(1)
St. Johns, FL, USA
(2)
Helen Keller Foundation for Research and Education, International Society of Ocular Trauma, Birmingham, AL, USA
(3)
Consultant and Vitreoretinal Surgeon, Milos Eye Hospital, Belgrade, Serbia
(4)
Consultant and Vitreoretinal Surgeon, Zagórskiego Eye Hospital, Cracow, Poland
This chapter discusses the technical issues of dealing with different types of membranes inside the vitreous cavity.1 Additional details2 about these membranes are discussed either here or in various chapters in Part V.
32.1 ILM3
32.1.1 Instrumentation and Infrastructure
Pearl
Repeatedly grabbing hard membranes (in PVR or PDR) with the ILM forceps can cause enough “microtrauma” to the closing surfaces that they will not work on the ILM anymore.
If the membrane is infinite (no edge initially), it is the width of the jaws’ tip that determines the area of contact between the forceps and tissue. Once an edge is present, the entire jaw surface can make contact with it.6
The greater the width of the ILM forceps, the more secure the grip and the less likely that it tears the ILM. However, increasing the width also interferes with the visual feedback the surgeon has over the depth of contact between forceps and ILM.
The plano-concave contact lens should be scratch-free and fully transparent.
Using the smallest amount of visco, rather than lots of it, also helps, provided the amount is sufficient not to trap any air bubble under the lens. Still, the nurse should have at hand a tool such as a muscle hook to be able to gently nudge the contact lens if it slides and needs to be re-centered.
Increase the zoom as much as possible – find a compromise between image size and sharpness.
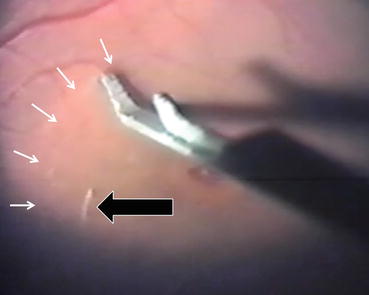
Fig. 32.1
Recognizing the unstained ILM. In this eye with macular hole, the unstained ILM has been incised with a barbed MVR blade. The lower blade of the forceps (Storz #E 1964 20 g; Bausch + Lomb, St. Louis, MO, USA) is pushed between the ILM and the nerve fibers and used as a spatula to separate them in a larger area. The two signs that give away that the lower jaw of the forceps is in the correct plane are the circumscribed light reflex (black arrow) and the faint semicircle of discoloration (white arrows)
32.1.2 Opening the ILM
Unlike all other membranes inside the vitreous cavity, the ILM has no free edge to grab: it must be surgically opened before it can be removed. The ILM can be opened in two ways: sharp or blunt.7
32.1.2.1 Sharp Opening: Incision First
Sharp opening of the ILM involves the use of a barbed8 needle (see Sect. 13.2.3.1).
Place the tip of the hook over the retina at a convenient and safe location9 (see Fig. 32.2) so that the tip barely touches the ILM surface. Avoid all visible blood vessels.
Fig. 32.2
The location of the initial ILM incision. (a) In this right eye with a macular hole, the surgeon places the barbed needle, held in his dominant right hand, in the superonasal area from the fovea. Ideally, the direction of the slice follows the course of the nerve fibers so that even if the incision is too deep, the damage will be limited. The incision avoids all visible vessels to reduce the risk of bleeding. (b) The ICG-stained ILM is opened with a barbed 23 g needle
Once your hand is truly steady, gently push down with the barb.
Slowly drag the barb, parallel to the retinal surface, a millimeter or so. The stained ILM will produce a visible flap, indicating that it has been incised. The opening should be at least as wide as the jaws of the forceps.
Take a forceps and grab the flap and then peel the ILM (see below).
In principle, working with a sharp tool is the least traumatic way to open the ILM. The surgeon needs to control no more than a single maneuver at a time – the depth to which the tiny hook is sunk into the retina first and then moving the tool “in plane”10 and even that over a little distance only.
Q&A
Q
Is it not a contradiction to say that a sharp tool is safer than a blunt one?
A
No – as long as the surgeon is able to control the depth to which he pushes the barb into the retina. With forceps, there are additional variables to control (see below). The third option, the scraper, is even more dangerous, precisely because the surgeon gives up control (see below).
32.1.2.2 Blunt Opening: No Incision
Blunt opening of the ILM is possible in two very different ways: via a primarily vertical movement (forceps) and a primarily horizontal one (scraper).
The ILM Forceps11
The advantage of this technique is that the same tool is used to tear and then peel the ILM. The disadvantages include the difficulty controlling the depth (so as to avoid tearing the nerve fibers, which run just beneath the 2 μ thick membrane) and the complexity of the maneuver.
Place your forceps over ILM (see above the site-selection criteria).
All current forceps designs are such that the tip of the jaws is perpendicular to the axis of the jaws – none is slanted. Since the jaws face a concave surface, the initial contact point of the forceps should be rather posterior so that the tip is parallel with the retinal surface (see the concept under Sect. 24.1). Moving it too peripherally means that only the corner-edge of the tip of the jaws, a very tiny area, will be able to grab the ILM (see Fig. 32.3).
Fig. 32.3
Schematic representation of the point of attack with the ILM forceps. If the forceps is used rather centrally within the vascular arcade, the tip of the forceps is parallel with the retina (R), allowing the surgeon to grab the ILM with the entire width of the forceps (F 1). If he tries to grab it further away from the central area, only the edge of the tip will make contact (F 2), increasing the likelihood that the ILM will tear or that he pushes the forceps too deep
Gently press down with the forceps. The depth should be just enough to create a depression so that when the jaws will be closed, a loop of ILM is caught but no nerve fibers (see Fig. 32.4).
Fig. 32.4
Schematic representation of grabbing the intact (unincised) ILM with forceps. (a) Left: the forceps approaching the ILM. Right: the forceps closing too early; no ILM between the jaws. (b) Left: too deep a grasp will result in picking up deeper retinal layers as well as the ILM. Right: blown-up image showing nerve fibers, seen clinically as white “fluff,” between the forceps jaws (shown for demonstration purposes with the forceps open). (c) Left: perfect grabbing of the ILM. Right: blown-up image showing that only the 2 ILM layers and no nerve fibers are caught by the forceps jaws (shown for demonstration purposes with the forceps open). F forceps, I ILM, R retina
Close the jaws.
Pearl
The most common error the inexperienced surgeon commits is to combine all movements into a single motion, instead of separating it into its basic elements. (1) Have your wrist firmly supported and keep your little finger on the patient’s forehead. (2) Position the forceps over the ILM in the selected area. (3) Close the forceps ~80% so that the ILM will easily fit into the jaws yet the distance your fingers will have to travel to close the jaws is shortened. (4) Push down with the forceps so that the ILM bulges as a loop in-between the jaws. (5) Close the jaws. (6) Lift the forceps. (7) Repeat all steps if there is no purchase.
Lift the ILM gently and hold it for a few seconds. The ILM is rigid and will rip.
Start peeling it in a certain, predetermined direction and angle.12 Even if the ILM tears subsequently – and it will – from now on, you will have an edge to grab, which is much easier (see below).
The Scraper
The diamond-coated instrument is repeatedly dragged over the ILM until the membrane breaks: the main vector component of the movement is parallel with the retina.
However, the silicone flap of the scraper must also be pressed downward to allow engagement of the ILM. The surgeon has no visual control over how much downward pressure is exerted.
Once the ILM has been opened, accidentally dragging the diamond crystals over the now-denuded nerve fibers instantly becomes possible, and tearing of the nerve fibers is almost inevitable. This is especially dangerous if the surgeon is not using an effective dye so that he knows exactly over which surface not to use the scraper.
Q&A
Q
Should the scraper be used to open the ILM?
A
No. A surgeon who uses the scraper for opening the ILM gives up control in favor of apparent ease. The risk of such a maneuver far exceeds its benefits.
32.1.3 Peeling the Membrane
Once the ILM has been opened, the surgeon’s task becomes much easier, since now he has a clear edge to grab.13 Although peeling can also be done with the probe (under constant aspiration, with the probe turned away from the retinal surface) or the scraper14 (flipping the ILM over, similar to how the barbed needle is used to complete the capsulorhexis), it is best performed using forceps.
Grab the edge of the ILM.
The two areas where ILM grabbing should be avoided are the center of the fovea and the maculopapillary bundle, especially if close to the disc margin. If the ILM tears here, try to peel the ILM from elsewhere toward/into these areas.
Pull it at an acute angle in a predetermined direction.
It is almost inevitable that the ILM will tear multiple times, not come off in a single piece.15
If repeated tearing occurs in a small area (several small pieces are torn off), change the direction of pulling (see Fig. 32.5).
Fig. 32.5
Schematic representation of reducing the risk of ILM tearing during peeling. Surgeon’s view. (a) If the ILM keeps tearing in the intended direction of pulling (white arrow), change the direction (granite arrow). (b) Once a larger ILM piece is removed in that area, return to the original site (shown by the granite star) and grab/pull the ILM as initially intended (white arrow) but with a slight modified peeling direction. R retina, ILM already removed, I are where the ILM is still present, F forceps
Especially in eyes with thickened ILM or increased adhesion, the ILM may have to be regrabbed many times. This alone represents a higher risk of causing retinal damage, even if the forceps is in the hands of the most experienced and cautious surgeon (see Fig. 32.4b).
Pearl
The sight of white, fluffy material in the jaws of the forceps signals that the surgeon grabbed nerve fibers, not (only) the ILM.
Never forget that, even if the risk is low, the retina may tear16 if the ILM is very adherent and/or the retina is already damaged.
The appearance of small hemorrhages17 if typical. They rarely occur as a result of direct forceps damage (i.e., they are not found at the point of grabbing); as the ILM is separated, the wall of a small vessel is broken. The bleeding usually spontaneously disappears in a day and without clinically detectable consequences.
Very rarely, the ILM is so adherent to the wall of a major vessel that the peeling will tear the vessel’s wall and cause a significant bleeding. Most commonly, however, the ILM actually tears along the vessel: the border of the peeling will be congruent with the course of the vessel.
Always proceed slowly and keep a close watch over the (advancing) border where the ILM separates from the retina.
Although it is practically impossible to visually appreciate the curvature of the eyewall, remember that you work over a concave tissue, not a flat surface. If you do not simultaneously watch the advancing tip of the forceps, you may bump it into the retina (see Fig. 32.6). The greater the distance between the forceps’ tips and the border of ILM separation, the higher the risk of bumping into the retina.18
The peeled area may rapidly turn white. This discoloration, probably caused by temporary edema, spontaneously disappears within hours and without clinically detectable consequences.
The peeling technique greatly depends on whether the macula is healthy or unhealthy (see Sect. 49.2).
Inevitably, small ILM fragments get stuck to the forceps jaws. Remove them (see Fig. 32.7) before you attempt to regrab the ILM: the fragments interfere with visualization, not allowing you to see how deep into the retina you push the forceps jaws. They also make the regrabbing more difficult.
The vitreous cavity will contain numerous ILM floaters by the end of the peeling; carefully collect all of them before the completion of the operation.
Fig. 32.6
Schematic illustration of the risk of retinal “bumping” during ILM peeling. The forceps (F 1) approaches the retina (R) and F2 picks up the ILM (black line). If the surgeon monitors only the advancing separation between ILM and retina (arrow), but not the distance between the tip of the forceps (F 3) and the retina, the forceps will hit the arching retina at some point (black star). The danger is increased if the ILM held in the forceps is a long piece and if the forceps must be kept close to the retina (edema-damaged retina; see Chap. 49)
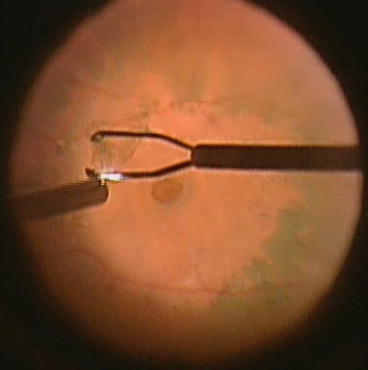
Fig. 32.7
Getting rid of a small ILM fragment stuck to the forceps jaws. In this picture the ILM is stuck to the jaw that is closer to the surgeon (the inferior one as viewed on the image). Twang that jaw with the light pipe after you brought the forceps to the light pipe – not the other way around so that you are away from the retina. Do not push the light pipe between the jaws but do the twang outside-in
32.1.4 The Extent of ILM Peeling
How far to carry the ILM removal varies with the condition, but it is mostly the individual surgeon’s decision; there is no proven recommendation about the size of the area. A few things need to be kept in mind.
Except for a few eyes with high myopia, there is no ILM over the optic disc. Occasionally, a tiny hole is seen in the ILM over the foveola.
The ILM may be missing over the major vessels: the tearing will occur exactly over them (see above). This is why ILM peeling is rarely extended beyond the arcades.
Outside the major vessels, it becomes very difficult and eventually impossible to peel.
In eyes with RD, especially if at high PVR risk, as large an area as possible should be peeled (see Table 54.9). Fortunately, in this scenario it is relatively easy to peel beyond the vascular arcades.
32.1.5 What If the ILM Cannot Be Peeled?
Although it is very rare that the ILM is impossible – or too risky – to remove, it may occur in the following cases:
There is no PVD. With vitreous on the retinal surface, the ILM will tear, as it is too weak to withstand the weight of the gel (see Table 32.1).19
Table 32.1
Indicationsa for ILM peeling
Indication
Comment
“Assuring the PVD has been done”
This is a rather nonsense of an argument. ILM removal is not the correct way to achieve PVD; in fact, the presence of the vitreous cushion on the retinal surface interferes with ILM removal: the ILM tears under the weight of the vitreous. Conversely, very fine proliferative membranes may be removed together (as one piece) with the ILM (see below) – but in these cases the ILM comes off with the epiretinal membrane, not vice versa
BRVO
Sheathotomy at the arteriovenous crossing, in addition to dealing with macular edema (see below)
Cellophane maculopathy
To remove the diseased surface and to prevent continual/recurring growth
EMP
To ensure that all of the proliferation is removed and eliminate the risk of recurrence
Hemorrhagic macular cyst in Terson syndrome
In the submembranous type, the blood-accumulation is under the ILM; once detached, the ILM never readheres
Macular edemab
To help dry out, and keep dry, the retinac
Macular hole
To increase the success rate by eliminating all traction forces
Optic pit
A somewhat controversial indication since ILM removal can also weaken the already damaged retina on one hand, but may, on the other hand, help if a macular hole is present
PDR
Removal of current, and prevention of subsequent, membranes growing on the macular surface, in addition to dealing with macular edema (see above)
Prophylactic
Against the future development of EMP or edema, which may threaten in many diseases as well as the result of the treatment itself
PVR
Complete removal of current, and prevention of subsequently developing, membranes on the macular surface
RD
To prevent EMP formation and treat the edema in long-standing cases
Staphyloma-spanning central RD
Removal of the rigid ILM allows the remaining, elastic neuroretina to conform to the eye’s increased concave contour at the posterior pole
VMTS
To ensure that the traction is completely relieved
Similarly, thick EMPs do not allow ILM removal (see below).
Highly adherent ILM. This may be the case in very young children and some diabetics. It is a judgment call whether to continue or abandon – and if yes, at what point – the peeling.20
The highly myopic eye. The staining is usually faint, even with ICG, and the contrast is very weak, due to the depigmentation of the posterior pole. In addition, the retina is extremely thin,21 further increasing the risk (see Chap. 42).
Although technically very difficult and associated with an increased chance of iatrogenic retinal damage, ILM removal in these eyes has extreme benefits; a careful consideration of risk vs benefit is needed.
32.1.6 ILM Removal in Eyes with Detached Macula
The ILM is usually easier to remove from areas of detachment, but the detachment also presents unique challenges. The surgeon has two options to peel the ILM over a detached macula.22
32.1.6.1 Reattaching the Macula First
Inject enough PFCL to reattach the macula.24
Peel the ILM. There are two major differences compared to peeling under BSS and over previously not detached retina.
The ILM tears easily, and the free edge instantly gets pressed against the retina by the weight of the PFCL, making the regrabbing technically more difficult.
The retina is mobile25: the forceps drags the retina along, however minimally.
32.1.6.2 Peeling When the Macula Is Still Detached
Stain the ILM with ICG.
Drain the subretinal fluid as much as possible to reduce the height of the detachment, but do not perform F-A-X.
Begin the peeling just above the maculopapillary bundle at the disc margin (see Fig. 32.8).26
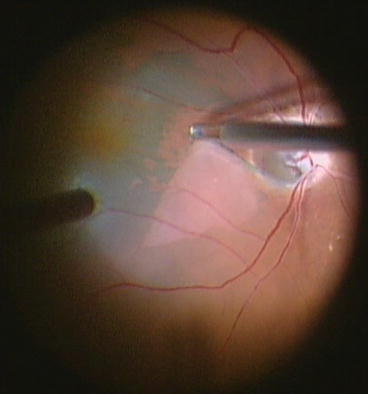
Fig. 32.8
Peeling the ILM over detached retina. The peeling is started much closer to the disc margin than is usual (see Fig. 32.2a ). The peeling direction is always away from the disc to reduce the movement of the retina and to provide a counterforce against the vector of the peeling. The retina is lifted (tenting) as the forceps is dragging the ILM and the retina temporally: a white line is visible at the border of ILM separation. The same phenomenon is noticed if a strongly adherent ILM is peeled in an eye with severe macular edema (see Fig. 49.3)
The direction of the peeling is always away from the disc, where the retina is fixated.
Even though the ILM will separate in atypically large sheets, regrabbings are still necessary; it is easier to grab too deep if the retina is detached.27
32.2 EMP
Although some ophthalmologists try to “treat” the patients with anti-VEGF injections, this obviously addresses only one of the consequences of the membrane (ME), not the cause. What offers definite cure is PPV with removal of the EMP.
Pearl
In the vast majority of eyes with EMP, a spontaneous PVD is present at the time of PPV.
32.2.1 The Clinical Characteristics of the EMP28
The membrane may be any of the following “pairs” – or something in between.
Very thin or extremely thick.
Small or large, spreading outside the field accessible through the contact lens without moving the microscope.
Made up of a single or multiple layers.29
Surrounded by retina that has several or no folds.30
Located in the epicenter or parafoveally.
During peeling, the membrane will prove to be very adherent to, or simply located on top of, the retina.31
During peeling, the membrane will prove to be rigid or fluffy. The latter is much more difficult to peel because the membrane is elastic (composed mostly of cells). Occasionally it can give the surgeon the shivers since it resembles “peeling” of the nerve fibers (see above).
32.2.2 Removal Technique
32.2.2.1 Staining or Not?
Proper staining (see Sect. 34.2) helps identify the membrane and helps both in tactical decision-making and its execution.32 My personal decision-making related to the timing of staining is shown in Fig. 32.9a; b is a clinical example of the staining being useful.
Fig. 32.9




Staining the ILM in macular pucker surgery. (a) Decision-making flowchart: staining before or after EMP removal. (b) “Negative” staining of the EMP. On the left of the image, the ILM has been stained with ICG; on the right, the EMP prevented the underlying ILM from turning green. Otherwise, only the light reflex gives away the presence of the EMP; the membrane itself is barely visible. M membrane, R retina
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


