General Ocular Evaluation
CHAPTER CONTENTS
VISUAL ACUITY ASSESSMENT
Methods
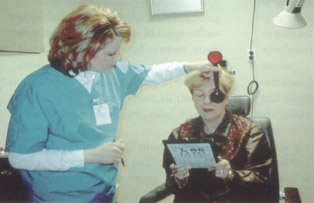
- Measure uncorrected distance, near, monocular, and binocular visual acuity. (Fig. 5-1).
- Measure best corrected visual acuity (BCVA) for distance, near, monocular, and binocular vision with patient wearing prescribed spectacles or contact lenses (if applicable).
- Measure and document acuity preoperatively and at all postoperative evaluations for statistical assessment, progression analysis, and medicolegal documentation.
- Carefully educate patients with reduced acuity because of pathology or amblyopi that refractive surgery probably will not improve their BCVA.
Postoperative Patient Management
- Show documentation of a patient’s preoperative uncorrected visual acuity to help provide perspective if he or she is unhappy with the postoperative result.
- Compare a patient’s pre- and postoperative BCVA to reassure the patient that his or her best corrected vision has not changed.
- Extreme myopes may have decreased acuity with spectacle correction because high-power minus lenses minify the size of objects in the spectacle plane.
- Wearers of hard or soft contact lenses may suffer decreased acuity because of poor-fitting lenses or undesirable tear film/contact lens interactions.
- Refractive surgery may improve acuity compared with spectacles or contact lenses but is not guaranteed.
EYE DOMINANCE TESTING
Indications
- manifest refraction binocular balance testing [the dominant eye is left with “clearer” vision when equal balance unobtainable for both eyes (see Chapter 6)]
- crucial for surgically created monovision (the dominant eye is almost always corrected for distance vision, and the non-dominant eye is targeted for near or intermediate vision)
- confirmation or identification of a patient’s dominant eye
Methods
- Ask the patient which eye he or she uses to look through a telescope or focus a camera (identified eye usually dominant).
- Perform some or all of the specific methods discussed below.
Pointing
The use of pointing to determine a patient’s dominant eye is simple but obtained results may be unreliable.
Methods
- Instruct the patient to leave both eyes open and point at a distant object using an index finger and with the arm fully extended.
- If the object becomes displaced relative to the finger when the patient closes one eye, then the patient closed the dominant eye, but if the object did not become displaced, then the closed eye is nondominant.
- Repeat this test to confirm results.
Framing
The framing method of determining a patient’s dominant eye is simple to perform but may provide ambiguous results.
Methods
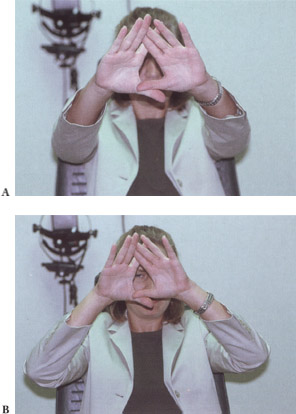
- A patient uses both hands (thumbs and index fingers) to create a triangle-shaped “frame” around a readily identifiable, small, distant object (Fig. 5-2A).
- With arms fully extended and both eyes open, the patient frames the object and then brings both hands toward the face moderately quickly, keeping both eyes open with the distant object sighted and in focus the entire time (Fig. 5-2B). (The patient should frame the dominant eye.)
- If the patient cannot perform this task without seeing the distant object as “double,” then the patient may be partially or totally ambiocular (i.e., without a strongly dominant eye).
- Instruct the patient to repeat the procedure to confirm results.
Hole Card
This test uses the same principle as the framing method but may also provide ambiguous results.
Methods
- Create the hole card by punching a hole in the center of a small, square piece of paper (about the size of a prescription pad).
- Instruct the patient to hold the card with both hands and with arms extended.
- Ask the patient to sight a small, designated, distant object through the hole in the card with both eyes open.
- Ask the patient to bring the hole card swiftly back toward his or her face, keeping the object in focus and leaving both eyes open. (The patient should bring the hole card back to the dominant eye.)
- If the patient cannot sight the object through the hole without seeing “double,” the patient may be partially or totally ambiocular.
- Repeat this test several times to confirm the dominant eye.
Four Base Out Test
The pointing, framing, and hole card tests may yield ambiguous results, but the four base out (BO) test provides definitive results.
Methods
- Place a four prism diopter lens BO over the patient’s suspected dominant eye while the patient fixates with both eyes on a distant object (Fig. 5-3).
- Next, place the 4Δ BO prism over the suspected nondominant eye with the patient fixating on the same distant object.
- If this is truly the patient’s nondominant eye, the examiner should note little to no eye shift in the opposite (dominant) eye.
- If the examiner has difficulty detecting eye shift versus no eye shift when presenting the prism to either eye, try increasing the prism amount to elicit a more substantial reaction.
- If this is truly the patient’s nondominant eye, the examiner should note little to no eye shift in the opposite (dominant) eye.
- If the 4Δ BO test and the other eye dominance tests yield conflicting results, then consider the patient to be ambiocular. (Generally, ambiocular patients do not accept monovision well and should be considered very cautiously as monovision candidates.)

MONOVISION CONSIDERATIONS
Preoperative Considerations
- the patient’s personality, age, hobbies, and goals for refractive surgery
- determination of monovision target power (allows a patient adequate near/intermediate vision while maintaining acceptable distance vision)
- testing of patients who use computers regularly by using the patient’s habitual computer font size and working distance at a computer terminal
- realistic patient expectations about surgical results
- ambiocular patients (of 1 in 10 patients in general population unable to accept any level of monovision, most are difficult to measure and quantify; see Eye Dominance Testing)
- patient preference of the dominant eye for near vision (should be attempted only with careful trials and documentation and after performing a trial run of monovision with contact lenses)
- previous monovision failure
- possible success with surgical monovision for patients with previously unsuccessful monovision contact lenses (may have been caused by dry eyes, poor lens fit, inaccurate lens powers, or improper eye selection)
- consider cautiously as surgical candidates until proven otherwise
- requires preoperative trial frames for motivated patients
- possible success with surgical monovision for patients with previously unsuccessful monovision contact lenses (may have been caused by dry eyes, poor lens fit, inaccurate lens powers, or improper eye selection)
- patient education
- discussion of advantages and compromises of monovision with all presbyopic patients and those older than 40 years, the average age of onset for presbyopia (highly motivated patients < 40 years old may be considered if thoroughly educated and intent on undergoing the procedure)
- the possible reversibility of monovision with enhancement surgery if monovision unacceptable [most applicable for radial keratotomy (RK), photorefractive radial keratectomy (PRK), and laser in situ keratomileusis (LASIK) myopic candidates who are intentionally undercorrected in one eye to create monovision]
- notification of the possible postoperative adjustment period that lasts from one to several weeks and may be disorienting
- advantages (lifelong decreased or eliminated dependence on spectacles for near and intermediate tasks)
- disadvantages (possible scotopic halos and glare, compromised depth perception in dim lighting that may be alleviated by thin night-driving eyeglasses)
- discussion of advantages and compromises of monovision with all presbyopic patients and those older than 40 years, the average age of onset for presbyopia (highly motivated patients < 40 years old may be considered if thoroughly educated and intent on undergoing the procedure)
- documentation of the discussion about monovision
- the patient’s decision for or against monovision
- the patient’s understanding of possible consequences of his or her choice (e.g.,possibility of increased night glare vs.need for reading glasses)
- the patient’s decision for or against monovision
Monovision Trial Framing
Indications
- identification of poor monovision candidates before surgically creating monovision (Fig. 5-4)
- determination of monovision target powers

Methods
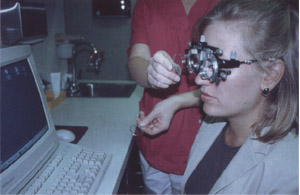
- Place the patient’s manifest refraction result for each eye in the trial frame.
- Place an occluder lens in the trial frame over the patient’s dominant eye (see Eye Dominance Testing for methods).
- Instruct the patient to look at a near vision card, and place a plus lens (for monovision) over the unoccluded eye.
- Select the power of the plus lens based on the patient’s age (from +1.00 D at 40 years of age to +2.00 D at 55 years of age) and visual goals (e.g., small near tasks like threading a needle or general intermediate tasks such as seeing a computer).
- After acknowledging the patient’s ability to see the near card, remove the occluder lens from the trial frame over the patient’s dominant eye to allow the patient to see binocularly in monovision
- The patient initially may report ghosting or doubling of the near letters with binocular monovision in the trial frame (often occurs if the optical center is off in the trial frame lenses).
- Instruct the patient to shift the near card slightly to attempt to remove the ghosting.
- The patient initially may report ghosting or doubling of the near letters with binocular monovision in the trial frame (often occurs if the optical center is off in the trial frame lenses).
- Next, allow the patient to experience monovision at various distances with the trial frame by having the patient walk around with a technician.
- Try various monovision target powers with the patient (Fig. 5-5).
- For example, if a 46-year-old patient has an initial monovision target of +1.50 D but does not see a computer screen well with this lens, the technician should try a target of +1.00 D at the computer).
- If more acceptable to the patient and agreeable with the patient’s goals, adjust the target.
- If a patient chronically experiences significant ghosting of near letters or experiences outright diplopia or nausea that does not subside, the patient will probably not tolerate monovision.
- Single-vision soft contact lenses (for patients who have essentially spherical refractive errors) are an easy, inexpensive way to allow refractive surgery candidates to experience monovision in their own home or work environment.
- Try various monovision target powers with the patient (Fig. 5-5).
PUPILLOMETRY
Indications
- identification of patients with physiologically large pupils
- may warrant patient counseling about possible irreversible night-glare symptoms after RK or laser refractive surgery procedures
- may have problematic glare symptoms because of small clear, corneal optical zones created by incisions during surgery (specifically RK)
- may experience induction of glare, halos, or “star bursting” with laser ablation zone sizes smaller than scotopic pupil sizes (with PRK and LASIK)
- may have problematic glare symptoms because of small clear, corneal optical zones created by incisions during surgery (specifically RK)
- determination of likelihood of patient complaints (few complain about nocturnal vision 3 months postoperatively although occasionally a patient with normal or smaller than average pupils complains of poor night vision associated with the procedure, even when all objective tests are within normal limits)
Pupil Card
This is probably the easiest and least expensive method for evaluating pupil size but may be less accurate than other methods.
Methods
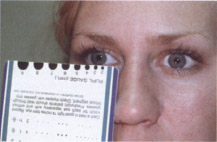
- Simply line up semicircles (usually ranging from 1.0 to 10.0 mm in increments of 1.0 mm) at the vertical midpoint of the patient’s pupil and determine which semicircle on the card best represents the patient’s pupil size (Fig. 5-6).
- Record corresponding measurements from the pupil card in both photopic (light) and mesopic (dim) conditions.
Holladay-Godwin Pupil Gauge
This gauge (American Surgical Instrument Corporation, Westmont, IL) was designed to make pupil measurement simple and accurate.
Methods
- Use this gauge in the same manner as the pupil card.
- Measure pupil sizes larger than 0.5 mm in scotopic and mesopic conditions by comparing actual pupil size with the full circles and semicircles on the gauge (from 1.0 to 10.0 mm in increments of 0.5 mm) (Fig. 5-7A).

Figure 5-7 (A) The Holladay-Godwin pupil gauge. (B) The Colvard pupil gauge.
Colvard Pupillometer
This hand-held, battery-operated pupillometer from Oasis (Glendora, CA) preoperatively evaluates and measures the scotopic and photopic pupil size. It allows accurate visualization of the pupil in a darkened examination room by incorporating light amplification technology for accurate scotopic measurements (Fig. 5-7B).
SLIT-LAMP EXAMINATION
Indications
- preoperative identification of pterygium (ideally, elimination of it prior to any corneal surgery)
- identification of corneal neovascularization or pannus (significant intraoperative bleeding may occur during corneal procedures with either of these)
- identification of corneal endothelial pigment spindles (may indicate future or current pigment dispersion, glaucoma)
- preoperative documentation of intraocular pressure (IOP) (future readings will be lower than preoperative values by approximately 1.5 mmHg/100 μm of ablated tissue for laser procedures during which significant corneal tissue is removed)
- identification of inactive corneal opacities and/or scars and assessment of their impact on visual acuity (Fig. 5-8; see Chapter 3)
- identification of dry eye or keratoconjunctivitis sicca (if severe, then may be contraindications for corneal surgery)
- recognition of anterior basement membrane dystrophy (may complicate LASIK procedures intraoperatively or delay visual recovery with any refractive surgery procedure) (see Chapter 3)
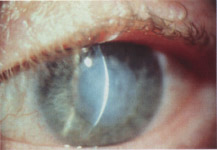
Figure 5-8 Central corneal scars or opacities must be evaluated for their impact on visual acuity.
Relative Contraindications for Surgery
- corneal disease
- prior corneal surgery
- specific orbit configurations
- abnormal eyelid closure (lagophthalmos) because of increased risk for delayed corneal healing
- poorly healed corneal scars (may ablate more easily than surrounding tissue)
- signs of prior herpes simplex or zoster keratitis (because of reduced corneal sensitivity and potential for reactivation of infection)
Absolute Contraindications for Surgery
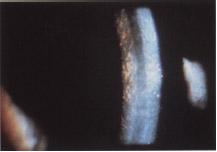
- endothelial dystrophies (such as Fuchs’s dystrophy or severe gutatta with a total cell count < 1500) (Fig. 5-9; see Chapter 3)
- increased risk for future corneal edema and decompensation (bullous keratopathy)
- particularly worrisome with clear lens extraction refractive surgery (associated with a 4-8% cell loss during the procedure)
- increased risk for future corneal edema and decompensation (bullous keratopathy)
- any active anterior segment infectious or inflammatory process (must be completely resolved preoperatively)
- keratoconus with or without Vogt’s stria or Fleischer’s ring (Fig. 5-10) (for any corneal refractive surgical procedure)
FUNDUS EXAMINATION
Indications
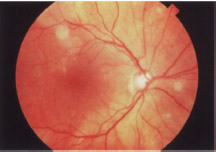
- identification and discussion of macular pathology such as pathological myopic degeneration, age-related macular degeneration, or diabetic retinopathy (Fig. 5-11) (discussion with patient warranted if pathology has already affected visual function because refractive surgery will not increase the patient’s BCVA)
- identification of patients with prior vitreoretinal, cataract, or strabismus surgery (may complicate refractive surgical procedures such as LASIK or clear lens extraction)
- identification of significant vitreal syneresis or lattice degeneration associated with traction or holes (may complicate LASIK or clear lens extraction refractive surgical procedures)
- identification of severe glaucoma or other optic nerve disorders (consider on a case-by-case basis) (Fig. 5-12)
- IOP rises transiently during LASIK surgery
- poor long-term visual prognoses of severe glaucoma with any refractive surgical procedure
- IOP rises transiently during LASIK surgery
- identification of retinitis pigmentosa (consider on a case-by-case basis with emphasis on patient counseling)
- aggravation of the associated attenuated vasculature and optic nerve changes because of marked transient rise in IOP during LASIK
- inhibition of night vision in patients with retinitis pigmentosa after other refractive surgical procedures, including LASIK
- aggravation of the associated attenuated vasculature and optic nerve changes because of marked transient rise in IOP during LASIK
- identification and evaluation of posterior staphyloma using ultrasonography particularly when considering clear lens extraction (see Chapter 7)

Figure 5–10 Fleischer’ ring seen around the base of the cone in a patient with keratoconus.
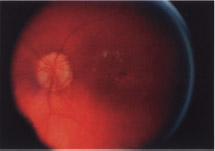
Figure 5-11 Macular degeneration has not yet affected visual acuity in this patient.
Suggested Readings
Assil KK, Schanzlin DJ. Radial and Astigmatic Keratotomy: A Complete Handbook. St. Louis: Poole Press; 1994.
Carlson NB, Kurtz D, Heath DA, Hines C. Clinical Procedures for Ocular Examination. Norwalk, CT: Appleton & Lange; 1990.
Machat JJ, Slade SG, Probst LE. The Art of LASIK. 2nd ed. Thorofare, NJ: Slack Inc.; 1999.
< div class='tao-gold-member'>



