3
Medical Evaluation of
the Uveitis Patient
John J. Huang and Tracy Wright
Communication with the patient is the cornerstone of the uveitis workup, yielding far more information than any ancillary laboratory or imaging studies. This chapter aims to assist the practitioner in undertaking the patient interview so as to obtain information that is useful in diagnosing and treating ocular inflammatory disease. The process involves careful attention to the patient’s presenting symptoms, history of the presenting illness, medical history, medications, family and social histories, and review of systems (ROS). We discuss each of these elements of the clinical workup with specific references to its potential diagnostic and therapeutic significance. In providing specifics, we naturally risk excluding some worthwhile information. Certainly, the range of circumstances that one could encounter in the clinical setting is nearly endless and exceeds what can reasonably be included in a practical manual like this one. Nevertheless, the specific recommendations offered here are likely to guide the practitioner in approaching the great majority of patients with ocular inflammatory diseases.
PRESENTING SYMPTOMS
Diagnostic Utility of Presenting Ocular Symptoms
For the most part, eye-related symptoms are not nearly as useful as the ocular examination for diagnosing a patient’s ocular inflammatory condition. We are often amazed by the wide range of things that patients report for each type of ocular inflammation, and we really do not find any symptom to be consistently suggestive of a specific ocular or systemic diagnosis, or truly helpful in directing the underlying workup, so we do not “hang our hat” on any symptom during the medical evaluation. Nevertheless, certain observations may be helpful in diagnosing a patient’s uveitis or scleritis.
- Visual loss on presentation generally implies that the patient’s uveitis is long-standing, hence probably chronic, which itself may occasionally narrow the differential diagnosis of various types of ocular inflammation.
- The practitioner can generally ascertain from the patient’s symptoms if the inflammatory process is bilateral, although the findings on complete ocular examination will provide this information definitively.
- Acknowledging the variability in uveitis symptoms, it is generally the case that photophobia indicates inflammation of the iris, hence at least some component of the anterior uveitis. Floaters are often due to vitreous cells and hence suggest that the patient will have at least some vitreitis. Table 3.1 lists symptoms commonly associated with various forms of uveitis and common etiologies of each form. As noted above, a description of current symptoms in terms of location, character, and laterality always relies on the ophthalmologic examination.
Table 3.1 Common ocular symptoms and causes of anterior and posterior uveitis
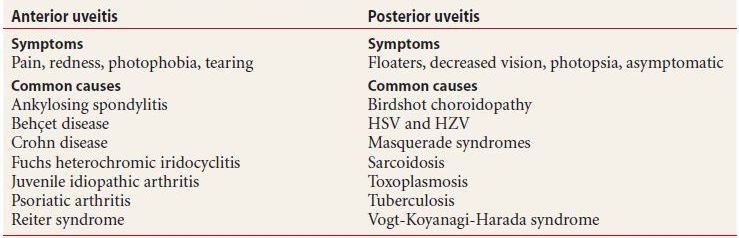
HSV, herpes simplex virus; HZV, herpes zoster virus.
Therapeutic Utility of Presenting Ocular Symptoms
Symptoms are quite significant with regard to therapy:
- Willingness to undergo therapy. It is fair to assume that patients with severe pain or visual loss will be more amenable to undertaking difficult or elaborate treatment regimens than those who are barely bothered by the disease, and we keep this in mind in our discussions with our patients.
- Need for routine monitoring. Patients with symptomatic disease generally seek therapy when their inflammation is active, and for this reason, symptomatic uveitis is unquestionably preferable to indolent, asymptomatic disease. Patients with a history of asymptomatic ocular inflammation usually require more frequent visits to monitor for disease recurrence, since they may not know if their eyes are inflamed.
HISTORY OF PRESENT ILLNESS (HPI)
Diagnostically Useful Elements of the HPI
- Determining chronicity. Patients can often recall the onset of their symptoms, which may help in determining if their inflammation is acute or chronic in nature.
- Determining recurrence. Prior episodes of patients’ current symptoms—even many years prior—suggest that ocular inflammation is recurrent, which is characteristic of certain diseases, including herpetic eye infection and HLA-B27-related iritis.
Patients occasionally attribute their disease to some specific event or describe apparently exacerbating factors for their disease (e.g. psychosocial stress). While we are never quite sure what to do with this sort of information and have yet to find it useful in a direct sense, it sometimes helps us develop an overall mental picture of the patient (who is otherwise usually a complete stranger), and so we listen and document carefully here and keep their comments in mind in structuring a treatment regimen.
Therapeutically Useful Elements of the HPI
- Gauging disease severity. Knowing how long a disease has been active often enables us to gauge its severity (e.g., if a patient reports several months of therapy and examination shows only mild inflammation with few inflammatory sequelae, we consider this mild disease), and this in turn affects our approach to therapy.
- Gauging likelihood of recurrence. Knowing whether a disease has recurred once is somewhat of an indicator of whether it will recur again, and we incorporate this observation into our discussions with patients.
PAST OCULAR HISTORY
Acknowledging that a list of potentially clinically relevant aspects of the past ocular history would be endless, we find that patients with uveitis will often have a history of one of a few diagnoses or interventions that inform the evaluation and management of their disease.
Diagnostically Informative Findings in the Past Ocular History
History of Cataracts at a Young Age
Cataract in young patients is often due to chronic uveitis. This seems elementary, but we are routinely astonished to see patients under 40 years of age diagnosed with cataract—and even taken in for cataract surgery—before they are noted to have chronic uveitis. A history of cataract in a young patient with uveitis suggests that the patient’s inflammation was present long enough to cause the cataract.
History of a Retinal Tear or Vitreous Hemorrhage
Patients with chronic uveitis often develop retinal tears or vitreous hemorrhage, presumably due to changes in the vitreous in the setting of inflammation, with subsequent traction at the vitreous base. The development of the tear or hemorrhage is often the event that brings a patient with chronic smoldering uveitis to ophthalmologic attention, although not uncommonly the uveitis is not diagnosed until after the posterior segment disease has been treated, and confusion sometimes results regarding whether the treatment caused the uveitis (which is quite unlikely) or the uveitis caused the tear (which is typical).
History of Eye Trauma or Surgery
The most obvious risk here is endophthalmitis if the surgery was performed fairly recently. Beyond this, an underlying predisposition to ocular inflammation may become manifest when a patient undergoes eye surgery. Both scleritis and uveitis can be “provoked” by this sort of intervention. The postoperative inflammation very often is initially presumed infectious, and the question of a possible infection may persist for quite a while before the immune-mediated nature of the disease becomes apparent. For this reason, ocular inflammation in the postoperative setting represents among the most challenging scenarios for the uveitis practitioner. At the very least, the management of ocular inflammation following an intraocular surgery should take place under the abiding suspicion that the condition may in fact be immune mediated and not infectious. (Such immune-mediated postsurgical reactions should be worked up like any other uveitis.) It should also be noted that when treating a patient with bilateral uveitis at any time after intraocular surgery, the practitioner is compelled to state whether this presentation may represent sympathetic uveitis.
History of Pseudophakia
Intraocular lenses (IOLs) are occasionally detrimental to patients with uveitis, and one is wise to be suspicious of the IOL as a potentially aggravating factor in a pseudophakic patient with uveitis.
Therapeutically Informative Findings in the Past Ocular History
History of Glaucoma
Patients with a history of glaucoma are particularly likely to develop corticosteroid-induced intraocular pressure elevation and often require immunomodulatory therapy for this reason.
History of Scleral Buckle Surgery
These patients may have had extensive manipulation of their conjunctiva, and this makes it difficult to inject corticosteroids in the subtenon or subconjunctival space. Indeed, any surgery involving extensive conjunctiva incision (strabismus procedures, open globe repairs, etc.) will create this problem. Transseptal/orbital floor injections may be more appropriate in this setting (see Chapter 20 on procedures).
MEDICAL HISTORY AND MEDICATIONS
A prior history or ongoing treatment of any of several systemic diseases affects our approach to the patient with uveitis, either because the systemic condition (or rarely its treatment) is a potential underlying cause or because it impacts our choice of pharmacotherapy.
Medical History Findings that Suggest a Uveitis Etiology
A number of systemic diseases and a few therapies are likely suspects of underlying causes for ocular inflammation. We observe that such entities can be grouped into five broad categories, an awareness of which helps us to organize our thoughts while undertaking the medical evaluation. Table 3.2 lists systemic diseases that are associated with ocular inflammation.
Table 3.2 Systemic disorders with ocular manifestations
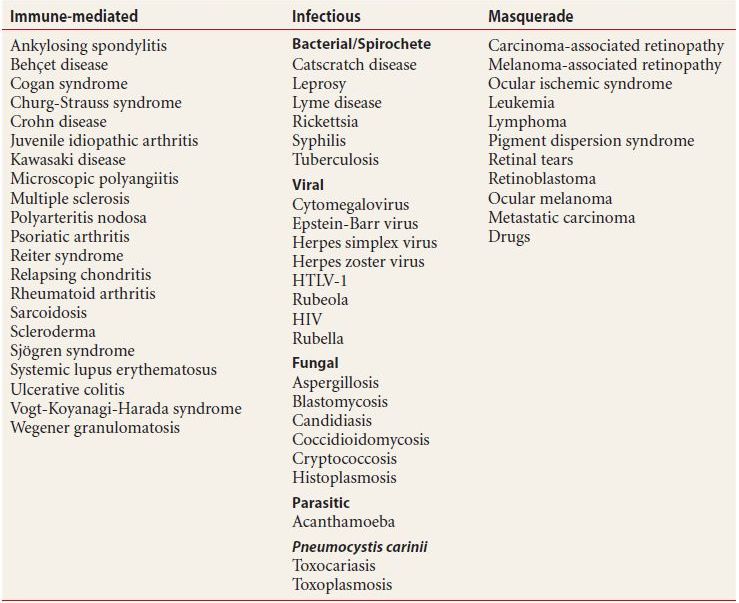
HIV, human immunodeficiency virus; HTLV-1, human T-lymphotropic virus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


