Intacs Corneal Ring Segments
CHAPTER CONTENTS
Myopia, or nearsightedness, is the most common refractive problem in the United States; more than one fourth of the population (∼ 70 million people) use corrective eyewear for myopia. With recent technological advances, consumers have increased interest in, as well as heightened expectations for, refractive surgery as a reasonable and viable alternative to eyeglasses and contact lenses. INTACS (KeraVision, Inc., Fremont, CA) is the third generation of the original 360-degree intrastromal corneal ring (ICR) (KeraVision, Inc.) that comprised two 150-degree arcs (Fig. 18-1).]
HISTORY
A. E. Reynolds conceived of the ring (based on expansion and contraction) in 1978; Kera Associates was formed in 1980 to develop the ring and other concepts. In 1985, the first preclinical studies of Reynolds’s concept led to development of lens thickness as the means of achieving correction (as opposed to the expansion/ contraction model), and in 1986, Kera-Vision, Inc., was founded to focus solely on development of its ICR technology.
Researchers first placed the ring in animal eyes in 1985 and subsequently conducted extensive feasibility studies on various animals, including rabbits, cats, and three primate species. The rabbit became the safety model because rabbits’ eyes had been used historically for ophthalmic research and safety testing (its response to a foreign body approximates that of the human eye). However, no animal model had a cornea with the same thickness and morphological characteristics as the human cornea. Despite the thinness of rabbit cornea and the absence of a Bowman’s membrane, researchers did not identify a more representative animal model. To refine the procedure for evaluating the ICR in live eyes, researchers inserted ICRs into the eyes of approximately 200 rabbits.
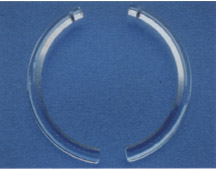
Figure 18-1 Appearance of Intacs segment before implantation.
In 1991, to demonstrate the safety of the ICR in humans, researchers conducted a blind-eye trial in Brazil and a similar one in the United States shortly thereafter. Both studies demonstrated that the ICR could be safely inserted into the peripheral corneal stroma in humans, thereby flattening the central cornea; five-year follow-up demonstrated that the eye tolerated the ring well, even years after insertion. The first procedures on sighted human eyes were performed in Brazil in 1991 and in the United States in 1993 as part of a phase II study regulated by the U.S. Food and Drug Administration (FDA).
In 1995, KeraVision created intrastromal corneal ring segments (ICRS), an alternative design, and introduced them into clinical trials in the United States. A U.S. phase II study and a two-site European study were initiated in 1995. U.S. phase III (10 reporting sites) research was initiated in 1996. In April 1999, the FDA approved three sizes (0.25, 0.30, and 0.35 mm) of Intacs, the commercial name for ICRS. Intacs completely replaced the 360-degree ICR. Use of Intacs has eliminated incision-related healing complications that were noted with the 360-degree ICR. Surgeons have performed approximately 1,800 Intacs procedures clinically worldwide to date. As a nonlaser alternative that does not remove tissue from the central optical zone (OZ) and is both removable and replaceable, Intacs represent a new direction for refractive surgery.
Specifications
- two half-rings placed through a single, peripheral incision
- made of polymethylmethacrylate
- varying the thickness of Intacs changes corneal curvature and dioptric correction (a nearly linear relationship between the degree of flattening achieved and the device thickness)
Advantages
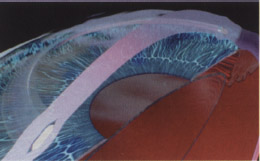
- reshaping of the cornea’s anterior curvature without invading the patient’s central visual axis (Fig. 18-2)
- maintenance-free correction
- rapid, predictable, and stable results
- minimal risk of loss of best corrected visual acuity (BCVA) (in FDA clinical trials that did not allow secondary interventions, 90% of patients with one implanted eye were very satisfied with their surgical outcome, and 95% of patients with bilateral surgery were satisfied)
- approximately 20% of patients with BCVA of 20/16 or better after primary procedures involving Intacs without enhancements (data from an FDA study)
- simple outpatient procedure performed under topical anesthesia, with little risk of incision-related complications
- preservation of tissue in central OZ
- maintenance of prolate corneal asphericity
- simple removability or replaceability (unique to Intacs and especially appealing to conservative or cautious patients)
- following removal, return of refraction to preoperative level, in most cases (according to recent data)
- excellent safety results (1.1% incidence of complications in U.S. trials)
- approximately 20% of patients with BCVA of 20/16 or better after primary procedures involving Intacs without enhancements (data from an FDA study)
PREOPERATIVE CONSIDERATIONS
Indications and Inclusion Criteria
- reduction or elimination of mild myopia (–1.00 to –3.00 D spherical equivalent at the spectacle plane)
- age of 21 years or older
- documented stability of refraction, as demonstrated by less than 0.50 D of change for at least 12 months prior to the preoperative examination
- +1.00 D or less of astigmatism
Patient Education
- Assist the patient in choosing the best procedure for his or her refractive error.
- Advise patient of realistic visual expectations and potential postoperative visual problems, including the fact that the patient may not be totally independent of spectacle lenses, as a result of this or any other refractive procedure.
- Discuss the specific advantages, limitations, and potential complications of the selected refractive procedure at an early consultation (this can save time in the long run).
- Address patient’s concerns about permanently altering the eyes and the availability of options in the event that the patient is dissatisfied with the outcome.
- Discuss all known general surgical risks with patient.
Patient Preparation
- As with any surgical procedure, take precautions to minimize the risk of infection.
- Instruct the patient to discontinue application of eye makeup for 2 to 3 days before the procedure.
- Advise the patient to instill one drop of trimethoprim (Polytrim; Allergan, Inc., Irvine, CA) in the operative eye at bedtime on the night prior to the procedure.
- Instruct the patient to instill one drop of Polytrim every hour (a total of three applications) beginning 3 hr before the procedure.
- Ensure that the patient completes all administrative forms, including the patient consent form.
Preoperative Medications
- Valium (5-10 mg, 20-30 min before procedure)
- diclofenac sodium (Voltaren Ophthalmic; CIBA Vision, Atlanta, GA) drops (20-30 min prior to procedure)
- tetracaine (Cetacaine or Pontocain; apply drops upon entering operative suite)
SURGICAL CONSIDERATIONS
Absolute Contraindications
- collagen vascular, autoimmune, or immunodeficiency disease
- ocular conditions that may predispose the patient to future complications (e.g., keratoconus, recurrent corneal erosion syndrome, or corneal dystrophy)
Relative Contraindications
- pregnancy or nursing
- use of isotretinoin (Accutane; Roche Pharmaceuticals, Nutley, NJ), amiodarone (Cordarone, Wyeth-Ayerst Laboratories, Madison, NJ), and/or sumatriptan (Imitrex; Glaxo Wellcome, Inc., Research Triangle Park, NC)
Methods
- Administer topical anesthesia alone, topical anesthesia with mild short-acting sedation, or topical anesthesia with intravenous conscious sedation and local anesthesia.
- Prepare and drape the patient in the usual fashion for anterior segment surgery.
- Use tetracaine drops as required.
- Use “verbal” anesthesia (constant reassurance to the patient throughout the procedure).
- Use an 11-mm OZ marker to mark the geometric center to the cornea to ensure accurate placement of the incision.
- Soak a Chayet sponge with tetracaine before making the incision or just prior to placement of the vacuum centering guide (VCG).
- With a previously inked incision marker, delineate the position of the radial incision, which should be no more than 1.8 mm long.
- Measure the peripheral corneal thickness at the center of the radial incision mark by ultrasound pachymetry, and set a diamond knife to 68% of this reading.
- Make a radial incision with the diamond knife at two-thirds of the corneal depth in the peripheral stroma.
- Using a modified Suarez spreader, laterally separate the corneal tissue at the base of the incision to prepare a corneal pocket near each side of the incision.
- Place a VCG over the center mark.
- Insert a dissector into the incision.
- Perform dissection of the cornea at two-thirds depth, clockwise and counterclockwise.
- Release the VCG.
- Use forceps to place the segments through the stromal channels.
- Position the segments temporally with a Sinskey (Duckworth’s Kent, St. Louis, MO) hook so that the superior ends are approximately 3 mm apart and symmetrically positioned around the incisions.
- Appose the radial incision edges as indicated in Figure 18-3.
- Place sutures.
- To close the incision, use one or two 11-0 nylon interrupted sutures (ensures good wound apposition through postoperative day 7).
- Shorter incisions (<1.8 mm) may require placement of only one suture.
- Remove sutures at postoperative day 7.
- If you observe loose sutures or at least 1.0 D of suture-induced manifest refraction cylinder (“with the rule” astigmatism), remove sutures earlier.
- To close the incision, use one or two 11-0 nylon interrupted sutures (ensures good wound apposition through postoperative day 7).
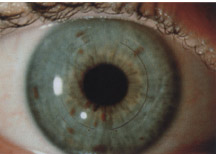
Figure 18-3 Appearance of Intacs after placement.
Intraoperative Complications
- allergic reactions, the remote chance of damage to the eye, medical complications, or death from anesthesia
- see Table 18-1
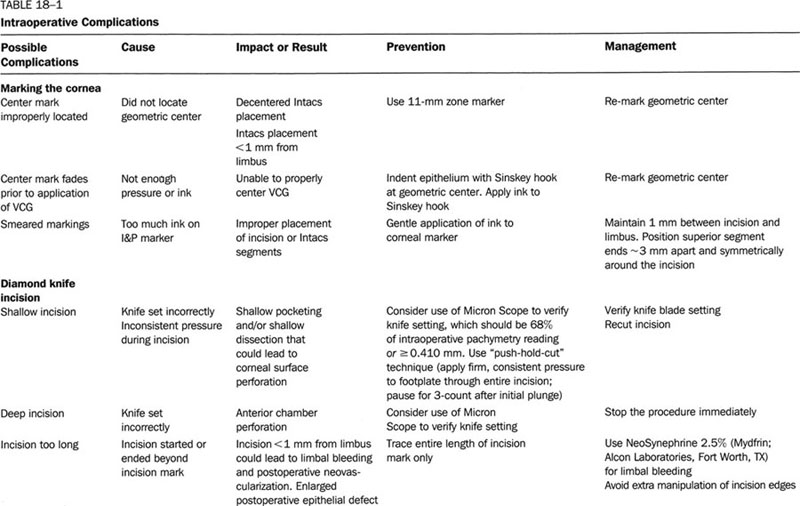
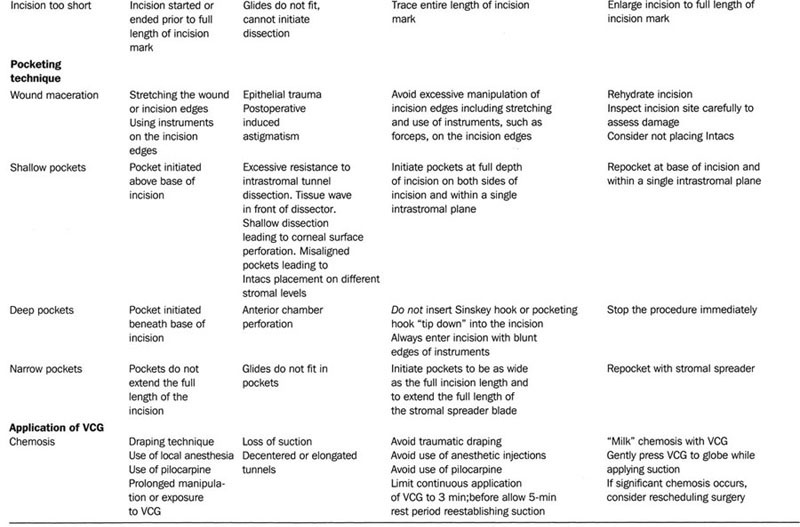
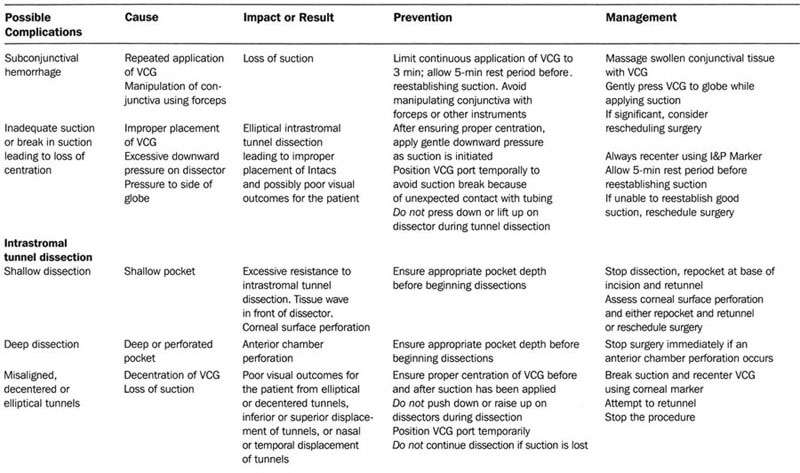
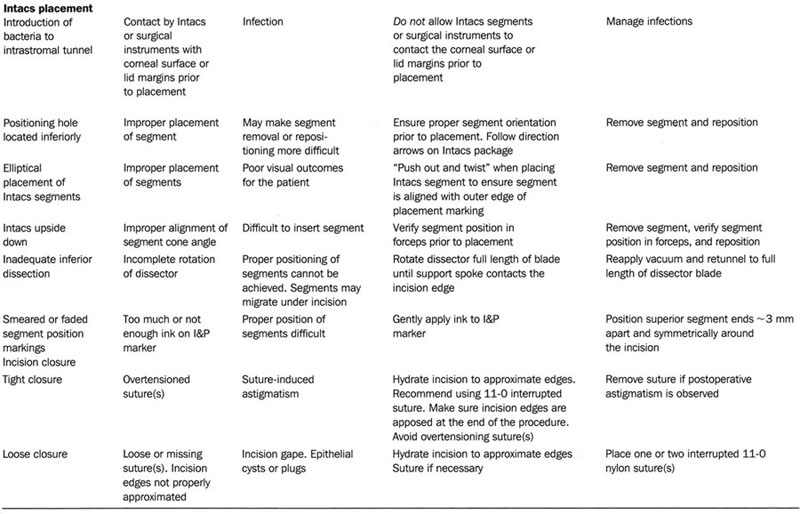
Intraoperative Complications
POSTOPERATIVE CONSIDERATIONS
Postoperative visits are usually scheduled for 1 day, 1 week, 1 month, 3 months, and 6 months after surgery.
Day of Surgery
- expected symptoms
- mild to moderate discomfort/pain for a few hours after surgery (if pain is more severe, contact the surgeon)
- foreign body sensation or “scratchiness” (common during the immediate postoperative period)
- fluctuating vision during the first month
- dry eyes for the first 2 to 3 months
- mild to moderate discomfort/pain for a few hours after surgery (if pain is more severe, contact the surgeon)
- management
- Apply an antibiotic-steroid combination ointment or solution (0.1% dexamethasone and 0.3% tobramycin or equivalent) to the operative eye at the end of the procedure.
- Perform a slit-lamp examination (to observe the segment placement and incision closure and to verify tunnel depth).
- Cover the operative eye with a clear shield (the patient should wear a shield at night for 1 week).
- Provide the patient with postoperative instructions.
- Prescribe analgesic medication (acetaminophen, paracetamol, or equivalent) for postoperative discomfort (prescribe other pain medication at your discretion).
- Provide artificial tears as needed.
- Recommend that the patient take a nap (patients will be photophobic and they should rest their eyes).
- Prescribe postoperative medications [antibiotic-steroid combination solution (0.1% dexamethasone/0.3% tobramycin or equivalent], four times a day for 1 week.
- Instruct the patient to watch for symptoms of infection (e.g., dull, aching pain or discomfort, with or without photophobia) at any point in the postoperative period.
- Remind the patient to contact his or her doctor if any of these symptoms occur.
- Advise the patient to avoid rubbing the eye (may lead to segment migration or improper healing of the incision).
- Apply an antibiotic-steroid combination ointment or solution (0.1% dexamethasone and 0.3% tobramycin or equivalent) to the operative eye at the end of the procedure.
The Immediate Postoperative Period (Days 1-7)
Expected Results
- good visual acuity (majority of patients see better than 20/40)
- Advise patient that over the next 3 to 6 weeks visual acuity will be good but may fluctuate from day to day and even during the course of the day.
- Advise patient who does not have 20/40 vision that refractive surgery procedures typically require some recovery time and that vision will most likely improve.
- Advise patient that over the next 3 to 6 weeks visual acuity will be good but may fluctuate from day to day and even during the course of the day.
- good intraocular pressure
- possible astigmatism
- No intervention is necessary.
- epithelium healing
- Healing is usually complete and foreign-body sensation resolved by the end of the first week.
COMPLICATIONS Several complications may be observed during the first week of postoperative recovery.
Epithelial Defect
- usually measures about 2×2 mm at the end of surgery
- rare incidence of adverse events (1.1% during U.S. clinical trials)
- symptoms
- decreased visual acuity (usually slightly less at day 3 than on day 1, secondary to superficial punctate keratitis from the topical medications and increased suture-induced astigmatism as the superior corneal edema in the region of the incision resolves)
- diurnal fluctuating vision (usually reported by patient because he or she generally self-tests his own visual acuity in the operative eye* 6-20 times per day)
- pain (but no patient discomfort from a peri-incisional epithelial defect located under the upper lid)
- diurnal fluctuating vision (usually reported by patient because he or she generally self-tests his own visual acuity in the operative eye* 6-20 times per day)
- decreased visual acuity (usually slightly less at day 3 than on day 1, secondary to superficial punctate keratitis from the topical medications and increased suture-induced astigmatism as the superior corneal edema in the region of the incision resolves)
foreign body sensation (if epithelium has not yet healed)
photophobia
- findings
- possible mild subconjunctival hemorrhage and/or chemosis remaining from the VCG
- little to no intraocular inflammation
- possible mild subconjunctival hemorrhage and/or chemosis remaining from the VCG
- management
- Half of cases almost entirely resolve by the first postoperative day and most others completely resolve by day 3.
- Attempt to bury suture knots, if not already done.
- Provide a bandage contact lens to be worn until the defect heals.
- If the epithelial defect is larger than 2×2 mm, use a bandage contact lens or mild patching. (Beware of excessive pressure on the dome of the cornea that could cause movement or malpositioning of the segments.)
- Monitor bandage contact lens use (prolonged contact lens wear may aggravate superficial neovascularization to the superior aspect of the incision).
- Discontinue the bandage contact lens as soon as the epithelial defect resolves or when limbal vascular buds form.
- Half of cases almost entirely resolve by the first postoperative day and most others completely resolve by day 3.
Filamentary Keratitis
- usually a single filament extending from the end of the incision (causes disproportionate discomfort to the patient)
- symptoms
- foreign body sensation
- photophobia
- foreign body sensation
- findings
- occasionally may develop as the epithelial defect heals
- management
- Treat with debridement, hypertonic saline drops (5% sodium chloride), or a bandage contact lens.
- See Epithelial Defects section for information about monitoring and removing bandage contact lenses.
- Treat with debridement, hypertonic saline drops (5% sodium chloride), or a bandage contact lens.
Drug Toxicity and Allergies
- symptoms
- foreign body sensation
- eye irritation
- foreign body sensation
- findings
- superficial punctate keratitis
- extensive chemosis [possible allergic reaction to topical medications unless surgery involved significant trauma (i.e., difficulty with VCG placement or prolonged application of the VCG)]
- lid edema
- lid erythema
- superficial punctate keratitis
- management
- In the presence of severe conjunctival chemosis in the early postoperative period, shift topical medications to an increased dose of topical steroids.
Infection
- symptoms
- significant ocular discomfort or pain
- photophobia
- decreased vision
- ocular discomfort and photophobia (one patient in U.S. clinical trials for PMA Cohort who had infectious lamellar infiltrates)
- significant ocular discomfort or pain
- findings
- infiltrate at incision
- infiltrate in tunnel
- cultured Staphyloccus epidermidis (in the one case where an infectious infiltrate was identified in the U.S. clinical trials for the PMA Cohort, which suggests that it may have been introduced at the time of surgery, perhaps because of contact of the Intacs or instruments with the lid margin or the “lacrimal lake”)
- infiltrate at incision
- management
- See all patients who call with complaints of rapid onset of discomfort and photophobia as soon as possible.
- Suspect infection in rapidly progressive infiltrates that appear in the first or second postoperative week.
- Manage infiltrates that progress more rapidly, however, with aggressive topical fortified broad-spectrum antibiotic therapy.
- If the infiltrates progress more slowly, fortified topical antibiotic therapy and systemic antibiotic therapy may lead to quick resolution.
- Consider removal of Intacs.
- See all patients who call with complaints of rapid onset of discomfort and photophobia as soon as possible.
Corneal Edema
- peripheral or central corneal edema and recurrent or extended corneal edema (rare)
- mild corneal edema from placement, removal, or replacement of Intacs or other refractive procedures (routine)
- symptoms
- blurred vision
- management
- Prescribe or increase the dosage of topical corticosteroids.
Suture-Induced Astigmatism
- symptoms (associated with induced astigmatism or undercorrection)
- glare
- halos
- double images
- blurred vision
- glare
- findings
- with the rule astigmatism (not coupled)
- steepening along the 90-degree meridian, which leads to additional steepening along the 180-degree meridian (perhaps from blunting of the typical flattening that occurs in the opposite meridian with suture-induced astigmatism)
- For example, a −2.00 + 2.00 X 90-degree refraction prior to suture removal shifts to piano after suture removal.
- undercorrection
- use of 10-0 nylon, more than one suture, tight suture closure, wound dehydration during surgery, and wound maceration or excess manipulation during surgery (all increase risk)
- with the rule astigmatism (not coupled)
- management
- If induced astigmatism is at least 1.00 D, identify the probable source of the astigmatism.
- Astigmatism related to over-tensioning of the incision sutures (i.e., with the rule astigmatism) typically diminishes over time.
- If there is more than 1.00 D with the rule astigmatism and sutures are still in place after day 7, remove the sutures.
- Address suture-induced astigmatism early if the incision is healed and does not stain with fluorescein.
- If induced astigmatism is at least 1.00 D, identify the probable source of the astigmatism.
The Intermediate Postoperative Period (Weeks 1-4)
Expected Results
- no ocular discomfort or inflammation
- uncorrected visual acuity (UCVA) typically better than 20/40 (fluctuates from day to day and during the course of a day, usually in proportion with the induced astigmatism)
COMPLICATIONS Several complications do not become apparent until later during recovery.
Induced With-the-Rule Astigmatism
- a myopic shift in the spherical equivalent (Intacs may blunt the concomitant flattening usually seen with suture-induced astigmatism)
- symptoms
- astigmatic blur
- double vision
- astigmatic blur
- findings
- a long incision with limbal encroachment
- visible incision and suture scarring
- elliptical decentration
- with the rule topographic changes
- too tight sutures or those left in place too long (according to current clinical data, may result in prolonged or even permanent with-the-rule astigmatism, even after suture removal)
- a long incision with limbal encroachment
- management
- Administer topical corticosteroids to carefully modulate overly aggressive wound healing during the initial postoperative period.
- Reincise the original incision and suture loosely or leave the incision unsutured for those patients who have corneas that healed aggressively. (This strategy has had only very limited success in a very small number of patients with astigmatism. Available clinical data have not demonstrated consistent results.)
- Selective suture removal may be necessary if the induced astigmatism is greater than 1.00 D at 2 weeks.
- Remove sutures by 4 weeks.
- Administer topical corticosteroids to carefully modulate overly aggressive wound healing during the initial postoperative period.
Induced “Against-the-Rule” Astigmatism
- symptoms
- double vision
- astigmatic blur
- double vision
- findings
- “against-the-rule” topographic changes
- incision wound gape
- cysts
- epithelial plugs
- inadequate wound closure
- wound trauma (e.g., blunt force or eye rubbing)
- flatter than average preoperative asphericity
- “against-the-rule” topographic changes
- management
- Remove any epithelial cysts or plugs.
- Debride the incision or reapproximate the wound edges and resuture the wound as appropriate.
- Remove any epithelial cysts or plugs.
Corneal Thinning
- symptoms
- foreign body sensation
- findings
- epithelial breakdown or staining over Intacs
- shallow Intacs placement (typically when placed at <30% depth)
- epithelial breakdown or staining over Intacs
- management
- Recommend early intervention to prevent corneal thinning.
- Remove Intacs immediately.
- Recommend early intervention to prevent corneal thinning.
- Make a new intrastromal tunnel at the appropriate depth (68% of pachymetry reading).
- Reposition Intacs.
Infiltrates
- may be infectious or sterile
- symptoms
- eye redness
- photophobia
- eye redness
- findings
- focal whitish infiltrate
- iritis
- epithelial streaming
- poor wound healing
- incomplete wound closure
- presence of a foreign body (e.g., stromal debris, fiber)
- inadequate steroid dosing
- focal whitish infiltrate
mechanical trauma
- management
- Administer combined antibiotic and steroid treatment (even though some may self-resolve over time).
Intacs Displacement
- may be vertical or lateral
- symptoms
- glare
- starbursting
- halo
- variable visual acuity
- glare
- findings
- inferior or superior placement or irregular astigmatism (vertical displacement)
- inadequate centration mark during surgery, incomplete tunnel dissection, incomplete advancement of Intacs, aggressive eye rubbing by patient, or segment movement within the intrastromal tunnel (vertical decentration)
- mismatched pupil center to surgical center of the Intacs, irregular topography, or irregular astigmatism (lateral displacement)
- decentered intrastromal tunnel, poor VCG placement or loss of suction during surgery, aggressive eye rubbing by patient, oversized pocket superiorly, or removal of Intacs and replacement with segment movement within the intrastromal tunnel (lateral decentration)
- inferior or superior placement or irregular astigmatism (vertical displacement)
- management
- Replace Intacs and properly align the new lens on the pupillary center.
Large Pupils
- symptoms
- Intacs edge visible to patient
- glare
- starbursting
- Intacs edge visible to patient
- findings
- large pupil in dark environment
- mismatched pupil to surgical center of Intacs
- poor Intacs placement
- decentered intrastromal tunnel
- segment movement within the intrastromal tunnel
- large pupil in dark environment
- management
- Carefully select patients to avoid large-pupil issues.
- Remove or reposition the Intacs if decentration is the main issue (may self-resolve over time).
- Carefully select patients to avoid large-pupil issues.
Epithelial Plug Formation in Incision
- management
- Intervene as soon as possible after observing the plug.
- Remove the incision sutures (if present) and debride and resuture the incision area.
- Follow the patient closely for 2 weeks to ensure adequate incision closure.
- Intervene as soon as possible after observing the plug.
The Late Postoperative Period (Month 2 and Beyond)
Between months 1 and 3 the surgeon should begin assessing whether the patient is satisfied with his or her vision and is “20/Happy.” Follow satisfied patients on a routine basis after the six-month examination.
Expected Results
- stabilized visual acuity by month 3
- refractive stability typically maintained after month 3 (usually <1.00 D of shift in the spherical equivalent between subsequent visits)
- gradual resolution of any induced astigmatism (high degrees of cylinder should continue to resolve over time)
- positioning hole deposits (nonprogressive and clinically inconsequential)
- usually appear 3 to 6 weeks postoperatively
- filling of a small manipulation hole used for final positioning of Intacs at the superior end of each Intacs segment with an opalescent substance (documented on a limited basis as proteoglycan, collagen, and keratocytes)
- usually appear 3 to 6 weeks postoperatively
COMPLICATIONS In general, late complications of Intacs placement are rare.
Intrastromal Tunnel Deposits
- generally appear between 3 and 12 months postoperatively
- findings
- observed in 68% of the U.S. Phase III clinical trial patients at the month 12 exam
- remain confined to the intrastromal tunnel (do not spread centrally into the visual axis)
- rarely, lead to confluent accumulations of opalescent material limited entirely to the dissected intrastromal tunnel
- may become visible to the naked eye
- from month 6 to month 12, prevalence and levels of deposits remain stable
- causes not yet conclusively established
- observed in 68% of the U.S. Phase III clinical trial patients at the month 12 exam
Pannus and Deep Neovascularization
- findings
- prior contact lens wear
- preoperative pannus
- incision extending to the limbal vessels during surgery
- wound healing issues (e.g., neovascularization in incision)
- loose sutures
- prior contact lens wear
Undercorrection or Overcorrection
- findings
- vessel growth
- management
- Before considering replacement, perform a cycloplegic refraction and evaluate topography.
- Where appropriate, discuss options including replacement.
- Prescribe topical corticosteroids to stop vessel growth once present.
- Advanced vessel growth that does not respond to topical corticosteroids may require laser therapy to impede deep vessel growth.
- Replace Intacs with thinner or thicker segments, depending on the residual refractive error (currently, insufficient data on efficacy of exchanging Intacs)
- Remove Intacs.
- See section on Removal and Replacement that follows.
- Before considering replacement, perform a cycloplegic refraction and evaluate topography.
Removal and Replacement
Intacs may be removed or replaced, unlike essentially permanent refractive techniques that directly cut or remove tissue and may be adjusted but not undone. Initial results of Intacs removal are very good although further analysis is needed. In FDA trials, only 6.9% of patients required removal in the first year.
Indications
- change in patient’s vision over time
- a clinically significant complication
- titration of the refractive effect with thicker or thinner Intacs
Expected Results
- within one line of preoperative BCVA
- no complications
- return of refraction to preoperative levels within 3 months (most cases)
- an additional effect because of replacement with thicker segments (6 procedures in FDA study)
Methods
ALTERNATIVE TREATMENTS
Intacs insertion is the first new refractive surgery technology to appear since laser in situ keratomileusis (LASIK), photorefractive keratectomy (PRK), and radial keratotomy (RK). LASIK, PRK, and RK were originally used to treat higher myopic patients, leaving patients with low myopia with very low hopes for laser vision correction.
The use of Intacs, LASIK, and intraocular lenses (IOLs) will most likely overlap somewhat, just as glasses, contact lenses, and refractive surgery have. Surgeons may choose among them based on their skill level, patient profiles, and practice environment.
Laser In Situ Keratomileusis
There has been no formal study of LASIK after initial Intacs insertion or LASIK and then subsequent insertion of Intacs, and no supporting data are available. However, anecdotal reports suggest that LASIK is effective after Intacs removal.
Characteristics
- similarities with Intacs
- use of topical anesthesia
- comparable visual results
- use of topical anesthesia
- dissimilarities with Intacs
- ability of Intacs to be placed (and if necessary, removed or replaced) without disturbing the visual axis
- better quality of vision with Intacs according to available single-site data
- ability of Intacs to be placed (and if necessary, removed or replaced) without disturbing the visual axis
Suggested Readings
Asbell PA, Ucakhan OO, Durrie DS, Lindstrom RL. Adjustability of refractive effect for corneal ring segments. J Refract Surg. 1999;15:627-631.
Burris TE, Baker PC, Ayer CT, et al. Flattening of central corneal curvature with intrastromal corneal rings of increasing thickness: an eye-bank eye study. Cataract Refract Surg. 1993;9(suppl):182-187.
Fleming JF, Lovisolo CF. Intrastromal corneal ring segments in a patient with previous laser in situ keratomileusis. J Refract Surg. 2000;16: 365-367.
Twa MD, Hurst TJ, Walker JG, Waring GO, Schanzlin DJ. Diurnal stability of refraction after implantation with intracorneal ring segments. J Cataract Refract Surg 2000;26:516-523.
Twa MD, Karpecki PM, King BJ, Linn SH, Durrie DS, Schanzlin DJ. One-year results from the phase III investigation of the KeraVision Intacs. J Am Optom Assoc. 1999;70:515-524.
< div class='tao-gold-member'>



