Cyclodestructive Surgery
The operations discussed in the preceding chapters lower the intraocular pressure (IOP) by improving the rate of aqueous outflow. This is clearly preferred from a physiologic standpoint, in that the aqueous humor can continue to be produced in an unaltered state and fulfill its various functions, including nourishment of intraocular tissues. An alternative approach to reducing IOP, however, is to decrease the rate of aqueous production by partially eliminating the function of the ciliary processes. Historically, these techniques were rarely the first operation of choice, because the results are hard to predict and the complication rate is high because of damage to adjacent ocular structures and the influence of a pronounced inflammatory response. Newer approaches with transscleral and endoscopic diode laser appear to be associated with reasonable efficacy and fewer vision-threatening complications and may be considered earlier in the treatment paradigm.
Cyclodestructive procedures constitute a valuable adjunct in our surgical armamentarium for eyes in which other operations have failed or when the surgeon wishes to avoid incisional surgery, such as in eyes with limited visual potential or with a high risk for intraocular complications with standard outflow procedures. An important exception is endoscopic cyclophotocoagulation (ECP), a procedure that may be a useful adjunct in eyes with reasonable visual potential and whose indications are still evolving.
OVERVIEW OF CYCLODESTRUCTIVE PROCEDURES
Cyclodestructive operations differ according to (a) the destructive energy source and (b) the route by which the energy reaches the ciliary processes. In the 1930s and 1940s, several energy sources were evaluated, including diathermy, β-irradiation, and electrolysis, although only cyclodiathermy achieved clinical acceptance. Cryotherapy was introduced in the 1950s and became the most commonly used cyclodestructive procedure. However, subsequent experience with laser cyclophotocoagulation showed clear advantages over other techniques, and it has become the preferred cyclodestructive operation. Other cyclodestructive techniques include therapeutic ultrasonography and microwave cyclodestruction. Each of these energy sources may be delivered by the transscleral route, in which the destructive element passes through conjunctiva, sclera, and ciliary muscle before reaching the ciliary processes. Transscleral cyclodestructive operations have the advantages of being nonincisional and relatively quick and easy. However, significant disadvantages include the inability to visualize the processes being treated and damage to adjacent tissue, leading to unpredictable results and frequent complications. With the advent of laser energy as the cyclodestructive element, alternative delivery routes, including transpupillary and endoscopic approaches, are now possible.
EARLY CYCLODESTRUCTIVE PROCEDURES
Penetrating Cyclodiathermy
Weve (1) introduced the concept of cyclodestructive surgery in 1933, using nonpenetrating diathermy to produce selective destruction of ciliary processes. Vogt (2,3) modified the technique by using a diathermy probe, which penetrated the sclera, and this became the standard cyclodestructive procedure. One or two rows of diathermy lesions were generally placed 2.5 to 5 mm behind the limbus several millimeters apart for approximately 180 degrees. Early reports of experience with cyclodiathermy were encouraging (4,5). However, subsequent study revealed a low success rate (about 5%) and a significant incidence of hypotony and phthisis (about 5%) (6).
Other Early Cyclodestructive Procedures
β-Irradiation Therapy
In 1948, Haik and coworkers (7) reported the experimental application of radium over the ciliary body in rabbit eyes and in one clinical case. Although this was shown to produce a reduction in the vascular supply of the ciliary body, it also caused damage to the lens, and the technique was never adopted for clinical use.
Cycloelectrolysis
Berens and coworkers (8) in 1949 described a technique that used low-frequency galvanic current to create a chemical reaction within the ciliary body. This led to the formation of sodium hydroxide, which is caustic to the tissue of the ciliary body. Although this was shown in rabbit studies to produce destruction of ciliary processes (9), the procedure did not seem to have significant advantages over penetrating cyclodiathermy and never achieved widespread clinical popularity.
Therapeutic Ultrasonography
In 1964, Purnell and associates (10) introduced the concept of using focused transscleral ultrasonic radiation to produce localized destruction of the ciliary body in rabbit eyes. Coleman and coworkers in 1985 reported the results of rabbit studies and preliminary clinical trials with high-intensity focused ultrasound (11,12). Several clinical trials of therapeutic ultrasonography in patients with refractory glaucomas, similar to those described in studies of other cyclodestructive procedures, have revealed IOP reduction to the low 20s (mm Hg) or less in one half to two thirds of the cases 6 to 12 months after a single treatment (13–15). In a multicenter study involving 880 eyes, success (IOP between 6 and 22 mm Hg) after a single treatment was 48.7% at 6 months (16). With repeated treatments as required, the success rate rose to 79.3% at 1 year. The most common complication was an immediate postoperative IOP increase and mild iritis. Scleral thinning was observed in 2.5%, and phthisis in 1.1%. Decreased visual acuity occurred in approximately 20% of the cases.
Transscleral Microwave Cyclodestruction
The direct application of high-frequency electromagnetic radiation over the conjunctiva in rabbits produced heat-induced damage to the ciliary body with relative sparing of the conjunctiva and sclera (17). In rabbits with experimentally induced glaucoma, the procedure was successful in reducing IOP in all treated eyes for 4 weeks (18).
Excision of the Ciliary Body
In addition to the use of many cyclodestructive elements, as described earlier, other surgeons have sought to reduce aqueous production by removing a portion of the ciliary body. Several studies have revealed reasonable success and complication rates with this basic approach in eyes with unusually refractory glaucomas (19–21).
LASER CYCLODESTRUCTION
Transscleral Cyclophotocoagulation
In 1961, Weekers and associates (22) used light as the cyclodestructive element, using the transscleral application of xenon-arc photocoagulation over the ciliary body. As with other operations that use light energy, however, it was the introduction of the laser that eventually led to the clinical application of cyclophotocoagulation. In 1969, Vucicevic and associates (23) reported the use of a ruby laser to perform transscleral cyclophotocoagulation in rabbits, with an adjunctive cytochemical agent to enhance laser absorption by the ciliary body. Other reports of transscleral laser cyclophotocoagulation followed (24–26), and in 1984 Beckman and Waeltermann (27) reported results of a 10-year experience with 241 eyes treated by using transscleral ruby laser cyclophotocoagulation. Their overall rate of IOP control was 62%, with 86% in aphakic eyes with glaucoma and 53% in eyes with neovascular glaucoma. Chronic hypotony occurred in 41 eyes, with phthisis in 17 cases, although most eyes retained their preoperative level of vision. However, it was not until the availability of specially designed Nd:YAG (neodymium:yttrium–aluminum– garnet) and, subsequently, semiconductor diode lasers that widespread interest in transscleral cyclophotocoagulation developed.
Instruments
Nd:YAG Lasers
Nd:YAG lasers, with a wavelength of 1064 nm, have been useful for transscleral cyclophotocoagulation because they traverse the sclera with relatively low absorption and scatter. They may be operated in a pulsed, free-running, thermal mode, or a continuous-wave mode, and may be delivered by either a noncontact, slitlamp system, or a contact probe, fiberoptic system. However, these units do not appear to be commercially available for transscleral cyclophotocoagulation. (Readers wishing more information can consult the fifth edition of this book.)
Semiconductor Diode Lasers
Although semiconductor diode lasers, with a range of wavelengths between 750 and 850 nm, do not traverse the sclera as efficiently as Nd:YAG lasers do, they have the advantage of greater absorption by uveal melanin. In addition, they have the advantage of solid-state construction with compact size, low maintenance requirements, and no special requirement for electric outlet or water cooling.
The Oculight SLx (Iris Medical Instruments) is a continuous-wave, contact delivery diode laser with a wavelength of 810 nm, a maximum power output of 2.5 to 3.0 W, and a maximum duration of 9.9 seconds (28–30) (Fig. 41.1). The probe (G-Probe) consists of a 600-µm quartz fiberoptic, protruding 0.7 mm from a handpiece, which is fabricated to center the fiberoptic 1.2 mm behind the surgical limbus and parallel to the visual axis (30). The back of the G-Probe pushes the lid away from the surgical site, and the sides can be used to aid in spacing the laser applications (Fig. 41.2).


Figure 41.1 A: Semiconductor diode laser (IRIS, Oculight, SLx, Iris Medical Inc., Mountain View, CA) for transscleral diode cyclophotocoagulation.B: G-Probe handpiece for transscleral diode cyclophotocoagulation. (From Lin SC. Endoscopic and transscleral cyclophotocoagulation for the treatment of refractory glaucoma. J Glaucoma. 2008;17: 238–247.)

Figure 41.2 Transscleral diode cyclophotocoagulation, showing use of G-Probe to position fiberoptic 1.2 mm from surgical limbus and to space adjacent laser applications.
An ophthalmic laser microendoscope (Endo Optiks Inc., Little Silver, NJ) has also been developed which houses fiberoptics for a video monitor, diode laser endophotocoagulation, and illumination in a 20-gauge probe (31) (Fig. 41.3). The diode laser has 1.2 W of power output and is focused visually by means of a 670 nm (2.0 mW) laser aiming beam. Optimal focal distance for the laser is 0.75 mm from the tip of the probe. Depth of focus while viewing is from 0 to 20 mm, and the camera lens has a 70-degree field of view.

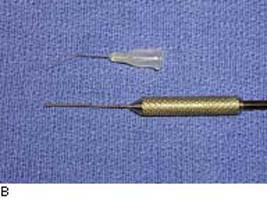
Figure 41.3 A: An ECP unit (Uram E2, Endo Optiks, Little Silver, NJ), including laser, monitor, and foot pedal.B: An ECP probe (20 gauge). A 27-gauge cannula tip is shown above for size comparison. (From Lin SC. Endoscopic and transscleral cyclophotocoagulation for the treatment of refractory glaucoma. J Glaucoma. 2008;17: 238–247.)
Krypton Lasers
Transscleral cyclophotocoagulation has also been performed with a retinal krypton laser, delivered by a contact probe. The shorter wavelength results in poorer scleral transmission but better uveal pigment absorption than with the Nd:YAG laser, and histologic lesions in rabbits were similar with the two lasers (32). Successful clinical results were reported, using 4 to 5 J of energy, 10-second exposures, and firm compression with the probe (33,34).
Theories of Mechanism
The mechanism by which transscleral cyclophotocoagulation reduces IOP is not fully understood. The prevailing theory is that it reduces aqueous production by damaging the pars plicata, although it is unclear whether this is due to direct destruction of the ciliary epithelium or reduced vascular perfusion. Still other investigators suggest that the primary mechanism may be increased outflow through an effect on the pars plana.
Evidence for Reduced Aqueous Production
Rabbit studies have demonstrated that transscleral application of Nd:YAG laser energy results in coagulative necrosis of the ciliary epithelium, including destruction of ciliary vessels in the overlying area (35).
Studies of human autopsy eyes revealed structural changes of the ciliary body similar to those seen in rabbits. The gross appearance of lesions created by the noncontact, free-running Nd:YAG laser was a white elevation of the ciliary epithelium (36). The histologic correlate was a blister-like elevation of the epithelial layers from the adjacent stroma, with marked disruption primarily of the pigmented epithelium but minimal change in the ciliary muscle and sclera in the path of the laser beam (37,38) (Fig. 41.4). In contrast, the histologic appearance of lesions created by the contact, continuous-wave Nd:YAG laser was a smaller, more coagulative effect on the epithelium with less of the blister-like elevation (38,39). One study showed a more full-thickness thermal effect, including sclera (38), while another showed no scleral alteration (39). A videographic study of human autopsy eyes also showed that shorter-duration Nd:YAG laser exposures caused greater tissue disruption, whereas the more prolonged, continuous-wave exposures produced a more coagulative, shrinkage-like lesion (40).
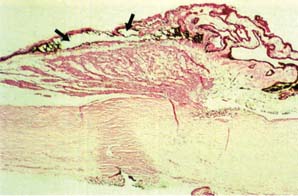
Figure 41.4 Light microscopic view of human autopsy eye treated with transscleral thermal, pulsed Nd:YAG cyclophotocoagulation showing blister-like elevation of disrupted ciliary epithelium (arrows) with minimal ciliary muscle and scleral damage. Defect on scleral surface was created by needle with India ink to mark center of laser track after laser application.
Histologic studies have also been performed on human eyes that were enucleated at some point after transscleral Nd:YAG cyclophotocoagulation. In one series of eyes treated with the noncontact, free-running Nd:YAG laser a few days before scheduled enucleation, the structural changes were the same as those seen in human autopsy eyes with the addition of fibrin and scant inflammatory cells between the disrupted epithelial layers and stroma (41). No changes in ciliary body vasculature were observed. A clinicopathologic study of three eyes enucleated 2 weeks, 8 weeks, and 17 months after noncontact Nd:YAG cyclophotocoagulation revealed destruction of the nonpigmented and pigmented ciliary epithelium, occlusion of capillaries, and stromal necrosis, with subsequent hyperplasia of the epithelial layers, fibrosis, and near–total atrophy of the ciliary processes (42). Histologic evaluation of another eye, which had received the same laser treatment 70 days before enucleation for hypotony and pain, revealed pigment disruption and granulomatous inflammation of the ciliary body (43). Two eyes treated with contact, continuous-wave Nd:YAG transscleral cyclophotocoagulation 1 day before enucleation for melanomas revealed epithelial necrosis and partial capillary thrombosis of the ciliary body with slight scleral damage (44).
Histologic observations with both light microscopy and scanning electron microscopy reveal that tissue treated with transscleral diode cyclophotocoagulation shows pronounced tissue disruption of the ciliary body muscle and stroma, ciliary processes, and both pigmented and nonpigmented ciliary epithelium. ECP-treated tissue, however, only exhibits pronounced contraction of the ciliary processes with disruption of the ciliary body epithelium, sparing of the ciliary body muscle with less architectural disorganization (Fig. 41.5) (45). A study of vascular effects of transscleral compared with ECP in rabbits demonstrated immediate and severely reduced or nonexistent blood flow in the areas of treatment after both types of procedures (46). After 1 week and 1 month, however, transscleral-treated processes remained nonperfused, whereas ECP processes showed some reperfusion that increased over time. The authors concluded that chronic poor perfusion of the ciliary after transscleral diode cyclophotocoagulation may partly account for its efficacy and the significant complications, including hypotony and phthisis. Late reperfusion of this region after ECP may provide some insight into the differences in efficacy and complication rates, compared with transscleral diode cyclophotocoagulation.
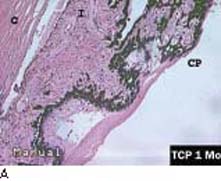
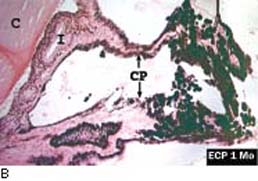
Figure 41.5 A: Histopathology of rabbit ciliary processes 1 month after contact transscleral diode cyclophotocoagulation. Note coagulative necrosis of the ciliary tissue with cyclitic membrane formation (×40).B: Histopathology of rabbit ciliary processes 1 month after diode laser ECP. Disruption of ciliary architecture is shown but a relatively normal process with patent vessel is seen to the left (×40). C, cornea; CP, ciliary processes; I, iris. (From Lin SC. Endoscopic and transscleral cyclophotocoagulation for the treatment of refractory glaucoma. J Glaucoma. 2008;17: 238–247.)
Evidence for Increased Aqueous Outflow
Although the aforementioned studies confirm that transscleral cyclophotocoagulation can destroy tissues of the pars plicata, most likely by a direct effect on the ciliary epithelium, this does not prove that direct destruction of the pars plicata is an essential element in the mechanism of IOP reduction. Other studies have shown that more posteriorly placed lesions over the pars plana or even peripheral retina also decrease the IOP (47–50). The explanation for this observation could be reduced aqueous production due to the inflammatory response (47), although it is unlikely that this would be a sustained effect. An alternative explanation is enhanced aqueous outflow, either by transscleral filtration or uveoscleral outflow (48–52). In a monkey study of contact, continuous-wave Nd:YAG cyclophotocoagulation, in which right eyes were treated over the pars plicata, 1 mm behind the limbus, and left eyes were treated over the pars plana, 3 mm behind the limbus, IOP reduction occurred in both eyes but returned to baseline by 8 weeks in the former group, whereas the latter group maintained IOP reduction for the 6-month observation period (51). Histology of the latter eyes suggested enhanced uveoscleral outflow by showing tracer elements in enlarged extracellular spaces of the ciliary stroma from the anterior chamber to the suprachoroidal space. In a similar clinical trial in which laser applications were placed either 1.5 mm or 3.0 to 4.0 mm behind the limbus, the latter group had a higher percentage of eyes with sustained IOP reduction, although they also had received more than twice as many laser applications (52). In another clinical trial using noncontact Nd:YAG cyclophotocoagulation in which all treatment parameters were kept constant except for laser placement 1.5 or 3.0 mm posterior to the limbus, the former group had significantly lower IOP and required fewer repeated treatments during 6-month follow-up (53).
In summary, the most likely mechanism of IOP lowering by transscleral cyclophotocoagulation is reduced aqueous production through destruction of ciliary epithelium. However, alternative possibilities, including reduced inflow due to ciliary vascular disruption or chronic inflammation, or increased outflow due to pars plana–transscleral outflow or enhanced uveoscleral outflow, have not been ruled out.
Techniques
Preoperative and Postoperative Management
Unlike most other glaucoma laser procedures, the intraoperative pain associated with transscleral cyclophotocoagulation is such that retrobulbar anesthesia is required, although this has been omitted by some surgeons with the contact, continuous-wave technique (44). Also, unlike most other laser procedures and other transscleral cyclodestructive procedures, postoperative IOP rise is not a frequent problem, and special preoperative and postoperative measures, such as the use of topical apraclonidine, are usually unnecessary. For ECP, peribulbar, topical, or intracameral anesthesia may be selected.
Postoperative inflammation can be a significant problem, requiring special prophylactic measures. One approach is to give a subconjunctival injection of a short-acting steroid at the end of the procedure and to prescribe topical atropine and steroid for approximately 10 days (54). Use of preoperative glaucoma medications is continued, except for miotics, until IOP reduction allows discontinuation. Postoperative pain is typically mild, and a weak analgesic is usually sufficient. IOP is usually checked a few hours after the procedure, the following day, and then thereafter as required.
Laser Settings and Protocols
The histologic studies with human eyes, as previously described, have been used to establish protocols for clinical trials. However, preferred settings differ among surgeons, and the optimum protocols have yet to be established.
Nd:YAG Noncontact, Thermal Mode, and Continuous Wave. These instruments are no longer available but appear to have a similar mechanism of action as contact, thermal mode lasers.
Semiconductor Diode, Continuous Wave. With the Oculight SLx, the G-Probe footplate is placed on conjunctiva with the short side adjacent to the limbus, which positions the fiberoptic tip 1.2 mm behind the limbus. Initial settings are 1750 mW and 2 seconds (30). If a popping sound is heard with the initial application, the power is reduced by increments of 250 mW until no pop is heard. If no pop is heard with the initial application, the power is increased by the same increments until the sound is heard, and then it is reduced by one increment. Videographic studies of human autopsy eyes have shown that this audible indicator represents excessive tissue destruction, whereas a power setting one increment below this level is believed to provide optimum tissue damage (55). Some surgeons prefer lower power and longer duration burns, such as 1250 mW at 4 seconds in heavily pigmented eyes and 1500 mW at 3.5 seconds in lightly pigmented eyes (56). The laser applications are spaced circumferentially by placing the side of the G-Probe footplate adjacent to the indentation mark of the previous fiberoptic placement. The original protocol involved 17 to 19 applications for 270 degrees (30), although 24 applications for 360 degrees may provide more effective IOP reduction. We suggest avoiding the 3- and 9-o’clock positions because this may reduce the chances of occluding the long posterior ciliary vessels and thus reduce the chance of anterior segment ischemia. This procedure can be performed with the patient supine or reclining in an examination chair or positioned at a standard slitlamp.
The G-probe used with transscleral diode cyclophotocoagulation can be reused several times without loss of power, even if cleaned by alcohol each time (57). More research is needed, however, to determine the best sterilization methods for this probe.
For ECP, a limbal or pars plana approach can be used. In the limbal approach, a paracentesis is created (about 2 mm), usually at the temporal side initially, and the anterior chamber is filled with viscoelastic agent (typically a cohesive viscoelastic such as sodium hyaluronate), which is further used to expand the space between the iris and the intraocular lens. This viscoelastic expansion of the posterior chamber allows for easier approach to the pars plicata with the ECP probe. A pars plana approach is preferred if there is an anterior chamber IOL or if the anterior segment structures are disrupted or the view is not good (e.g., with a failed penetrating keratoplasty graft). The pars plan approach can be used if eyes have received a previous complete vitrectomy, or where simultaneous vitrectomy can be done.
After orientation of the probe image outside of the eye (with black lettering on a ruler, suture pack, or label), the ECP probe is inserted through the incision and into the posterior chamber. At this time, the ciliary processes are viewed on the monitor and the surgeon’s attention can be turned to the monitor (Fig. 41.6). Usually, about five to six processes are viewed and the aiming beam is directed on the apex of the processes. It is important to have the probe oriented as flat as possible (otherwise the aiming beam will focus further posteriorly on the pars plana or ora serrata).
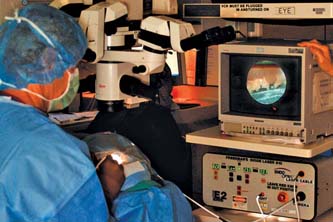
Figure 41.6 Surgeon performing ECP. A video monitor is used to view the ciliary processes during the procedure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


