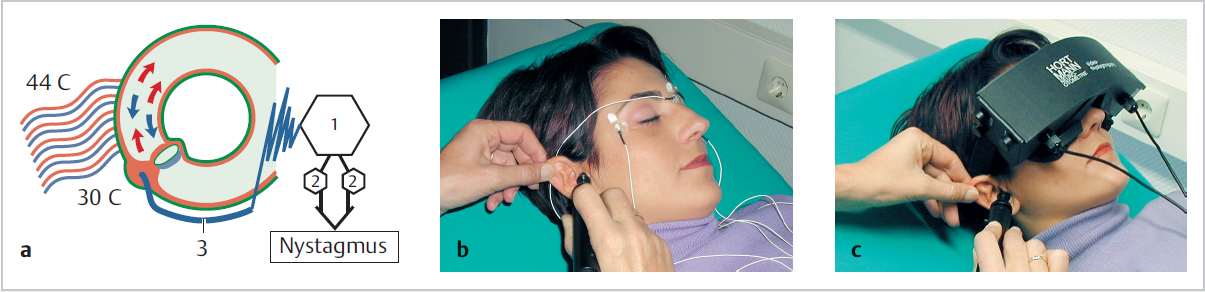
18 Vestibular Examination and Investigation • Most vestibular disorders are diagnosed from the history, but examination and sometimes investigation may be helpful • Need to assess various aspects that contribute to balance • EAC, TM (for COM), PTA (asymmetrical SNHL consider vestibular schwannoma), tuning fork testing • Fistula test: if bone over lateral Scc eroded by COM, exposes membranous canal: intermittent pressure on tragus induces vertigo/transient nystagmus; a fistula may also cause a Tullio phenomenon: vertigo with loud sounds (sound energy via mobile footplate to labyrinth) • Vestibulo-ocular reflex (VOR) maintains gaze stability during head movements (detected by labyrinth) • Ocular palsies (III n, IV n, VI n) suggest intracranial pathology • Nystagmus: a rhythmic, oscillating, involuntary movement of the eyes that may be horizontal, vertical, rotatory, or mixed; may be physiological or pathological (congenital, spontaneous, positional): – 1st degree: present when eyes deviated in direction of fast component – 2nd degree: present on central gaze – 3rd degree: when eyes deviated in direction of slow phase – Smooth pursuit: the response for slowly moving objects that keeps the target on the fovea; patient tracks a target moving sinusoidally (e.g., follows swinging pendulum); unilateral impairment implies CNS pathology, maybe cerebellar (bilateral more non-specific, may be drug-induced) – Saccadic eye movements: the response to objects that move out of the visual field requiring a restorative movement of the eyes (a saccade) to bring back to the fovea; patient looks back and forth between examiner’s fingers, separated horizontally or vertically; abnormalities imply central pathology (assuming normal ocular muscles) • Vestibulospinal response preserves appropriate muscle tone to avoid falling when environment is moving • Unterberger test (Fig. 18.1): mark time stepping on spot with arms outstretched, palms faced up, eyes closed; reduces input from proprioception and eyes; rotate to side of paralytic labyrinthine lesion (in the acute setting) • Romberg test: stand with feet together, arms by side, eyes shut; +ve if imbalanced (visual suppression); sway to side of lesion if labyrinthine problem; central cerebellar lesion gives symmetrical sway less affected by eye closure; can make test more sensitive to vestibular deficits by standing patient on 3″ (8 cm) foam or assessing them in tandem gait (removes proprioceptive input) • Heel/toe gait; failure implies central (cerebellar) component (if not during acute vestibular episode); gait with eyes closed—veers towards side of vestibular lesion (but non-specific) • General gait observation as patient walks • Hyperventilation: might reproduce symptoms • Cerebellar function (finger–nose, dysdiadokokinesis) • Other CNS • Consider cardiovascular examination (e.g., for postural drop in blood pressure, arrhythmias) • Vestibular function testing is rarely diagnostic, but may help to determine whether a condition is central or peripheral, uni- or bilateral • Physiology: • Caloric testing alters the temperature of endolymph to set up thermally induced convection currents that stimulates stereocilia and causes nystagmus and vertigo (Fig. 18.2a) • Stimulating temps are equally above and below body temp (30° and 44°C) • Only the lateral Scc is stimulated • Patient at 30° recline, thus putting the lateral Scc in the vertical plane • Cold water first, timing until nystagmus stops, then other ear, then warm water • Can use air to supply thermal stimulus when TM perforation • Can record nystagmus electrically (electronystagmography) or simply observe (Fig. 18.2b, c) • Tests in part the integrity of the VOR; the response should be symmetrical when both lateral Sccs are intact • Interpretation: cold causes nystagmus to opposite side, warm to same (COWS) • Formulas based on recorded times predict degree of vestibular activity • Unilateral canal paresis denotes response of one side is reduced or absent compared with other side; usually implies lesion of peripheral vestibular system; significant canal paresis is >20–25% • A directional preponderance (DP) denotes non-specific enhancement of nystagmus in one particular direction; suggests pathology but is usually non-localising (i.e., peripheral or central); significant if ~>20%; may be localizing with some peripheral lesions when DP is usually directed away from diseased ear • This testing relies on comparing the two ears, so if both impaired identically, will fail to demonstrate this • Electronystagmography (ENG) evaluates the VOR objectively • Best done with Frenzel lenses to prevent visual fixation that can inhibit nystagmus • Uses normal electrical potential between cornea and retina; eye movements alter this potential relative to surface electrodes placed around the eye
18.1 Diagnosis
18.2 Examination
18.2.1 Ear
18.2.2 Vestibulo-Ocular
 Slow phase beats to affected side, due to impulses from vestibule (or visually induced) if paralytic problem (most common)
Slow phase beats to affected side, due to impulses from vestibule (or visually induced) if paralytic problem (most common)
 Fast phase is what is described, the recovery movement, a central correcting (saccadic) reflex
Fast phase is what is described, the recovery movement, a central correcting (saccadic) reflex
 Nystagmus may be in part a failure of the VOR, due to peripheral (labyrinthine) or central pathology
Nystagmus may be in part a failure of the VOR, due to peripheral (labyrinthine) or central pathology
 If irritative vestibular problem (e.g., acute Ménière attack) nystagmus (fast phase) beats towards bad ear
If irritative vestibular problem (e.g., acute Ménière attack) nystagmus (fast phase) beats towards bad ear
 75% normal people get physiological nystagmus if eye deviates further horizontally than canaliculi, or when looking out of window of moving train (optokinetic nystagmus—indicates intact visual pathways)
75% normal people get physiological nystagmus if eye deviates further horizontally than canaliculi, or when looking out of window of moving train (optokinetic nystagmus—indicates intact visual pathways)
 Congenital nystagmus is present from birth
Congenital nystagmus is present from birth
 Spontaneous nystagmus present when patient sitting still, no external stimulus; increasing degrees of severity (Alexander law: in patient with vestibular lesion the nystagmus becomes more pronounced when patient looks in direction of the quick-phase):
Spontaneous nystagmus present when patient sitting still, no external stimulus; increasing degrees of severity (Alexander law: in patient with vestibular lesion the nystagmus becomes more pronounced when patient looks in direction of the quick-phase):
 If spontaneous nystagmus + dysequilibrium at the time = peripheral (otological) cause; usually fatigues
If spontaneous nystagmus + dysequilibrium at the time = peripheral (otological) cause; usually fatigues
 If spontaneous nystagmus + no dysequilibrium at the time = central cause
If spontaneous nystagmus + no dysequilibrium at the time = central cause
 Spontaneous nystagmus may be due to current drug therapy (e.g., benzodiazepines, phenytoin, barbiturates, which may be being taken for dysequilibrium)
Spontaneous nystagmus may be due to current drug therapy (e.g., benzodiazepines, phenytoin, barbiturates, which may be being taken for dysequilibrium)
 Positional nystagmus: e.g., when head in a specific position or moved quickly to a specific position Note: When testing eye movement in horizontal plane, failure of conjugate gaze (hence inability to move both eyes in the same direction) = internuclear ophthalmoplegia, a sign of multiple sclerosis
Positional nystagmus: e.g., when head in a specific position or moved quickly to a specific position Note: When testing eye movement in horizontal plane, failure of conjugate gaze (hence inability to move both eyes in the same direction) = internuclear ophthalmoplegia, a sign of multiple sclerosis
 Nystagmus (spontaneous) assessment; patient sits up, looking ahead and then 30° to either side; Frenzel glasses prevent visual fixation and make easier observation (enhance peripheral induced nystagmus, suppress central)
Nystagmus (spontaneous) assessment; patient sits up, looking ahead and then 30° to either side; Frenzel glasses prevent visual fixation and make easier observation (enhance peripheral induced nystagmus, suppress central)
 Dix–Hallpike test for positional nystagmus: +ve for BPPV if delayed rotatory nystagmus with distress that resolves; if central cause get sudden onset nystagmus without distress and no resolution
Dix–Hallpike test for positional nystagmus: +ve for BPPV if delayed rotatory nystagmus with distress that resolves; if central cause get sudden onset nystagmus without distress and no resolution
 Optokinetic reflex maintains visual fixation on a moving object when the head is stationary:
Optokinetic reflex maintains visual fixation on a moving object when the head is stationary:
 Head thrust/Halmagyi test: (patient fixes on target, e.g., your nose, as you turn head rapidly to each side); if refixation saccade back to target implies reduced vestibular function in plane of rotation for ear ipsilateral to thrust, because reduced input to VOR
Head thrust/Halmagyi test: (patient fixes on target, e.g., your nose, as you turn head rapidly to each side); if refixation saccade back to target implies reduced vestibular function in plane of rotation for ear ipsilateral to thrust, because reduced input to VOR
 Post-headshake nystagmus: (tilt head 30° forward and shake in horizontal or vertical plane, with patient’s eyes closed); if nystagmus, pathology in vestibular input in plane of rotation (odd nystagmus if central problem)
Post-headshake nystagmus: (tilt head 30° forward and shake in horizontal or vertical plane, with patient’s eyes closed); if nystagmus, pathology in vestibular input in plane of rotation (odd nystagmus if central problem)
 Dynamic visual acuity: (reading during headshake); reduced acuity probable vestibular problem; get oscillopsia, a visual blurring on head movement
Dynamic visual acuity: (reading during headshake); reduced acuity probable vestibular problem; get oscillopsia, a visual blurring on head movement
 VOR suppression test: (follow object that rotates with head, e.g., tongue depressor held in teeth, which has a pin stuck vertically in it); should be able to visually suppress vestibular signal, but if CNS pathology get nystagmus due to incomplete visual fixation
VOR suppression test: (follow object that rotates with head, e.g., tongue depressor held in teeth, which has a pin stuck vertically in it); should be able to visually suppress vestibular signal, but if CNS pathology get nystagmus due to incomplete visual fixation
18.2.3 Vestibulospinal
18.2.4 Other
18.3 Investigation
18.3.1 Calorics
 Sccs detect angular acceleration
Sccs detect angular acceleration
 Within ampulla of each canal have the crista on which sits the cupula
Within ampulla of each canal have the crista on which sits the cupula
 Endolymph fills the membranous canal and has inertia, so there is a relative difference in velocity of canal and the fluid with head movements; so fluid forced through gap between crista and cupula causing deflection of stereocilia, increasing or decreasing the resting tonic discharge depending on direction of deflection
Endolymph fills the membranous canal and has inertia, so there is a relative difference in velocity of canal and the fluid with head movements; so fluid forced through gap between crista and cupula causing deflection of stereocilia, increasing or decreasing the resting tonic discharge depending on direction of deflection
 The two labyrinths work in conjunction, so increase in neural signals from one is associated with decrease in other
The two labyrinths work in conjunction, so increase in neural signals from one is associated with decrease in other
 The three Sccs are at right angles so 3D information provided
The three Sccs are at right angles so 3D information provided
 Warm water causes endolymph to rise in lateral Scc, so deflecting kinocilium towards utricle and hence increasing firing rate; consider test on R ear—this response, via VOR, causes eyes to move to L, so the corrective response is a saccade to the R (so R-beating nystagmus)
Warm water causes endolymph to rise in lateral Scc, so deflecting kinocilium towards utricle and hence increasing firing rate; consider test on R ear—this response, via VOR, causes eyes to move to L, so the corrective response is a saccade to the R (so R-beating nystagmus)
18.3.2 Electronystagmography
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree