Acquired Macular Disease
Introduction
The anatomic macula is defined as the area of the posterior retina containing at least two layers of nuclei within the ganglion cell layer. Clinically, this area extends 6 to 7 mm from the temporal edge of the optic nerve and includes the area within the temporal vascular arcades. Virtually all retinal vascular and retinal inflammatory diseases may involve the macula, as do numerous metabolic, hereditary, degenerative, neoplastic, and traumatic entities. Even vitreous and peripheral retinal and choroidal disorders have potential for macular involvement. A discussion of all potential disorders involving the macula within the scope of a single chapter is thus impossible without some exclusion criteria. Thus, inherited macular dystrophies, inflammatory etiologies, and vascular diseases are not addressed in this chapter.
Acquired macular disorders include diseases that may initially manifest as retinal pigment epithelial derangements with subsequent retinal pathology, or a pathologic condition involving the neurosensory retina may over time effect features of the retina pigment epithelium. Thus, our categorization and organization of macular disorders is arbitrary and is an attempt to simplify the logical progression of this chapter. Topics discussed in this chapter include the following:
Disorders Arising From Retinal Pigment Epithelium and Choroid
Age-Related Macular Degeneration (AMD)
Central Serous Chorioretinopathy (CSC)
Ocular Histoplasmosis Syndrome (OHS)
Angioid Streaks
Disorders Arising From Retinal Pigment Epithelium (RPE), Choroid, and Retina
Pathologic Myopia
Disorders Arising From Retina
Epiretinal Membrane
Macular Hole
Cystoid Macular Edema
Parafoveal Telangiectasis
Age-Related Macular Degeneration
Introduction
First described by Pagenstecher in 1875 and by Haab in 1889, AMD is now the most common cause of blindness in patients older than 60 years of age in the western hemisphere.1,2 The incidence, prevalence, and other epidemiologic associations with AMD are provided in Table 23.1. Calculating the prevalence of macular degeneration has been complicated in the past with different definitions regarding severity of macular degeneration.3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19 Typically, color fundus photography, grading by independent reading centers, and analysis of gender and racial subgroups are performed.8,12,16,17,20,21,22,23,24,25,26,27 Prevalence variations are apparent in various racial subgroups19,28,29,30 (Table 23.1).
Table 23.1 Prevalence of AMD Table | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Growing evidence of an inherited or genetic component influencing the pathophysiologic nature of macular degeneration has accumulated in recent years.10,15,31,32,33 Malattia leventinese and Sorsby’s macula dystrophy are known genetic disorders with phenotypic expression identical or similar to the clinical presentation of AMD.34,35,36,37,38,39 Nevertheless, given the environmental and dietary factors implicated in influencing the expression and severity of disease, the inclusion of AMD in acquired macular diseases is appropriate.40,41,42
Pathogenesis of Age-Related Macular Degeneration
The pathogenesis of AMD involves a complex interaction involving genetic factors combined with senescence of vital structures that normally maintain the health of the photoreceptor-retinal pigment epithelium-Bruch’s membrane complex. The following factors are generally implicated in the development and complications of macular degeneration: genetic influences, extracellular changes, oxidative stresses, hydrodynamic alterations, hemodynamic changes, angiogenic elaboration, inflammatory influences, and apoptotic factors.43,44
Genetic Factors
Although environmental insults that appear to exacerbate or accelerate complications of macular degeneration are undeniable, the influence of genetics is also clear. Twin-concordant studies suggested the initial impact of genetics.10,15,31,32,33,45,46,47 First-degree relatives of patients with AMD are also much more likely to develop exudative complications.48,49 Monozygotic twins exhibit 90% concordance.45,47,50 Mutations in the ATP-binding cassette transporter (ABCA4) gene, which is responsible for forms of Stargardt’s macular dystrophy, cone dystrophy, and retinitis pigmentosa, have been detected in patients with AMD.51 Linkage analysis and genotyping have further correlated genes associated with macular dystrophies similar to phenotypes in AMD. These include Bests disease, Doyne’s honeycomb retinal dystrophy, and Sorsby’s macular dystrophy.36,38,39,52,53,54
With the advent of genetic analysis, three candidate genes have now been identified as strongly linked to the expression of AMD.
Variations in the regulators of complement activation (RCA) gene cluster on chromosome 1q25-q31 are now strongly correlated with macular degeneration. Replacing a tyrosine with histidine at position 402 of this encoding for complement factor H increases the risk of AMD of about fivefold. The risk variation is noted in approximately 40% of Caucasians.55,56,57
Mutations in the LOC387715 gene have been implicated as disease-causing. Specifically, an alanine substitution for serine at position 69 increases the risk of AMD approximated sevenfold. This risk is noted in approximately 30% of Caucasians.58,59,60,61
The factor B (BF)/complement component 2 (C2) locus in the major histocompatibility (MHC) class III region on 6p21.57
Extracellular Factors
Macular degeneration is associated with numerous changes within Bruch’s membrane. Bruch’s membrane separates the RPE from the choriocapillaris and is comprised of five layers: the basement membrane of the RPE, the inner collagenous zone, the elastic fiber layer, the outer collagenous zone, and the basement membrane of the choriocapillaris.62,63,64,65 At birth, Bruch’s membrane averages approximately 2 microns, whereas in adults, Bruch’s membrane thickness varies from 4 to 6 microns.64,65 Changes in membrane thickness are seen secondary to dynamic changes in protein composition, protein cross-linking, increased glycosaminoglycan size, and increased lipid content.66,67,68,69,70,71 These changes correspond to increased dysfunction in RPE cells that produce an excess of cell fragments, collagen, and basement membrane components that are not degraded due to increased impairment in matrix metalloproteinases.72
The maintenance of a healthy Bruch’s membrane is dependent on an intricate balance among collagen, laminin, fibronectin, glycosaminoglycans, and matrix metalloproteinases.62,72,73,74,75,76,77,78,79,80,81,82,83 The aging Bruch’s membrane contains an ever-increasing amount of type I collagen, debris, and filamentous material.66,84 An age-related decrease in laminin, fibronectin, and type IV collagen is also seen within the RPE basement membrane.68,69,80,85,86,87 Glycosaminoglycans, specifically heparin sulfate, increase in size and content.66,69,85,88 The end products of glycosaminoglycan accumulation result in macromolecules, which alter the normal physiologic negative electrical potential of the Bruch’s membrane–RPE complex.77,78
Hydrodynamic Factors
Bruch’s membrane serves a vital function in the permeability of water.82,83,89 Hydraulic conductivity decreases with age, with the inner collagenous layer of Bruch’s proposed as the primary site of hydraulic conductivity.79,82,83,90,91 An increase in this layer is noted as lipid and debris accumulate with age.67,68,69 Lipids, the end product of long-chain polyunsaturated fatty acids found in photoreceptor outer segments may alter the negative electrostatic charge of Bruch’s membrane resulting in a change in hydraulic conductivity of special importance due its intimate relationship with the choriocapillaris.82,83,89,91
Age-related deterioration in hydraulic conductivity with Bruch’s membrane produces an increase impedance of diffusion of vital metabolic exchange between the choroid and the retina and may disrupt photoreceptor function.90,91 The net result may be the accumulation of large confluent hydrophobic drusen that predispose to RPE detachments and hydrophilic drusen that predispose to the formation of choroidal neovascularization.74,92,93,94
Hemodynamic Factors
The choriocapillaris is not immune to age-related change.85,95,96 The density of the choriocapillaris and lumen diameter decrease with age.95,97 Subfoveal choroidal flow and perfusion based on indocyanine green angiography (ICG) are all noted to decrease with age.95,97 Guymer et al. have proposed that choriocapillaris has a vital role in the clearance of metabolic end products from Bruch’s membrane.76,98,99 The loss of normal vasculature within the choriocapillaris with advanced age may be a causal factor in the thickening of Bruch’s membrane.76
Oxidative Factors
Oxidative stress results in the generation of factors implicated in macular degeneration.100,101 The interaction between the retina and the RPE is a prime candidate for potential oxidative stress.100,102,103,104,105 Reactive oxygen species may be stimulated by a spectrum of factors including genetic proclivity, phototoxic injury, inflammation, hemodynamic abnormalities, and reperfusion injury.104 This results in the generation of free radicals. Within the eye, the photoreceptor and RPE receive high oxygen saturation due to their immense metabolic demands.106 Any increase in toxic end products of metabolic activity may precipitate the acceleration of photoreceptor death.100,107 Photoreceptor phagocytosis and vitamin A metabolism, the primary functions of the RPE, also result in oxidative stress.106,108,109 Finally, the retina itself is exposed over a lifetime to cumulative levels of irradiation.110,111 Photosensitizers within the retina and RPE include rhodopsin, lipofuscin, and cytochrome c oxidase, all of which may generate free oxygen radicals.101,112,113
Angiogenic Factors
Choriocapillaris ingrowth into Bruch’s membrane is inhibited by a complex interaction of angiostatic factors. Several factors have been implicated in influencing choroidal neovascularization.
Vascular endothelial growth factor is expressed in embryonic vascular tissues. As an extremely powerful regulator of vascular endothelial cell division, VEGF is induced by hypoxia.115,132,133 In addition to its mitogenic role on vascular tissue, degradation of extracellular matrix, endothelial cell migration, and vascular permeability are also potent effects.114,126,132 Within ocular tissues, VEGF has been experimentally shown to induce iris and retinal neovascularization in animal models.134,135,136,137,138 Elevated levels have been implicated in disease states including diabetic retinopathy, vascular occlusion, retinopathy of prematurity, and neovascular glaucoma.139,140,141,142,143,144,145,146 Within the healthy eye, retinal pigment epithelium produces VEGF as a trophic factor to maintain a normal relationship between RPE and choriocapillaris.147 Hypoxic-ischemic injury may alter the normal VEGF levels inducing aberrant endothelial cell growth, disruption of the normal extracellular matrix, and initiation of leakage from previously competent vessels.115,132
Other angiogenic factors include basic fibroblast growth factor, angiopoietins, PEDF, and nitric oxide. Basic fibroblast growth factor has also been detected in choroidal neovascular membranes.119,120 In porcine and rabbit models, fibroblast growth factor induces choroidal neovascularization.148,149 Low-intensity photocoagulation stimulates the overexpression of BFGF in mice.150 The angiopoietins are a family of molecules found in normal endothelial cells, but when exposed to elevated levels of VEGF lead to the development of enlarged caliber vessels.151,152
PEDF is a neurotrophic growth factor produced by RPE cells with inhibitory effects on angiogenesis.116,117,128,129,131,153,154 PEDF also acts as a potential counterbalance to the effects of VEGF, typically expressed in avascular tissues such as cornea and vitreous.128,129,154,155 In the aging vitreous and senescent RPE cells, PEDF is found to be in declining concentrations.153,154 Nitric oxide, a component known for its systemic effects on pulmonary and systemic blood pressure, may also induce angiogenesis by promoting endothelial cell migration and differentiation through effects on surface molecules such as integrins, which promote neovascularization.156,157
Inflammation
Inflammation is an important stimulus of exudative AMD.96,158,163 Components of drusen include immunoglobulin molecules and complement activators.66,158,164,165,166,167,168 Hageman et al. suggested that choroidal dendritic cells recruited by senescent or damaged RPE cells mediate immune responses in a fashion similar to the development of atherosclerotic plaques.169,170 Further evidence of inflammatory components includes the presence of immune cells such as macrophages, leukocytes, within degenerative RPE, as well as choroidal neovascular membranes.162,166,171,172,173 RPE debris and end products of Bruch’s membrane may provide the nidus for inflammation in eyes with macular degeneration.67,159,162,169,174
Apoptosis
RPE senescence and eventual apoptosis may be a reflection of a combination genetic factors and inflammatory etiologies.132,164,175,176 Senescence may be accelerated with the expression of genes that result from the exposure of RPE cells to oxidative stress and age.175 Foveal RPE cells lose their shape and density throughout life.177,178 Lysosomal activity in RPE cells decrease with age, and the resultant increase in end products may lead to reactive injurious compounds within Bruch’s membrane.177,178,179 These changes appear accelerated in RPE cells exposed to ultraviolet radiation and anaerobic conditions.105,110,111
Drusen
Introduction
Donders first described the characteristics of drusen in 1854.85,180 Drusen, he proposed, are the products of RPE conversion.85,180 Muller suggested drusen arise via deposition from intact RPE.181 Friedman described blood end products as the source of drusen accumulation.182 Histopathologic studies by several authors including Sarks and later by Green et al. subsequently elucidated the currently accepted pathogenesis of drusen.81,183,184
Clinical Findings
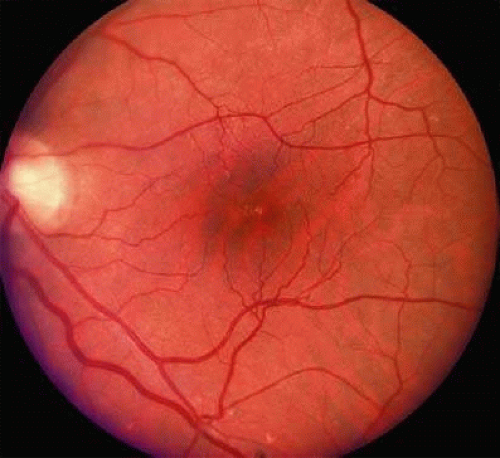
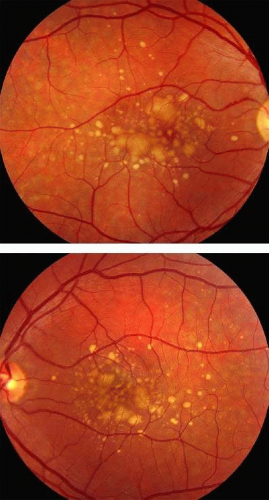
Drusen may be broadly described as hard drusen, less than 63 microns with well-defined borders, and soft drusen, greater than 64 microns with ill-defined borders. Several more specific classifications based on histopathology have also been proposed. Sarks et al. described five general categories based on morphology: hard drusen, hard drusen clusters, soft cluster-derived drusen, soft membranous drusen, and basal laminar or cuticular drusen81,183,185 (Fig. 23.1). Hard drusen clusters are more confluent accumulations of drusen that may occur in excess of 63 microns. Soft cluster-derived drusen are also yellow in color but have indistinct margins. Typically, soft clusters are found in patients greater than 55 years. Soft membranous drusen are yellow, indistinct lesions smaller in diameter than soft cluster-derived drusen but are confined to the macula and are thought to predispose to choroidal neovascularization Fig. 23.2) Basal laminar drusen are small, well-demarcated drusen with an often radial distribution throughout the macula 85,184,186 (Fig. 23.3)
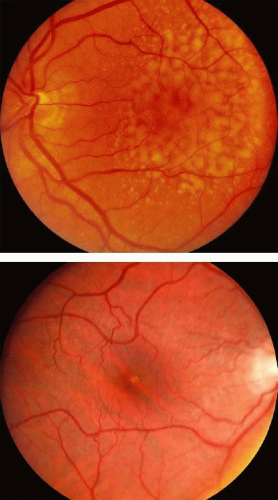 FIGURE 23.2 Soft drusen are larger than hard drusen with indistinct borders and tend to be confluent. |
 FIGURE 23.3 Basal Laminar Drusen is smaller, well demarcated formations that occasionally radiate from the macula. |
Hard drusen are accumulations of hyaline over thinned RPE.85,187,188,189 They may be noted at younger ages, though drusen less than 25 microns are difficult to detect clinically. Focal areas of increased density of Bruch’s membrane, termed microdrusen, precede the formation of hard drusen.183 Although the presence of small hard drusen is not prognostic for the development of macular degeneration in young patients, a large abundance have been described in patients with RPE atrophy.190,191,192 Hard drusen clusters occur later in life and are thought to regress over time evolving into a corresponding locus of atrophic RPE.191,192
Soft drusen are typically larger than 63 microns and have amorphous or poorly defined borders in contrast to hard drusen. Histologic studies suggest soft drusen are basal linear deposits external to the RPE membrane.183,184,193 Soft cluster-derived drusen and soft membranous drusen are thought to be difficult to distinguish on biomicroscopy, and differences are present on a histologic basis. Large soft drusen accumulations may coalesce into pigment epithelial detachments in the absence of choroidal neovascularization (drusenoid pigment epithelial detachment)92,193,194 (Fig. 23.4).
Ancillary Tests
Angiographic characteristics of drusen vary. Hyperfluorescence generally occurs from a combination of RPE loss of pigment over drusen and dye leakage into sub-RPE deposits.195 The timing of hyperfluorescence within angiographic studies is dependent on the constituents of the drusen and on the rate of staining of Bruch’s membrane.195 Drusen may also demonstrate direct staining. If RPE hyperpigmentation is present, many drusen may be obscured by relative hypofluorescence due to blocked fluorescein transmission. Delays in normal choroidal fluorescence have been attributed in some to delays in staining of Bruch’s and sub-RPE contents rather to the true lack of perfusion of choroidal vessels.97,196
Hard drusen and hard cluster-derived drusen typically appear as transmission defects due to overlying retinal pigment epithelial thinning or depigmentation.184,195,197 Hard drusen are thought to obtain greatest fluorescence minutes after injection with corresponding decrease in fluorescence paralleling background choroidal fluorescence.184,195,197 Angiography may reveal a greater number of hard drusen than are appreciated on biomicroscopy.184,195,197 Hard drusen are noted to fluoresce during angiography with indocyanine green dye (ICG).198,199,200,201,202,203
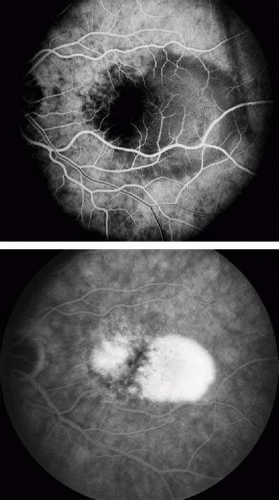
Soft drusen demonstrate progressive hyperfluorescence and dye pooling without leakage beyond their margins.184,195,197 Drusen that hyperfluoresce are thought to be hydrophilic secondary to the diffusion of water-soluble fluorescein.184,195,197 Alternatively, hypofluorescent drusen are possible hydrophobic due to the presence of neutral lipids. The hyperfluorescence is typically less intense and occurs later than the fluorescence exhibited by hard drusen.184,195,197 On ICG angiography, soft drusen are typically hypofluorescent.198,199,200,201,202,203 Studies have also identified vascularization of soft drusen, which may account for a component of the hyperfluorescence. Membranous drusen characteristics include very faint delayed hyperfluorescence on fluorescein angiography and are not detected on ICG angiography.198,199,200,201,202,203 Angiography of basal laminar drusen reveal early, discrete hyperfluorescence and late fading that has been described as “stars-in-the-sky.”204 (Fig. 23.5)
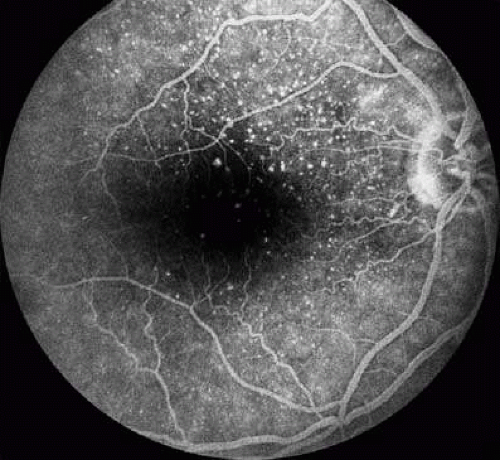 FIGURE 23.5 Fluorescein angiography of basal laminar drusen demonstrating the radial hyperfluorescence and small transmission defects in the classic “star-in-the-sky.” |
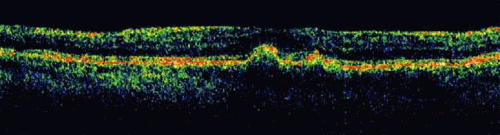
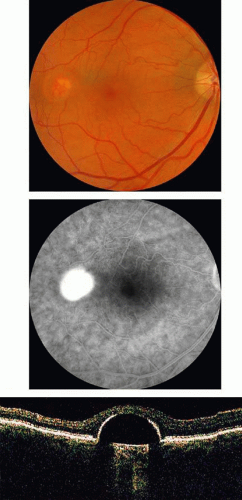
Optical coherence tomography (OCT) is a computer analysis tool that generates a cross-sectional view of the vitreomacular junction, neurosensory retina, retinal pigment epithelium, and Bruch’s membrane in a manner reminiscent of gross histological sections.205,206,207,208 Due to the reflective qualities of these interfaces, OCT imaging is able to detect the density differences in anatomic structures. As the vitreous fluid is relatively homogenous, OCT images depict the vitreous as black when compared to more reflective interfaces such as the posterior hyaloid, internal limiting membrane, neurosensory retina, and retinal pigment epithelium. Each layer is assigned a schematic color representation for ease in clinical analysis. Software computations allow an estimate of retinal thickness to within 3 μm.209,210,211 Drusen, which typically arise within the highly reflective retinal pigment epithelium layer, lead to local elevations, excrescences, and distort of the overall contour of the OCT-generated image210,212 (Fig. 23.6).
Pigment Epithelial Detachment
Synonyms: Drusenoid pigment epithelial detachment, serous pigment epithelial detachment
Introduction
Soft drusen often accumulate and coalesce forming overlying detachment of the retinal pigment epithelium. Decreased hydraulic conductivity across Bruch’s membrane and a thickened, hydrophobic barrier mark some of the critical changes in Bruch’s membrane in eyes with macular degeneration.82,91 A thickened, less soluble, lipophilic Bruch’s results in a hydrophobic state, suggested as a primary factor in the formation of RPE detachments.91,92,213 Bird et al. have suggested that serous RPE detachments occur due to a combination of the aforementioned hydrophobicity of Bruch’s, the potential cleavage plane that may exist between the basement membrane of the RPE and the inner collagenous layer and the water accumulation secondary to ion transport dynamics at the level of the retinal pigment epithelium.74,92
Clinical Features
The delineation between elevation of the retinal pigment epithelium due to drusen and leakage from an occult choroidal neovascular membrane can be quite difficult. Both are detected on biomicroscopy via elevation of the neurosensory retinal and retinal pigment epithelium in a blister like appearance. Drusenoid detachments because of their origination from drusen are themselves yellow, amorphous, and in many patients, asymptomatic (Fig. 23.7). Serous elevation in patients may be symptomatic and may not appear with drusen if related solely to serous fluid within the potential space of the sub-RPE. Detachments of the RPE may occur in isolation or may be seen with accompanying serous detachment of the neurosensory retina.
Roquet et al. followed 61 eyes of 32 patients and reported the clinical features of drusenoid pigment epithelial detachment.214 Three different natural outcomes were noted: persistence, atrophy, and choroidal neovascularization. Drusenoid pigment epithelial detachment was associated with a 50% risk of progressing to atrophic lesions after 7 years. Drusenoid pigment epithelial detachments larger than two disc areas (DD) and those associated with metamorphopsia were associated with higher risk of progression to atrophy or choroidal neovascularization after 2 years.
Ancillary Tests
On angiography, serous RPE detachments are characterized by a uniform, well-demarcated leakage into a potential space resulting in pooling of fluorescence, which is correlated with a blister-like elevation of the RPE and neurosensory retina195 (Fig. 23.8) Unlike a serous RPE detachment where angiographic pooling uniformly increases remains bright in the late phase, drusenoid RPE detachments are less fluorescent and either stain faintly or fade in the late phases of the study.195 Optical coherence tomography is effective in detecting pigment epithelial detachment, revealing the irregular elevation of the RPE. Drusenoid detachments demonstrate a hyperreflectivity of the drusenoid material.206
Atrophic Age-Related Macular Degeneration
Synonyms: Dry macular degeneration, geographic atrophy
Introduction
Geographic atrophy is defined as confluent areas of RPE death which progress to overlying photoreceptor atrophy or death.96,192 Twenty percent of legal blindness is attributed to visual loss secondary to atrophic macular degeneration.215 The estimated prevalence of geographic atrophy ranges from approximately 0.4% to 1.6% and increases with patient age.8,23,216 In the Beaver Dam study within the United States, in patients older than 75 years, the prevalence ranged from 3.5% to 7.1%.216 The overall 5-year incidence of pure geographic atrophy development was 0.3%.42,216 The presence of geographic atrophy does not exclude the possibility of later development of exudative forms of AMD.184 In the eyes with choroidal neovascularization and a fellow eye with geographic atrophy, the incidence of future choroidal neovascularization in the fellow eye ranged from 30% to 50%.217 Green et al. demonstrated a 34% incidence of geographic atrophy in histopathologic studies of patients with choroidal neovascularization.184 Therefore, it is unlikely atrophic and exudative AMD represent two entirely different diseases.
Pathogenesis
Because of the dependence of the photoreceptors on the RPE, apoptosis of both the outer nuclear layer and the inner nuclear layer of the retina have been found associated with areas of RPE atrophy.164,178,218 Sunness et al. have described the biologic etiologies of geographic atrophy.217,219,220,221,222,223,224,225,226,227,228,229,230 Large drusen and pigmentary abnormalities are associated risk factors for the eventual development of atrophic areas.12,16,23,43,225,231,232 Perfusion abnormalities and decreased vascular density are also implicated in the development of RPE loss.97,196,233,234 Vascular defects may result in a lack of trophic factors including VEGF that lead to subsequent RPE death and secondary photoreceptor depletion.155
Lipofuscin is implicated as both a possible indicator of devitalized retinal pigment epithelium and as a generator of free radicals.101,110,112,235 Lipofuscin can now be visualized with retinal pigment epithelial autofluorescence imaging and is often predictive of future sites of atrophic RPE.236,237,238,239,240 Lipofuscin may lead direct or indirectly to RPE cell death.70,108,241,242,243,244 Cells becoming engorged or laden with lipofuscin containing residual bodies may be unable to maintain normal cell metabolism. Lipofuscin is a known free radical generator but may also have direct toxic effects on cells by causing premature enzymatic lysosome release.101,112,245,246 The highest turnover of outer segments involves rods just outside the fovea, which parallels the distribution of lipofuscin in the RPE.101,112 Subfoveal RPE contains a relative increased amount of macular pigments, the highest cone density, and a reduced rod density.175,177,184,247,248 Thus, geographic atrophy often spares the fovea until advanced stages of macular degeneration.
Clinical Features
Atrophy may arise from areas of previous drusen, retinal pigment epithelial detachment, or choroidal neovascularization.43,85,190,192,249 Neovascularization tends to arise in close proximity to adjacent atrophied areas.190,192,217,219 Geographic atrophy is bilateral in many patients and is typically associated with an atrophic choriocapillaris in which the larger caliber vessels of the choriocapillaris are evident on biomicroscopy. Large drusen and pigment derangements involving the retinal pigment epithelium evolve into atrophic loci in many patients (Fig. 23.9)
Geographic atrophy leads to gradual and occasionally unpredictable visual loss.192,250 Visual acuity may not measure the degree of functional impairment in patients with scotoma near fixation.192,223,225,227,251 Visual acuity in dim illumination is preferentially affected secondary to a profound loss in retinal sensitivity.227,251 In patients with visual acuity of 20/50 or better, approximately 50% experience a loss of three or more lines over 2 years.192,221,228 Twenty-five percent of patients with geographic atrophy lose six or more lines over 2 years.228
Exudative Age-Related Macular Degeneration
Synonyms: Wet AMD, disciform macular degeneration
Introduction
Exudative AMD occurs when choroidal neovascularization occurs. Choroidal neovascularization is defined as the growth of blood vessels from choroidal vasculature. Exudative AMD accounts for 75% of severe visual loss in patients and if untreated is associated with an extremely poor visual prognosis.216 The Macular Photocoagulation Study (MPS) demonstrated 62% to 65% of patients with extrafoveal and juxtafoveal lesions were associated with severe visual loss defined as the loss of six or more lines of Snellen visual acuity.252,253,254,255,256,257,258 Severe visual acuity loss due to subfoveal lesions in the MPS ranged from 55% to 65%.255,256,259
Histopathologic characteristics of CNV in eyes with macular degeneration include early capillary ingrowth in larger soft drusen.96,184,185,260,261,262,263 The vessels enlarge in caliber over time and acquire both arterial and venular characteristics.184 Separation of tissue planes within Bruch’s membrane allows for further choroidal vascular ingrowth.184 Eventually, subretinal blood and exudates may lead to marked serous or hemorrhage detachment or the retina as well as retinal pigment epithelium.184 The hemorrhage may resolve and often results in further proliferation of pigment epithelium and fibrous components within the subretinal space.184 The final outcome in many cases is the development of disciform scar, composed of fibrous tissue proliferation secondary to the presence of hemorrhage and hyperplasia of the RPE itself.184 Disciform lesions may lead to further complications including persistent exudation and even pressure necrosis of arteries communicated between the choroid and the fibrous scar resulting in massive hemorrhage within the sub-RPE or subretinal space.262,264
Clinical Features
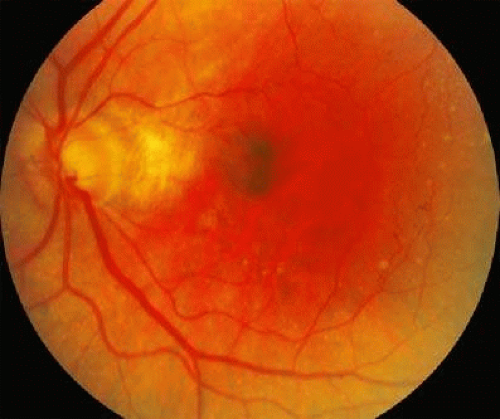
The presence of choroidal neovascular membranes may not result in symptomatic changes in the patient. Even on careful clinical examination, the presence of a small lesion is often difficult to detect. The presence of hemorrhage or subretinal exudation leads to elevation of the neurosensory retina or retinal pigment epithelium and resulting loss of visual acuity or metamorphopsia. On biomicroscopy, neovascular membranes are often described as gray or green subretinal tissue (Fig. 23.10)
Ancillary Tests
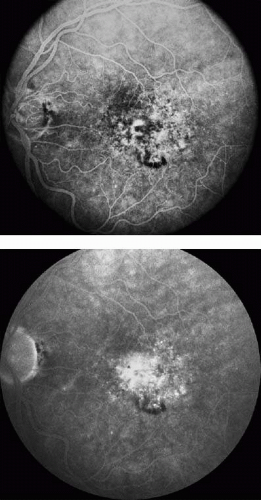
The conversion to choroidal neovascular membranes in patients with macular degeneration is heralded by a variety of fluorescein angiographic changes. These changes may be limited to hyperfluorescence in a nonspecific pattern in the latter phases of the angiograms or may be easily apparent within the arteriovenous phases with prominent leakage or have a typical pattern of well-demarcated, “lacy” hyperfluorescence within the earliest fluorescein dye (Fig. 23.11) The myriad interpretive skills required to correctly diagnose and evaluate various choroidal neovascular membranes are beyond the scope of this chapter. Patients with “classic” choroidal neovascular membranes seen in the arteriovenous frames of the angiogram often are followed by profound leakage in the later phases.255,256,258,265 (Fig. 23.12). Occult lesions may be characterized as any fluorescence not due to drusen that deviate from this “classic” pattern. Specifically, occult lesions may not demonstrate significant early-phase angiographic lesion but may demonstrate a “stippled” amorphous hyperfluorescence notable only in the late phases of the angiogram253,254,255,266 (Fig. 23.13).
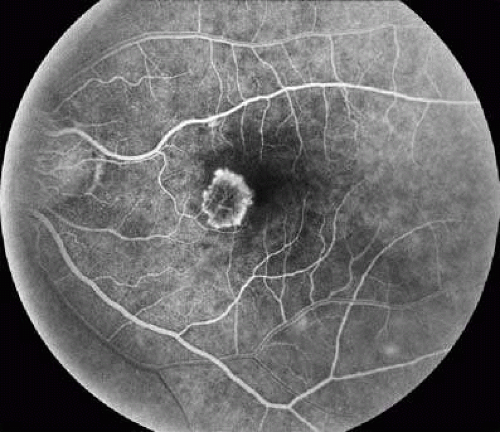 FIGURE 23.11 Fluorescein angiography of classic choroidal neovascular membranes is characterized by early lacy hyperfluorescence in the arteriovenous filling phase of the angiogram. |
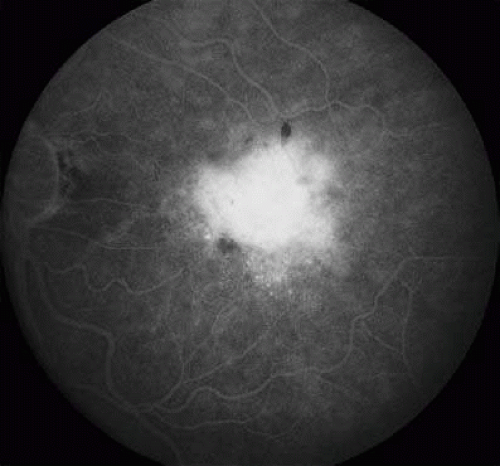 FIGURE 23.12 Fluorescein angiography of late leakage in classic choroidal neovascular membranes reveals profound hyperfluorescence that obscures the view of the borders of classic membrane. |
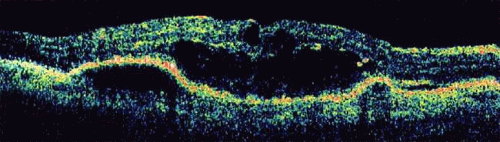
Optical coherence tomography is a useful ancillary and diagnostic tool used solely or in concert with angiograms and always coupled with clinical examination to stage, detect, and evaluate choroidal neovascular membranes.206,210,267,268 As choroidal neovascular membranes invade the subretinal space, they are characterized by disruption of the RPE. A physician interpreting an OCT scan may confuse the neovascular lesion with the RPE or choriocapillaris, as both have similar reflectivities. Neovascular membranes are associated with elevations caused by fluid leakage that accumulates in intraretinal or subretinal potential spaces206,210,268,269 (Fig. 23.14). The lesion itself may appear on OCT as a high backscattering lesion of well-defined thickening within the retinal pigment epithelial and choriocapillaris junction. OCT allows a measurement of retinal thickness and detection of the absence of RPE, detection of fibrotic scars, PED, and RPE tears. Distinguishing diffuse from cystoid macular edema, central serous chorioretinopathy from PED, and neurosensory retinal detachment from PED are all aided by the use of OCT.
Treatment
The treatments used to limit the progressive and occasionally catastrophic visual loss associated with the natural history of untreated choroidal neovascular membranes have undergone various stages of evolution and revolution. The benefit of placebo controlled, randomized, multicentered trials have aided in distinguishing effective treatments. Herein are significant treatment algorithms that have been applied treatment paradigms for exudative macular degeneration.
Multivitamin supplementation for prevention of severe loss for macular degeneration
The Age-Related Eye Disease Study (AREDS), an 11-center double-masked clinical trial, enrolled participants with extensive small drusen, intermediate drusen, large drusen, noncentral geographic atrophy, or pigment abnormalities in one or both eyes, or advanced AMD or vision loss due to AMD in 1 eye.40,270,271 Participants were randomly assigned to receive daily oral tablets containing:
Antioxidants (vitamin C [500 mg], vitamin E [400 IU], beta carotene [15 mg]
Zinc, 80 mg, as zinc oxide and copper, 2 mg, as cupric oxide
Antioxidants plus zinc
Placebo
Photographic assessment of progression to or treatment for advanced AMD and at least moderate visual acuity loss from baseline were used as primary outcomes. Serum-level measurements, medical histories, and mortality rates were used for safety monitoring.40,270,272
Average follow-up of the 3,640 enrolled study participants, ages 55 to 80 years, was 6.3 years, with 2.4% lost to follow-up. Comparison between placebo and the patients receiving antioxidants plus zinc demonstrated a statistically significant odds reduction for the development of advanced AMD with odds ratio (OR), 0.72; 99% confidence interval (CI), 0.52–0.98. The ORs for zinc alone and antioxidants alone were 0.75 (99% CI, 0.55–1.03) and 0.80 (99% CI, 0.59–1.09), respectively.40,270
In addition to these findings the natural history of patients enrolled with extensive small drusen, nonextensive intermediate size drusen, or pigment abnormalities had only a 1.3% 5-year probability of progression to advanced AMD. Both zinc and antioxidants plus zinc significantly reduced the odds of developing advanced AMD in the higher-risk groups. Statistically significant reduction in rates of moderate visual acuity loss occurred in persons assigned to receive antioxidants plus zinc (OR, 0.73; 99% CI, 0.54–0.99).40,270
Based on these findings, clinicians began recommending individuals older than 55 years with extensive intermediate-size drusen, at least one large druse, noncentral geographic atrophy in one or both eyes, or advanced AMD or vision loss due to AMD in one eye, and without contraindications such as smoking, should consider taking a supplement of antioxidants plus zinc such as that formulated in the AREDS study.40,270,273,274,275
Thermal laser photocoagulation treatment
The Macular Photocoagulation Study was a series of multicentered randomized controlled clinical trials designed to determine whether argon laser photocoagulation was effective for preventing or delaying severe visual loss in eyes with an extrafoveal and juxtafoveal choroidal neovascular membranes secondary to the following: age-related macular degeneration (Senile Macular Degeneration Study, SMDS), ocular histoplasmosis (Ocular Histoplasmosis Study, OHS), and idiopathic neovascularization (Idiopathic Neovascularization Study, INVS).252,253,254,255,256,257,258,259,265,276 Later, a cohort of patients with subfoveal choroidal neovascularization were also treated with laser photocoagulation and followed for treatment benefit in regards to visual loss prevention and recurrence rates.255,256,265
In the initial extrafoveal treatment algorithm, patients were randomized to treatment or to no treatment group until recruitment was terminated in 1982 (SMDS) and 1983 (OHS and INVS) due to significance of treatment benefit.252,257 The relative risk of experiencing severe loss of vision after three years in eyes initially assigned to the no-treatment group in comparison with eyes assigned to the argon laser photocoagulation group was 1.4 in the SMDS (95% confidence interval [CI] 1.1 to 1.9), 5.5 in the OHS (95% CI: 3.9 to 10.8), and 2.3 in the INVS (95% CI: 0.8 to 6.5).252,254,257
Outcome measures for patients with juxtafoveal lesions included changes in visual acuity at 5 years of follow-up and rates of persistent and recurrent choroidal neovascularization.254 Data were accumulated for 276 (92%) of 300 patients with AMD, 236 (92%) of 256 patients with ocular histoplasmosis, and 38 (97%) of 39 patients with idiopathic choroidal neovascularization. In eyes with AMD, the estimated relative risk (RR) of a loss of six or more lines of visual acuity from baseline to any examination from 6 months through 5 years after enrollment for untreated eyes in comparison with treated eyes was 1.20 (p = .04).252,254,255,256,257,265 Normotensive patients were noted to have benefit from laser treatment (RR,1.82) but little or no benefit (RR, 0.93) was noted in hypertensive patients. Untreated eyes with ocular histoplasmosis were at much greater risk of a six-line decrease in visual acuity from the 1-year through the 5-year examination than were treated eyes (unadjusted RR, 2.60; RR, 4.26 after adjustment for visual acuity and hypertension at baseline; (p < .001 for both).252 In idiopathic choroidal neovascularization, effects of treatment appeared to fall in between AMD and ocular histoplasmosis-related choroidal neovascularization.252,256,257,265 On this basis the retina community recommended laser treatment of choroidal neovascularization in juxtafoveal locations with the caveat that hypertensive patients with AMD carried a much more guarded prognosis.252,253,254,255,256,257,258,259,265,276
Finally, the Macular Photocoagulation Study Group also reported the treatment outcomes and benefits of subfoveal lesions.255,256,265 Eyes of consenting patients were once again assigned randomly to laser treatment or no treatment. Visual acuity, reading speed, and contrast threshold were measured before random assignment 3 and 6 months later and at 6-month intervals thereafter.256 Four years after enrollment 39 (47%) of 83 untreated eyes and 17 (22%) of 77 laser-treated eyes had lost six or more lines of visual acuity from baseline levels (p = .002).256 At the 3-year examination of patients re-treated for recurrent choroidal neovascularization, 21 (36%) of 58 untreated eyes and 6 (12%) of 49 treated eyes had lost six or more lines of visual acuity from baseline levels (p = .009).256 However, treatment was associated with almost immediate three-line average loss of vision. This decrease in vision persisted as compared to untreated eyes at 3-month and 6-month follow up examinations.256 This profound, treatment-associated decrease in vision spurred clinicians to continue the search for improved treatment modalities.
Photodynamic treatment
Photodynamic therapy (PDT) involves a photosensitizer, a chemical activated in response to light. Prior the Federal Drug Agency (FDA) approval of PDT, the primary treatment for choroidal neovascularization secondary was thermal laser photocoagulation.277,278,279,280,281,282,283,284 Especially for subfoveal lesions, photocoagulation was often excessively destructive resulting in post-treatment-related acute declines in vision.259 Verteporfin is a specific photosensitizer infused intravenously, which is derived from porphyrin.277 The lipophilic drug is complexed with circulating low-density lipoproteins (LDL), which complexes with more rapidly dividing endothelial cells of growing blood vessels, but not by normally resting endothelial cells.277 Activation thus leads to direct oxidative damage to the neovascular endothelial tissue with progressive thrombosis. In the FDA approval process for Verteporfin, several variables were studied: dose of the drug given, amount of energy applied, and the interval between the infusion and application of laser. Verteporfin doses of 6 mg/mm2 body surface area, infused 15 minutes before an application of 689 nm wavelength light at 600 mW/cm2 was approved.277 An application of 83 seconds producing a total 50 J/cm2 was delivered to the ocular tissues.
Several randomized trials produced data resulting in the widespread adoption of verteporfin for subfoveal choroidal neovascular membranes. The Treatment of Age-Related Macular Degeneration with Photodynamic Therapy Group (TAP) Trial included patients receiving PDT versus placebo for patients with AMD and subfoveal lesions with some degree of classic presentation.279,282,283 Specific inclusion criteria included lesions less than 5,400 μm in greatest linear dimension and visual acuity between 20/40 and 20/200. Primary outcome was loss of vision of less than 15 letters, or three lines, with examinations at 3-month intervals.279,282,283 Treatment was repeated in persistently leaking lesion, based on fluorescein angiography.
A benefit of PDT over placebo sustained over a 2-year study period was demonstrated, with 53% of the Verteporfin- and photodynamic-treated eyes losing three lines or less, compared to 38% of controls.282 The secondary end point of prevention of severe visual loss (loss of 30 letters or six lines Snellen acuity) was also statistically significant with 82% treated eyes versus 70% control eyes maintaining vision. Additional analysis yielded observations regarding lesion size, which demonstrated a trend toward better maintenance with the Verteporfin group.282 At 24 months of treatment, 23.1% of PDT eyes compared to 53.6% of control eyes had an increase in the lesion size. Fifty-one percent of Verteporfin-treated eyes versus 28.5% of placebo eyes had no classic features identified on angiogram.282 In the first year, an average of 3.4 treatments was required, whereas in the second year 2.2 treatments were performed.279,282
The Verteporfin in Photodynamic Therapy Study Group (VIP) examined the effects of PDT on lesions due to subfoveal choroidal neovascularization in which the lesions had no classic angiographic features and evidence of recent progression of disease and vision of at least 20/100.277,281,285 Also, the benefit of treatment for classic CNV with vision better than 20/40 was also studied. The primary outcome was loss of at least 15 letters, a difference from the TAP study, being a measure of loss of vision rather than preservation of vision.285
The VIP study showed no treatment benefit at 12 months.277 At 24 months, however, statistical significance was achieved, with treatment significance for the secondary outcome of severe visual loss (loss of 30 or more letters).285 Further subgroup analysis demonstrated lesions benefiting were those composed of occult with no classic characteristics and small lesion size (less than four disc areas), or worse vision at baseline (20/50).277,285,286 On this basis, predominantly classic lesions and occult lesions less than four MPS disc areas with recent disease progression and vision worse than 20/50 were recommended for treatment.278 Additional studies including earlier treatment prior to 3 months and changes in light application settings (fluence) did not demonstrate statistically significant results.287
Clinicians described the use of combination therapy with PDT and triamcinolone injected within the vitreous cavity.288,289,290,291,292,293,294,295,296,297 Various dosages have been described with this combination treatment, but this treatment lacked the proof of randomized controlled trials to test its efficacy.163
Anti-VEGF treatments
Antivascular endothelial-derived growth factor medications have heralded a new era in the treatment of exudative macular degeneration.114,126,298,299,300,301,302 Beginning with the initial results of the use of pegaptanib, the concept of intravitreous delivery of medications via periodic injections have revolutionized the treatment of choroidal neovascular membranes.303 The most significant of these thus far has been the ranibizumab, an anti-VEGF aptamer. Ranibizumab was studied initially with combined use of verteporfin and PDT in a randomized single masked phase I/II trial. The safety and efficacy of ranibizumab in combination with verteporfin PDT versus verteporfin and PDT alone in patients with subfoveal predominantly classic CNV due to AMD demonstrated the significant benefits of ranibizumab.304 One week before the first administration of either intravitreal ranibizumab or sham injection to the study eye, patients were treated with verteporfin PDT and with as many as 23 additional monthly injections with ranibizumab or sham injection.304 Patients continued to receive verteporfin PDT at the discretion of the investigator, in accordance with product labeling. The primary efficacy endpoint was the proportion of patients losing fewer than 15 letters at 1 year. The study enrolled 162 patients.304
The results were significant, both statistically and clinically. Approximately 90% of patients treated with the combination therapy had stable or improved visual acuity, compared with approximately 68% of patients in the control arm of PDT alone. Patients treated with combination therapy had significantly improved vision compared to baseline acuity; mean vision in the PDT alone control group decreased from baseline.304
A phase III, multicenter, randomized, double-masked, sham-injection-controlled trial included 716 patients with minimally classic/occult CNV secondary to AMD.305,306 Eligible patients had not previously received subfoveal laser treatment, verteporfin photodynamic therapy, or experimental treatments for their AMD in the study eye.305,306 Patients were randomized 1:1:1 to sham injection or to ranibizumab (0.3 mg) or 0.5 mg injected intravitreally monthly for 24 months.305,306 The primary efficacy end point was the proportion of subjects losing less than 15 ETDRS letters at 1 year. Approximately one-third of the patients had minimally classic CNV, and two-thirds had occult CNV.305,306
At 1 year, approximately 95% of patients treated with ranibizumab lost fewer than 15 letters at 1 year versus 62% in the control group.305,306 On average the patients treated with ranibizumab had a significant visual acuity improvement compared to baseline, whereas the control group experienced a substantial decrease from baseline in mean VA. Ocular adverse events included incidences of uveitis and endophthalmitis, each less than 1%.
Central Serous Chorioretinopathy
Synonyms: Central serous retinopathy, idiopathic central serous choroidopathy
Introduction
Von Graefe described an entity termed “recurrent central retinitis” in 1866, composed of serous detachment involving the macula.308,309 Bennett subsequently referred to this entity as central serous retinopathy, with Gass providing the term idiopathic central serous choroidopathy.310 Central serous retinopathy is best characterized as a decompensation of the choroid and retinal pigment epithelium, resulting in a tell-tale detachment of the neurosensory retina or retinal pigment epithelium.310,311,312,313,314,315,316,317,318,319,320,321,322,323,324,325 Since von Graefe’s original description, central serous retinopathy has remained a unique affliction, associated with Type A personality, emotional stress, and corticosteroid medication use.326,327,328,329,330,331,332,333,334
Epidemiology
Central serous retinopathy has been characterized as affecting young and middle-age adults between the ages of 20 and 50 years of age, although multiple reports of CSR affecting individuals older than 60 years have been presented.335,336,337,338,339,340,341 Men are more likely to be affected than women by a 9:1 ratio.310,342 Spaide reported his experience with patients above 50 years of age.341 In this retrospective cohort, the ratio of female to males was almost 1:1.341 Central serous retinopathy in women should perhaps be considered a distinct clinical entity as opposed to the condition that afflicts younger males. Female cohorts are likely to be older on average and may be more likely to have fibrinous subretinal deposits.339,340,343
Pathogenesis
The exact mechanism of central serous retinopathy is unknown. The association between individuals with a Type A personality or individuals under increased emotional strain has been a curious observation.309,326,344 “Stress hormones” such as increased catecholamines and cortisol may lead directly or indirectly to central serous retinopathy.345,346,347 Primate animal studies exposing epinephrine to choroidal vasculature result in local vasoconstriction serving as a possible model by which stress and the resulting glucocorticoid and catecholamine release potentiate the risk of central serous retinopathy in at-risk patients.324,325,348,349,350,351
Clinical features
Patients affected with central serous retinopathy may be asymptomatic or may report decreased vision, metamorphopsia, scotoma, and micropsia.352 Clinically, any of the following features may be consistent with central serous retinopathy:
Neurosensory retinal detachments may be diagnosed as round, oval, blister-like elevations. When the foveal region is affected, the normal foveal reflex is blunted or even absent. Occasionally, yellow subretinal fibrinous precipitates may be present, reminiscent of pseudovitelliform lesions. An atypical presentation is noted in certain predisposed patients. Those on systemic corticosteroid medications may be at greater risk for bullous serous retinal detachments that may be confused with rhegmatogenous retinal detachments in pseudophakic patients.363,364,365,366,367
Pigment epithelial detachments are also round, blister-like elevations as seen in neurosensory detachment, except that the underlying retinal pigment epithelium is detached. They may be so small as to escape detection on biomioscropy, thus the useful application of fluorescein angiography. Pigment epithelial detachments may be seen in isolation or in concert with overlying neurosensory detachment.
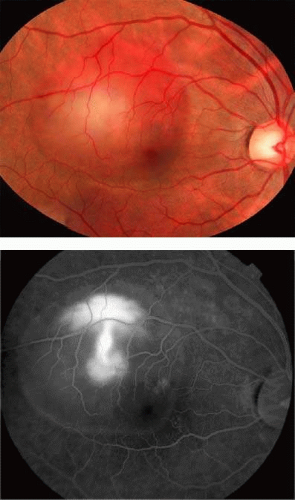
Retinal pigment epithelium atrophy occurs as the various serous detachments resolve. Atrophic changes are not specific to central serous retinopathy. Certain patterns of atrophy, specifically atrophic “tracts” or “guttering” are almost pathognomic of central serous retinopathy. Tracts or guttering are the consequence of gravity dependent shifts in subretinal fluid that progress to extramacular atrophic changes. These may be linear and are often noted predominantly in the inferior hemisphere357(Fig. 23.15).
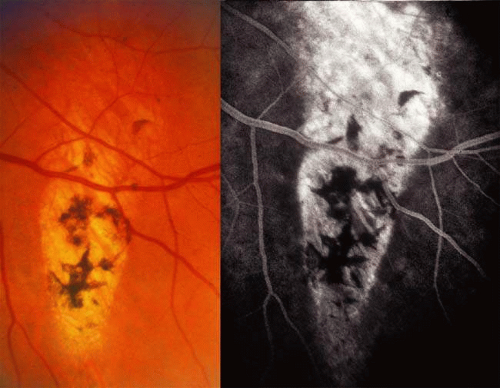 FIGURE 23.15 Atrophic RPE tracts in central serous chorioretinopathy. Angiography (right) demonstrates fluorescence from the underlying choroids secondary to RPE transmission defects. |
The differential diagnosis of serous retinal detachment includes any disease resulting in choroidal neovascularization, including macular degeneration, multifocal choroiditis, ocular histoplasmosis, and idiopathic choroidal neovascularization. Other causes of serous detachment include Harada’s disease, uveal effusion syndrome, and optic nerve pit. Patients presenting with retinal pigment atrophy should be evaluated for macular degeneration, pattern macular dystrophies, resolved rhegmatogenous detachment, and resolved Harada’s disease.
The clinical course is classically described as a self-limited disease with good prognosis of visual acuity retention. Typically, resolution occurs by about 3 to 4 months. However, recurrences are common in up to 49% of patients with 10% experiencing multiple recurrences.342 In a minority of patients, visual acuity suffers when atrophic areas invade the fovea, cystoid macular edema occurs, or if choroidal neovascularization arises.338,362,368,369
Women afflicted with central serous retinopathy warrant special consideration. Perkins et al. described the features of 84 eyes of 78 women diagnosed with central serous retinopathy.339 Central serous retinopathy was associated with subretinal precipitates, short duration (less than 5 months), absence of pigment epithelial detachment were associated with favorable prognosis, whereas those presenting with age older than 50 years or pigment epithelial detachment were likely to suffer extended clinical courses.339
Specific conditions are associated with increased rates or severity of central serous retinopathy and thus warrant discussion. Patients who are administered corticosteroids in almost any form may experience either acute central serous retinopathy or exacerbation of pre-existing retinopathy.331,332,370,371,372 As early as 1966, Jain described the association between corticosteroids and central serous retinopathy.373 Since that time, epidural, intranasal, intramuscular, oral, intravenous, and topical corticosteroid uses have been reported to induce or exacerbate central serous retinopathy.332,333,334,374
Ancillary Tests
Fluorescein angiography in classically described cases reveals focal hyperfluorescence with leakage into the subretinal space. In 7% to 20% of patients, a “smokestack” appearance is noted, hypothesized as an osmotic gradient that develops due to proteinaceous fluid315,370,375,376 (Fig. 23.16). Leakage sites have been noted in all quadrants with the superior nasal quadrant being the most frequently involved quadrant. Angiography typically depicts pigment epithelial detachments as homogenous, well circumscribed, and hyperfluorescence maintained throughout the angiogram.315,370,375,376 (Fig. 23.17). Atrophic areas are easily revealed with transmission of normal choroidal fluorescence.362 Optical coherence tomography is effective in revealing neurosensory detachment and pigment epithelial detachment.377 OCT may underestimate the extent of involvement of atrophic extramacular retinal pigment epithelial tracts.
Treatment
Given the benign clinical course in most patients, characterized by resolution and retention of vision of better than 20/40 in the majority of patients, the recommended treatment is typically limited to observation.342 Laser photocoagulation has been shown to increase the rate of resolution of neurosensory retinal detachment but has not shown to improve visual outcomes at follow up.378,379,380,381 Thus, specific recommendations regarding treatment recommendations are not available. Patients with persistent detachment, occupational needs, and poor visual acuity due to central serous retinopathy in the fellow eye may elect to receive treatment.
Yannuzzi et al. reported the outcomes of patients who received verteporfin and photodynamic therapy for chronic or persistent central serous retinopathy.382,383 The treatment was administered with the aid of indocyanine angiographic guidance. Twenty eyes of 15 patients were treated with PDT directed to areas of choroidal hyperpermeability detected via indocyanine green angiography. Treatment was associated with complete resolution of exudative macular detachments in 12 patients and incomplete resolution in the remaining 8 eyes. The vision improved in 6 eyes and remained unchanged in 14 eyes during a mean follow-up of 6.8 months.383
Ocular Histoplasmosis Syndrome
Synonyms: Presumed ocular histoplasmosis
Introduction
In 1942, Reid et al. described ocular abnormalities in a dying patient with acute disseminated histoplamsosis.384 Subsequently, other investigators reported chorioretinal lesions associated with histoplasmin skin testing. Woods et al. described 62 patients with histoplasmin reactivity, 19 of which demonstrated ocular lesions consisting of atrophic lesions now recognized as “histo spots.”385
The etiology of ocular histoplasmosis is believed to begin with infection of the respiratory tract with Histoplasma capsulatum, early in life.386,387,388,389,390 The fatal cases of histoplasmosis were typically the result of disseminated infection, associated with deficiencies in the immune system of the host. Histoplasmosis has the potential to affect almost all organ systems. Due to its proclivity to the immunocompromised patient, histoplasmosis is a common opportunistic infection in those with acquired immunodeficiency syndrome (AIDS).391
Comstock et al. outlined a rough triangle with apices near Omaha, Nebraska; Columbus, Ohio; and Natchez, Mississippi, which include the Ohio and Mississippi river valleys as the endemic areas of histoplasmosis.392 In this triangle, up to 60% of lifelong residents react positively to histoplasmin skin testing.
Presumed Versus Confirmed Ocular Histoplasmosis
Historically, the term presumed ocular histoplasmosis syndrome was used in the description of the disorder as the causative microbe was never confirmed in blood or tissue culture. A causal relationship between Histoplasma capsulatum and the ocular histoplasmosis syndrome was suggested given reactions to histoplasmin skin testing more commonly observed among patients who have disciform lesions than among controls.386,388,389,393 Reactivation of apparently quiescent lesions of ocular histoplasmosis coincident with positive histoplasmin skin testing has been reported. Finally, Spencer extracted DNA from H. capsulatum isolated from the enucleated eye of a man with chronic choroidal lesions diagnosed as ocular histoplasmosis.394
One study in Walkersville, Maryland, identified 22 subjects of 842 with characteristic ocular histoplamsosis.393 All 22 reacted positively to the histoplasmin skin antigen compared with 59% of the general population with a p value for this association of 0.06 by the Fisher exact test. Of those who tested positive by skin reaction to H. capsulatum, 4.4% had clinical POHS.393
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree