occur from occlusion of the tube from blood or secretions. Other potential causes include kinking of the tube or, more rarely, cuff herniation over the tip of the tube. Tubes may also become dislodged or disconnected, particularly when they are hidden under surgical drapes. Early recognition is key in rectifying the problem and preventing adverse effects.
Nerve injuries usually result from pressure and may involve the lingual nerve, hypoglossal nerve, recurrent laryngeal nerve, and internal branch of the superior laryngeal nerve. Fortunately, the vast majority are temporary and self-limited. Rare cases of transient hyposmia have been reported following nasotracheal intubation.
Cervical spine injury usually results from excessive neck manipulation and force in attempting to intubate patients with preexisting disease such as ankylosing spondylitis and rheumatoid arthritis. In patients with C-spine fractures, inadequate immobilization prior to intubation may aggravate or worsen the injury. Fiberoptic intubation is often a safer choice in these individuals.
Corneal abrasions are relatively common injuries associated with general anesthesia. They may result from a mask or other object rubbing against the eye or from the eyes being left partially open during anesthesia. Ophthalmology should be consulted for abrasions. Treatment usually consists of antibiotic ointment with an eyepatch. These injuries may be prevented by taping the lids closed and applying eyepads, particularly during head and neck surgery.