Medical and Corneal Disorders Relevant to Refractive Surgery
CHAPTER CONTENTS
Disorders of Other Ocular Structures
As we evaluate a patient for possible surgical vision correction, we must consider a variety of conditions, both systemic and ocular, that may affect surgical risk or outcome. A comprehensive systemic and ocular history is crucial for identifying the aspects of these conditions that determine the risks for intraoperative and postoperative complications of refractive surgical procedures. In this chapter, we discuss various systemic and ocular disorders as they pertain to refractive surgery, both preoperatively and postoperatively
MEDICAL DISORDERS
Vascular Disease
The presence of systemic vascular disease should be ascertained during the preoperative evaluation to determine the level of risk associated with refractive surgery. We discuss hypertension and diabetes mellitus, the most common vascular diseases. Other vascular conditions must be considered on an individual basis, with special attention to potential intraoperative and postoperative complications.
HYPERTENSION Hypertension in refractive candidates is usually mild, well controlled, and rarely associated with significant ocular disease.
Preoperative Considerations
- retinal findings (warrant further evaluation, consideration, and possibly postponement of refractive surgery)
- focal or generalized constriction of retinal arterioles
- arteriovenous (AV) crossing changes
- cotton-wool spots
- flame-shaped hemorrhages
- macular star of hard exudates (HEs)
- arteriolar tortuosity
- intraretinal edema
- preretinal hemorrhage (Fig. 3-1)
Surgical Considerations
- relative contraindications
- absolute contraindications
- sedative cross-reaction with systemic hypertensive medications
- malignant systemic hypertension
- sedative cross-reaction with systemic hypertensive medications

Figure 3-1 Hypertensive preretinal hemorrhage.
DIABETES MELLITUS Patients with diabetes may be good candidates for refractive procedures if the diabetes is well controlled and the patient’s ocular health is good.
Preoperative Considerations
- systemic history
- history of blood glucose levels and documented control
- positive family history of diabetes mellitus
- presence or history of gestational diabetes
- history of ocular diabetic findings
- presence of polydipsia, polyphagia, and polyuria
- general health status
- history of blood glucose levels and documented control
- refractive shifts and stability considerations
- recent unexplained hyperopic or myopic shift
- refractive instability
- recent unexplained hyperopic or myopic shift
- retinal signs of diabetic retinopathy
- retinal neovascularization
- vitreous hemorrhages
- fibrovascular membranes
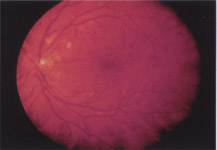
- microaneurysms (Fig. 3-2)
- retinal hemorrhage (dot blot/hemorrhages)
- hard exudate
- cotton-wool spots
- venous beading (VB)
- patient education about the progression of diabetes and its possible effect on ocular health and visual function
- retinal neovascularization
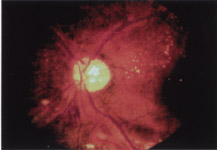
Figure 3–2 Diabetic retinopathy (microaneurysm).
Surgical Considerations
- absolute contraindications
- proliferative diabetic retinopathy (because of the intrinsic risk of retinal disease and loss of visual function with or without refractive surgery)
- relative contraindications
Postoperative Considerations
- slower wound healing (because of lower rates of corneal re-epithelialization)
- refractive shifts (require strict blood glucose control and postponement of enhancement procedures until the refractive shifts are stabilized)
- reduced rate of tear secretion and increased risk of dry eye and related symptoms (may require lubricant therapy)
Autoimmune or Collagen Vascular Diseases
This group includes a wide spectrum of diseases with most refractive patients exhibiting minimal signs or symptoms. Preoperative evaluation of the severity of the autoimmune disease as well as the number of medications required is important.
Preoperative Considerations
- decreased tear production because of lymphocytic infiltration and destruction of the lacrimal glands (most collagen diseases)
Surgical Considerations
- absolute contraindications (because of abnormal collagen cross-linking and abnormal and often unpredictable healing processes)
- scleroderma
- Marfan’s syndrome
- osteogenesis imperfecta
- Ehlers-Danlos syndrome
- documented history of keloid formation [only for procedures like radial keratotomy (RK) and photorefractive keratectomy (PRK), in which there is a prolonged healing process, to prevent permanent haze formation]
- scleroderma
- moderate relative contraindications (approach with extreme caution and only after complete patient education about the potential risks of surgery and the long-term visual outcome)
- rheumatoid arthritis
- systemic lupus erythematosus (SLE)
- Wegner’s granulomatosis
- polyarteritis nodosa
- relapsing polychondritis
- rheumatoid arthritis
- low relative contraindications (recommend surgery only after complete patient education about possible effects on the healing process and the long-term visual outcome)
- multiple sclerosis (warrants discussion on long-term prognosis for visual function)
- conditions that cause iridocyclitis, including ankylosing spondylitis, Reiter’s syndrome, and Crohn’s or ulcerative colitis (control the condition or wait for latency prior to surgical intervention)
- multiple sclerosis (warrants discussion on long-term prognosis for visual function)
Postoperative Considerations
- increased risk for poor or abnormal healing processes of the ocular surface
Infectious Diseases
Infectious diseases should be treated or stable prior to proceeding with an elective refractive procedure.
HUMAN IMMUNODEFICIENCY VIRUS AND AQUIRED IMMUNODEFICIENCY SYNDROME Many human immunodeficiency virus (HIV)-positive patients are quite healthy and have normal ocular status so they may still be good candidates for refractive surgery.
Preoperative Considerations
- a positive history of HIV or AIDS (does not preclude refractive surgery)
- a thorough history and comprehensive ocular examination to rule out retinopathy
- any sign of acute retinal necrosis, cytomegalovirus (CMV) retinitis, or other HIV retinopathy (warrants discussion about disease progression and effects on vision [Fig. 3–3])
Surgical Considerations
- need for universal precautions (the Centers for Disease Control provides guidelines) (although no documented cases of transmission of HIV from the tear film or through airborne vaporized particles from laser ablation)
Postoperative Considerations
- need for prophylaxis against postoperative bacterial or herpetic viral infection [fluoroquinolone, as well as trifluridine (Viroptic, Allergan, Irvine CA)], depending on the patient’s immune status.
HERPES SIMPLEX Herpetic keratitis often recurs, and residual corneal scarring affects visual performance so careful evaluation and education of these patients are essential.
Preoperative Considerations
- a complete ocular examination and history regarding previous ocular infection
- patient education about proper postoperative hygiene (to reduce risk of ocular contamination and infection for patients with a positive systemic history)
Surgical Considerations
- active ocular and periocular involvement (an absolute contraindication [Fig. 3–4])
- previous ocular or periocular infection (a relative contraindication )
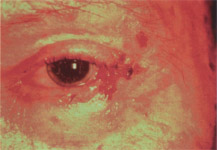
Figure 3-4 Periocular herpes simplex infection.
HERPES ZOSTER AND VARICELLA ZOSTER
Herpes zoster and varicella zoster recur less often but may be confused with herpes simplex infections so precautions are still required.
Preoperative Considerations
- see Herpes Simplex
Surgical Considerations
- latent systemic zoster infection (a relative contraindication ; advisable to delay surgical correction until the systemic disease is controlled)
- possible initiation of prophylactic systemic antiviral therapy 1 week before surgical intervention
- need for universal precautions to prevent contamination (although no documented cases of transmission of virus during laser ablation)
- increased risk for reactivation and transmission of the viral disease by incisional procedures
- possible initiation of prophylactic systemic antiviral therapy 1 week before surgical intervention
BACTERIAL INFECTIONS
Preoperative Considerations
Surgical Considerations
- possible postponement of elective surgical correction until signs of systemic disease abate and refractive stability and patient comfort return to normal
- high risk for sedative cross-reaction with systemic antibiotics
Postoperative Considerations
- systemic infection effects on refractive error
- rare medication effects on the refractive error (many medications may cause changes in accommodation)
- effect of sinusitis on patient comfort and tear film (decongestants often decrease normal tear production)
Endocrine and Metabolic Disorders
Few endocrine disorders have a dramatic effect on the eyes and refractive error. Abnormal thyroid function and the intricate hormonal changes associated with pregnancy and lactation are the most common endocrine conditions that may have a notable effect on refractive error and the postoperative healing process. These conditions are discussed in this section.
THYROID EYE DISEASE Patients with mild thyroid eye disease but without significant ocular complications may still be reasonable candidates for refractive surgery.
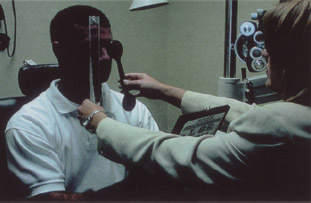
Figure 3-5 Prismatic correction for diplopia.
Preoperative Considerations
- signs or symptoms of thyroid eye disease (displayed by hyperthyroid, hypothyroid, or euthyroid patients)
- exophthalmos
- lid lag
- exposure keratitis
- diplopia
- exophthalmos
- binocular status (if binocular abnormalities are noted, educate the patient about possible progression and the potential need for prismatic correction to maintain single binocular vision)
- tear film status (increased likelihood of decreased aqueous secretion secondary to lymphocytic infiltration and destruction of the lacrimal gland)
Surgical Considerations
- refractive instability (an absolute contraindication)
Postoperative Considerations
- diplopia (may require prismatic correction after surgery to decrease or eliminate diplopia) (Fig. 3-5)
- tear film stability (may require topical lubricants and/or punctal plugs)
- dry eye (may require frequent lubrication to maintain comfort and visual function)
PREGNANCY AND LACTATION Patients’ refractive stability is often unpredictable during pregnancy and lactation.
Surgical Considerations
- temporary postponement of surgical correction (until after the pregnancy or, if the mother is breast feeding, until three months after weaning)
- potential systemic adverse effects of sedatives and topical prophylactic therapies on the fetus
Postoperative Considerations
- abnormal wound healing
- refractive instability
- tear films abnormality
CORNEAL DISORDERS
Epithelial Disorders
The surgeon and clinician should document various disorders of the corneal epithelium before undertaking surgical intervention. Epithelial basement membrane dystrophy (EBMD) or other epithelial defects may lead to poor or prolonged healing and increased risk for epithelial ingrowth or epithelial defects.

Figure 3-6 Poor epithelial adhesion.
These three processes may lead to patient discomfort during the early postoperative period and increase the risk that further surgery will be necessary. Some surgeons and patients may prefer refractive procedures such as PRK if epithelial disease is present, to prevent postoperative complications and, if possible, treat the ocular surface disease.
EPITHELIAL BASEMENT MEMBRANE DYSTROPHY EBMD is an abnormal maturation and production of epithelial basement membrane with associated abnormal epithelial adhesions.
Preoperative Considerations
- small, cystic, subepithelial, isolated or linear arrangement of subtle opacities (may be observed by focal illumination or high-lighted by retroillumination)
- negative staining patterns over abnormal basement membrane
Surgical Considerations
- laser in situ keratomileusis (LASIK)
- risk for epithelial ingrowth
- poor epithelial adhesions (Fig. 3-6)
- difficult flap replacement
- poor epithelial adhesions (Fig. 3-6)
- PRK
- irregular surface ablation
- incisional surgery
- epithelial ingrowth
Postoperative Considerations
- LASIK
- epithelial ingrowth formation
- development of stromal necrosis and flap melt (Fig. 3-7)
- recurrent erosion because of poor epithelial adhesions
- epithelial ingrowth formation
- PRK
- incisional surgery
- epithelial ingrowth formation
- slow or abnormal re-epithelialization rate
- epithelial ingrowth formation
- transient changes in vision quality secondary to recurrent epithelial erosions in advanced stages of disease (vision rarely affected in the mild stages of the disease)
- poor lubrication from irregular microvilli formation and subsequent poor glycocalyx formation
- patient discomfort as well as prolonged healing processes (because of the poor attachment of the epithelium small corneal erosions may develop).
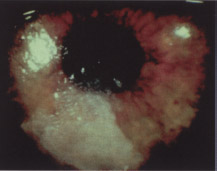
Figure 3-7 Stromal melt after LASIK.
RECURRENT CORNEAL EROSION Recurrent corneal erosions (RCEs) are most commonly caused by traumatic injury or other ocular surface disorders that affect the adhesive characteristics of epithelium and its basement membrane to Bowman’s membrane.
Preoperative Considerations
- positive history of an RCE (not a contraindication for refractive surgery)
- refractive range
- negative staining defects over recent erosions (Fig. 3-8)
- ocular history of pain upon waking that subsides with time
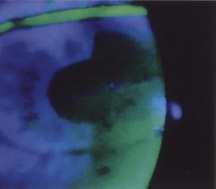
Figure 3-8 Negative staining defect over corneal erosion.
Surgical Considerations
- poor epithelial adherence in the area of the keratectomy edge or incision
- safety of refractive range (for removal of the area of damaged weak epithelium and basement membrane with PRK)
- preference for PRK or PTK (phototherapeutic keratectomy) over LASIK especially for low myopia with anterior basement membrane dystrophy (allows formation of new epithelial basement membrane and development of normal attachments to the underlying Bowman’s membrane or anterior stroma)
Postoperative Considerations
- epithelial ingrowth
- intermittent corneal defects
- poor tear film stability
- patient discomfort
PANNUS OR VASCULARIZATION Corneal hypoxia or inflammation often leads to corneal micropannus or vascularization anterior to the limbus. This vascularization is common in those who overwear their contact lenses or in the presence of other ocular surface diseases.
Preoperative Considerations
Surgical Considerations
- proximity to incision or keratectomy (Fig. 3–9) (may lead to intralamellar hemorrhage)
- intraoperative hemorrhage
- flap retraction along edge of pannus
Postoperative Considerations
- intralamellar hemorrhage
- inflammatory reaction (resulting in intralamellar keratitis)
- localized edema (resulting in decreased vision)
- inflammatory reaction (resulting in intralamellar keratitis)
- vascular advancement into the incisions
- hemosiderin deposition
- decreased vision from localized inflammatory process and edema
- intralamellar keratitis
- decreased vision from localized inflammatory process and edema
MEESMAN’S AND REIS BUCKLER CORNEAL DYSTROPHIES Meeseman’s or hereditary juvenile epithelial dystrophy is a bilateral and symmetric formation of epithelial cysts with thickened basement membrane that appear as early as the first few months of life. Reis Buckler disorder is a Bowman’s membrane disorder that also affects the central cornea. It is a bilateral and symmetric condition that usually results in central corneal opacities and a subsequent decrease in visual function by the first to second decades of life.

Figure 3-9 Pannus close to an RK incision.
Surgical Considerations
- need for a lamellar or full thickness corneal graft in advanced stages to decrease the fibrillar material that has replaced Bowman’s membrane (an absolute contraindication for lamellar refractive surgery)
Stromal Disorders
Most stromal disorders are relative contraindications for refractive surgery, though patients with some stromal dystrophies may benefit to some degree from lamellar surgery. A few stromal disorders, including ectatic disorders such as keratoconus are absolute contraindications for refractive surgery.
KERATOCONUS The etiology of keratoconus is unknown, but the progressive thinning of the central cornea associated with this disorder presents obvious challenges to successful refractive surgery.
Preoperative Considerations
- topography (for all refractive patients)
- pachymetry (for all patients in whom central corneal thinning is suspected)
- early-stage findings
- subtle, irregular astigmatism, usually bilateral but asymmetric [central corneal curvature readings of > 48 D (Fig. 3-10) and vertical asymmetry >5 D (Fig. 3-11)]
- progressive myopia (usually bilateral but asymmetric)
- moderate-stage findings
- progressive thinning of the central cornea (central corneal thickness significantly lower than peripheral corneal thickness, commonly < 500 (μm)
- Fleischer’s ring
- Vogt’s stria
- subtle, irregular astigmatism, usually bilateral but asymmetric [central corneal curvature readings of > 48 D (Fig. 3-10) and vertical asymmetry >5 D (Fig. 3-11)]
Surgical Considerations
- an absolute contraindication to all current types of refractive surgery because progressive corneal thinning increases the risk of corneal instability
Figure 3–10 Topography with corneal curvature greater than 48 D.
Figure 3–11 Topography with vertical meridian asymmetry greater than 5 D.
THIN CORNEAS Corneal thickness measurements are critically important for determining risk for both incisional and lamellar refractive surgery. The surgeon must both rule out preoperatively and prevent the development postoperatively of corneal ectasia.
Preoperative Considerations
- assessment of corneal thickness by pachymetry (average corneal thickness in normal myopic patients = 545−555 μm)
- minimization of postoperative risk for iatrogenic keratoconus (from lamellar surgery)
- minimization of postoperative risk for full-thickness perforations and endophthalmitis (from incisional surgery)
- minimization of postoperative risk for iatrogenic keratoconus (from lamellar surgery)
- estimated postoperative stromal bed thickness (for lamellar surgery)
- ideal = ≥ 300 μm
- borderline = 250 μm
- absolute minimum = 200 μm
- ideal = ≥ 300 μm
- variations in lamellar flap thickness (flat corneal curvature may result in an abnormally thin cap)
Surgical Considerations
- incisional surgery
- number of incisions (affected by corneal thickness)
- corneal thickness determines depth of incisions (perforations at any location during surgery suggest excessive incisional depth)
- number of incisions (affected by corneal thickness)
- lamellar surgery
- estimation of postoperative corneal thickne’ss (preoperative corneal thickness- thickness of stromal tissue ablated), which determines ablation profile and multizone vs. single zone considerations
- thin cap or a perforation in the corneal cap
- estimation of postoperative corneal thickne’ss (preoperative corneal thickness- thickness of stromal tissue ablated), which determines ablation profile and multizone vs. single zone considerations
Postoperative Considerations
- signs of corneal perforation after incisional surgery
- positive Seidel’s sign
- gaping incisions (Fig. 3-12)
- localized deep stromal inflammation and edema
- endophthalmitis
- positive Seidel’s sign
- lamellar surgery
- corneal ectasia from an abnormally thin cornea
- irregular astigmatism
- progressive myopia
- postoperative evaluation for iatrogenic keratoconus (thin corneas with refractive instability and steepening on topography, including pachymetry and topography)
- corneal ectasia from an abnormally thin cornea

Figure 3-12 Gaping RK incision.
STROMAL OPACIFICATION OR SCARS Stromal scars may be insignificant if completely off the visual axis or very significant if within the visual axis. Scars in the visual axis may cause a loss of BCVA and often lead to a suboptimal postoperative result.
Preoperative Considerations
- opacity (evaluated by slit lamp exam)
- depth
- location [effect on visual axis (Fig. 3-13)]
- density
- effect on refractive error assessment
- depth
Surgical Considerations
- selection of appropriate surgical procedure
- incisional surgery
- for opacities outside the visual axis (opacity will not affect postoperative healing of the incisions)
- irregular wound healing (effect of fibrosis on radial keratectomy blade incision)
- difficulty creating channel for insertion (effect of opacity or fibrosis on intracorneal ring insertion)
- for opacities outside the visual axis (opacity will not affect postoperative healing of the incisions)
- lamellar surgery
- LASIK indicated when the opacity is outside the visual axis (opacity will not affect postoperative healing of the flap)
- risk for irregular ablation (effect of the opacity or fibrosis on ablation profiles and homogeneity of ablation)
- LASIK indicated when the opacity is outside the visual axis (opacity will not affect postoperative healing of the flap)
- intraocular surgery (if the opacity is outside the visual axis)
- difficult visualization of anterior segment
Figure 3-13 Stromal scar near the visual axis.
Postoperative Considerations
- wound healing
- irregular healing and/or increased fibrosis (effect of opacity or fibrosis depth)
- irregular healing at fibrosis location (effect of opacity or fibrosis location)
- potential increase in fibrosis density if incision passes through fibrosis (effect of opacity or fibrosis density)
- irregular healing and/or increased fibrosis (effect of opacity or fibrosis depth)
- visual acuity (development of irregular astigmatism or surface changes)
- irregular healing with potential irregular astigmatism (effect of opacity or fibrosis depth)
- effect of opacity or fibrosis density (see above)
- irregular healing with potential irregular astigmatism (effect of opacity or fibrosis depth)
- partial-thickness lamellar graft (may eliminate the opacity and enhance unaided visual acuity)
STROMAL DYSTROPHIES The three primary stromal dystrophies (lattice, macular, granular) are not contraindications for refractive surgery but may pose difficulty in both presurgical evaluation and surgical performance.
Preoperative Considerations
- evaluation of cornea to identify stromal dystrophy
- effects of stromal dystrophy
- refractive error (more difficulty getting a refractive endpoint)
- visual acuity (BCVA may be reduced because of stromal opacities)
- potential for reduced preoperative BCVA
- visual acuity (BCVA may be reduced because of stromal opacities)
- patient education
- risks of surgery
- diagnosis of stromal dystrophy
- potential effect on visual acuity
- risk for disease progression and long-term visual acuity
- risks of surgery
Surgical Considerations
- ablation profile alterations (deeper ablation to remove opacities)
- intraoperative hydration levels (different hydration pattern of stroma because of different components)
- incisional difficulty (because of difficult visualization and different consistency of stroma)
Postoperative Considerations
- delay in healing response
- initial reduction in visual acuity because of poor healing response
- ocular surface abnormalities
Endothelial Disorders
Although less common, endothelial corneal dystrophies comprise a complex group of conditions that may significantly impact the results of refractive surgery. Patients should be carefully screened for these conditions before undergoing any refractive discussion.
ENDOTHELIAL GUTTATA OR FUCHS’ DYSTROPHY A few endothelial guttata are commonly found in patients older than 60 years of age and represent a premature aging process involving the corneal endothelium. Fuchs’ dystrophy is the association of guttata with frank corneal edema indicating endothelial decompensation (an absolute contraindication to refractive surgery).
Preoperative Considerations
- dewdrop or wartlike endothelium excrescences in the central cornea
- indicates an overall weakness of the corneal endothelium
- must be differentiated from endothelial pigment that is often deposited in the same location
- endothelial cell counts should be considered prior to any refractive procedure [if >10 guttata or if an intraocular procedure, such as phakic intraocular lens (IOL) insertion or clear lens extraction, is being considered]
- indicates an overall weakness of the corneal endothelium
- presence and status of corneal edema
Surgical Considerations
- good visual acuity and good prognosis for corneal integrity (then not a contraindication for refractive surgery)
- presence or severity of guttata
Postoperative Considerations
- visual acuity (edema and excessive corneal hydration may produce a myopic shift)
- corneal edema (minimize with hypertonics)
- damage to ocular surface integrity
- artificial tears or lubricating ointment
- bandage hydrogel lens (if necessary)
- artificial tears or lubricating ointment
Other Corneal Disorders
Preoperative identification of other rare corneal dystrophies is important because they may impact surgical planning and results of refractive procedures.
Preoperative Considerations
- examination to exclude posterior polymorphous dystrophy and iridocorneal endothelial dystrophies
Surgical Considerations
- absolute contraindications
- posterior polymorphous dystrophy
- iridocorneal endothelial dystrophies
- infectious keratitis with active herpetic infection or active fungal infection
- posterior polymorphous dystrophy
- relative contraindications
- active bacterial infection (postpone surgery until the ocular surface is clear)
- past history of herpetic infection (surgery carries a risk of reactivation; provide prophylactic treatment)
- active bacterial infection (postpone surgery until the ocular surface is clear)
Postoperative Considerations
- continuation of antiviral therapy if past herpetic infection is suspected
- monitoring of intraocular pressure (IOP) every 6 months if iridocorneal dystrophies suspected
DISORDERS OF OTHER OCULAR STRUCTURES
Eyelids
Eyelid abnormalities must be evaluated, documented, and managed properly to ensure the best possible surgical outcome. Ptosis, blepharitis, and appositional or meibomian gland disorders may affect patients’ intra- and postoperative status and are discussed in the following sections.
PTOSIS Mild ptosis (eyelid droop < 1 mm should be documented whenever noted preoperatively.
Preoperative Considerations
- proper assessment and documentation of preexisting ptosis (useful as a reference if its preexisting status is questioned after surgery)
- history of lid surgery or trauma (may indicate reason for ptosis and document that refractive procedure did not cause it)
- decreased levator function (may be associated with poor lid closure and exposure after refractive procedures)
- narrowing of the palpebral fissure (more difficult access to the eye for procedures)
Surgical Considerations
- proper and careful speculum placement (may cause further damage to the lid muscles, particularly if there was recent lid surgery)
Postoperative Considerations
- temporary ptosis (levator function usually returns within a few days but necessitates education of patient about cause and duration)
- permanent but rare ptosis (may warrant surgical repair for the following reasons)
- cosmetically unacceptable
- incomplete lid closure causing exposure keratitis
- reduction of visual field or blocking of visual access by lid
- cosmetically unacceptable
BLEPHARITIS Blepharitis is a very common eyelid condition often associated with dry eyes and meibomian gland dysfunction.
Preoperative Considerations
- proper diagnosis of and differentiation between staphylococcal and seborrheic blepharitis
- evaluation of dry eyes
- evaluation of any keratitis secondary to the blepharitis or dry eyes
- bulbar conjunctival edema
- anterior blepharitis
- Staphylococcus sp. flakes on the base of the eyelashes (collarettes), eyelid ulceration, associated marginal keratitis (preoperative treatment reduces risk of infection)
- posterior blepharitis
- chalazion (infection of meibomian gland; use lid scrubs and ocular lubrication generously for several weeks to eliminate prior to refractive surgery)
- seborrheic secretions on eyelashes (sleeves) associated with scalp dandruff (Fig. 3-14)
- chalazion (infection of meibomian gland; use lid scrubs and ocular lubrication generously for several weeks to eliminate prior to refractive surgery)
Surgical Considerations
- reduction or elimination of risk for postoperative infectious keratitis by postponing any procedure until blepharitis is controlled
- bulbar conjunctival edema and difficult keratome placement
- proper irrigation of the surgical field with topical antibiotics to prevent infection
- minimal contact with affected lids (if possible)
- bulbar conjunctival edema and difficult keratome placement
Figure 3-14 Seborrheic blepharitis.
Postoperative Considerations
- incisional surgery
- endopthalmitis induced by corneal perforation (treat aggressively)
- corneal ulceration (treat aggressively with fluoroquinolones and monitor daily)
- endopthalmitis induced by corneal perforation (treat aggressively)
- lamellar surgery
- intrastromal keratitis caused by bacterial endotoxin (treat with topical antibiotics, steroids, or both; usually clears within a few weeks, even if left untreated)
- corneal ulceration (treat aggressively with fluoroquinolones)
- intrastromal keratitis caused by bacterial endotoxin (treat with topical antibiotics, steroids, or both; usually clears within a few weeks, even if left untreated)
MEIBOMIAN GLAND DYSFUNCTION Abnormal production, constitution, or secretion of lipid from the meibomian glands characterizes meibomian gland dysfunction (MGD).
Preoperative Considerations
- indentification of chalazion
Surgical Considerations
- presence of chalazion (an absolute contraindication)
- may alter corneal structure and refractive status
- may affect patient comfort during and after surgery
- treat appropriately before surgical intervention
- may alter corneal structure and refractive status
- careful speculum placement to avoid excess lipid excretion or patient discomfort
- proper irrigation to eliminate lipid deposits in the lamellar interface in LASIK and PRK
Postoperative Considerations
- ocular surface inflammation
- mild intrastromal keratitis
- patient discomfort
Conjunctival Abnormalities
Preoperative Considerations
- conjunctival chemosis (Fig. 3-15)
- conjunctival redundancy
- conjunctival inflammation
Surgical Considerations
- absolute contraindication
- infectious conjunctivitis
- relative contraindications
- conjunctival redundancy or chemosis (proper vacuum for the keratectomy is often difficult in lamellar surgery)
- generalized conjunctival inflammation (may lead to poor healing response in intraocular surgery)
- conjunctival redundancy or chemosis (proper vacuum for the keratectomy is often difficult in lamellar surgery)
Postoperative Considerations
- wound healing complications (swollen inflamed conjunctiva may lead to an uneven ocular surface that prevents the smooth flow of tears and medications)
- infectious conjunctivitis (treat aggressively)
- ocular discomfort
- resolves in 24 to 48 hours
- often responds to postoperative steroid drops
- ocular discomfort

Figure 3-15 Conjunctival chemosis.
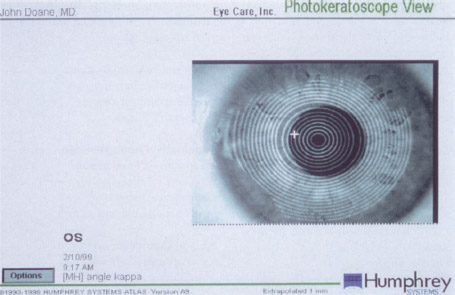
Figure 3-16 Angle kappa as seen on topography (photokeratoscopic view).
Extraocular Muscles
Phorias and tropias present an interesting challenge to the refractive surgeon because they are often corrected with a prism in the patient’s glasses. Patients often assume that the refractive procedure can also eliminate this prism, which is not possible. Preoperative counseling and potential treatment of the phoria or tropia is required.
Preoperative Considerations
- identification of motility or binocular status abnormalities for proper alignment of the visual system and successful surgical and visual outcome
- patient education about the risk for postoperative diplopia and the potential need for postoperative prismatic correction
- phorias (rarely affect intraoperative or postoperative outcomes of refractive procedures)
- tropias
- may affect visual outcome and overall subjective success of the surgery
- significant surgical correction before the refractive procedure may be indicated
- may affect visual outcome and overall subjective success of the surgery
- angle kappa (Fig. 3-16) (usually identified in hyperopic patients via photokeratoscopy and topography [photokeratoscopic view])
Surgical Considerations
- possible poor intraoperative fixation resulting from tropias
- alignment of visual axis (crucial for proper centration and central optical zone determination in incisional surgery)
- lamellar surgery
- alignment of visual axis
- patient fixation
- ablation centration (Fig. 3-17)
- alignment of visual axis
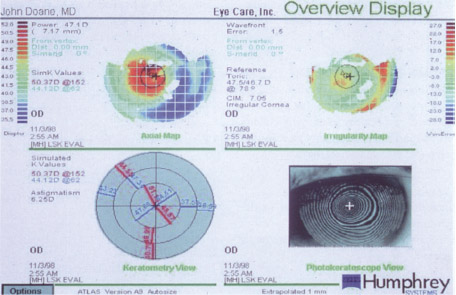
Figure 3–17 Ablation centration in the presence of angle kappa.
Postoperative Considerations
- aggravation of the binocular status of some patients can result in subjective or objective diplopia
- reduction or elimination of certain binocular problems by elimination of the refractive error for some patients
- postoperative diplopia secondary to removal of prismatic or accommodative effect of the spectacle lens with tropia
- visual therapy (if indicated)
- prismatic spectacle correction
- surgical correction of the tropia (misalignment) in rare cases
- visual therapy (if indicated)
Large Pupils
Preoperative Considerations
- evaluation of pupil size (using scotopic and photopic illumination, to avoid postoperative complaints about glare)
- choice of ablation zone of the laser (should be at least as big as the scoptic pupil size)
- preoperative perception of glare (thorough history with and without correction)
- patient counseling about the risk of postoperative glare
Surgical Considerations
- proper alignment of the visual axis and the pupil (essential to successful surgical and visual outcome)
- choice of the biggest zone possible
Postoperative Considerations
- “off-axis” treatment of persistent complaints of diplopia or scotopic glare
- spectacle tint or specialized contact lens to decrease glare
Orbital Configuration and Palpebral Opening
In lamellar surgery, small or deep-set eyes may make it difficult for the surgeon to set the microkeratome ring in the proper position. Narrow fissures also may make it difficult to place the ring, or may interfere with microkeratome movement. Unusual orbital configuration/palpebral openings also may increase postoperative patient discomfort because of lid trauma during surgery.
INCOMPLETE EYELID CLOSURE Patients may have nocturnal lagophthalmos and are often unaware that they have the condition. A careful preoperative examination allows anticipation and postoperative treatment of exposure problems if necessary.
Preoperative Considerations
- inferior band staining greater in the morning
- visible scleral show when eyelids are gently closed
Surgical Considerations
- proper speculum selection (allows for proper positioning with minimal patient discomfort)
- minimal anesthesia
- copious lubrication
Postoperative Considerations
- exposure keratitis (occurs often but is treatable with lubricants)
- use of ocular lubricants
- punctal plugs
- taping of eyelid at night for first week after procedure
SMALL FISSURE SIZE Hyperopic eyes in particular are associated with small fissures. The smaller opening makes any surgical procedure more difficult because visualization is more difficult and the equipment is a standard size.
Preoperative Considerations
- appropriate measurement of fissures to assess preoperative interpalpebral opening size (for LASIK, test the fit of the suction ring in the eye)
- patient education about difficulty of surgery on eyes with small fissures
Surgical Considerations
- proper speculum selection to increase patient comfort
- keratome selection for ease of passage
Postoperative Considerations
- usually minimal postoperative visual effects
Retinal Disorders
Retinal disorders should be evaluated and treated so that they are completely stable for any elective refractive procedure.
Preoperative Considerations
- identification of retinal tears, holes, detachment, or retinal scars
- history of retinal detachment
- history of previous retinal surgery
Surgical Considerations
- absolute contraindication
- visually threatening retinopathy
- relative contraindications (preoperative repair indicated)
- untreated retinal breaks
- retinal holes
- retinal tears
- untreated retinal breaks
- careful placement of suction ring detachment to ensure adequate suction (if previous scleral buckle for retinal detachment)
Postoperative Considerations
Suggested Readings
Doane JF, Slade SG. ALK, LASIK, and hyperopic LASIK. In: Wu H, Steiner R, Slade S, Thompson V, ed. Refractive Surgery. New York: Thieme; 1999:393-406.
Machat JJ. Preoperative myopic and hyperopic LASIK evaluation. In: Machat JJ, Slade SD, Probst LE, ed. The Art of LASIK. Thorofare, NJ: Slack Inc.; 2000:127-138.
Slade SG, Doane JF, Ruiz LA. Laser myopic keratomileusis. In: Elander R, Rich LF, Robin JB, ed. Principles and Practice of Refractive Surgery. Philadelphia: W.B. Saunders; 1997: 357-366.
Thompson VM, Wallin D. Patient selection and preoperative considerations. In: Wu H, Steiner R, Slade S, Thompson V. Refractive Surgery. New York: Thieme; 1999:41-52.
< div class='tao-gold-member'>



