Upper Eyelid Blepharoplasty
Jonathan M. Sykes
Christina K. Magill
Upper eyelid blepharoplasty is a common and often straightforward procedure; however, there are multiple considerations that need to be applied to each patient having surgery of the upper eyelid in order to ensure safety and optimal results. It is critical that the patient’s underlying concerns and pathology are identified prior to surgery. A patient who desires cosmetic upper eyelid blepharoplasty must be counseled appropriately about realistic expectations, recovery time, and the details of elective surgery. The older patient who presents primarily with a complaint of decreased vision must be properly diagnosed: is there a change in visual acuity or ocular insult? Is brow ptosis or blepharoptosis contributing to the problem? Is the peripheral loss of vision primarily from excessive upper eyelid skin, also known as dermatochalasis? A proper assessment of the patient’s desires and applied anatomy will maximize surgical outcomes and minimize complications. Success in upper eyelid blepharoplasty is guided by an understanding of surgical anatomy, patient motivational and medical history, the use of preoperative photography, appropriate surgical technique, and avoiding potential complications. This chapter outlines the preoperative considerations and surgical techniques for upper eyelid blepharoplasty.
SURGICAL ANATOMY
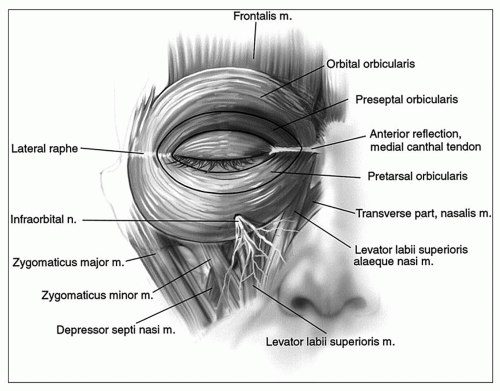
To perform upper eyelid blepharoplasty, a thorough understanding of the upper eyelid-brow complex, crosssectional anatomy of the upper eyelid, and anatomic composition of the eyelid crease is necessary (Fig. 186.1) (1). The eyebrow and the upper eyelid skin constitute the upper eyelid-brow complex. The upper eyelid-brow complex moves the eyelid during expression and serves a functional role. The frontalis muscle acts on the brow as an elevator, and the orbicularis oculi acts on the brow as a depressor during eye closure and facial expression. When evaluating the eyebrow, it is important to evaluate brow height, inclination, and orientation (2). The brow lies along the supraorbital rim in men in a relatively straight position. In women, the hair of the brow arches above the superior orbital rim at its lateral extent. As individuals age, the frontalis muscle can become atrophic and lax, allowing the brow to descend. In some patients, placing a finger on the eyebrow and returning it to its more youthful position may correct excess upper eyelid skin or loss of peripheral vision that would not be corrected with upper eyelid blepharoplasty alone (3).
In addition to evaluation of the upper eyelid-brow complex, an understanding of the tissue layers of the upper eyelid is critical to successfully perform upper eyelid blepharoplasty. There are several tissue layers in the upper eyelid, which are (from superficial to deep) skin, orbicularis oculi muscle, orbital septum, preaponeurotic fat, the levator aponeurosis, Müller muscle, and the tarsus and conjunctiva. A sagittal section of the upper lid can help illustrate the levels and depths of the upper lid retractors, fat compartments, and the tarsal plate (Fig. 186.2) (1).
The sectional anatomy of the upper eyelid begins with the skin. The upper eyelid skin is the thinnest skin in the body and is less than 500 microns thick. The skin of the upper eyelid is the thickest superiorly and the thinnest at the ciliary margin. Excess upper eyelid skin is often what patients wish to be surgically corrected.
Beneath the thin upper eyelid skin is the orbicularis oculi muscle. This muscle has a radial, sphincter-like pattern around the eye and is considered part of the superficial musculoaponeurotic system, mainly innervated by the zygomatic branch of the facial nerve. The muscle acts to close the eye, narrow the palpebral opening, and squint. The lateral ocular rhytids, or smile-lines that can appear in the skin over time, are perpendicular to the underlying orbicularis oculi muscle. The orbicularis oculi muscle can be very thin and easily incised along with the skin incision. Conversely, the orbicularis oculi muscle can also
be hypertrophic, causing lid thickening and excess eyelid squeeze (Fig. 186.3).
be hypertrophic, causing lid thickening and excess eyelid squeeze (Fig. 186.3).
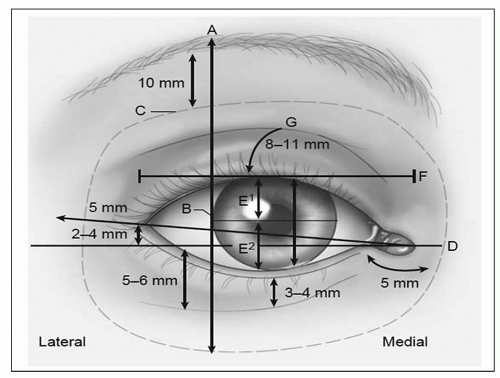 Figure 186.1 Topographic anatomy of the eyelids and eyebrow. (A) A vertical line drawn tangent to (B) the lateral limbus demarcates the highest point of the eyebrow. The inferior hair-bearing line of the eyebrow typically rests 10 mm above the superior orbital rim. (C) The orbit boundaries. (D) The lateral canthus is positioned 2 to 4 mm superior to the level of the medial canthus. (E1) The MRD1 is measured from the upper eyelid margin to the corneal light reflex at the level of the pupil. (E2) The lower eyelid margin measured to the corneal light reflex is the MRD2. The intrapalpebral distance is measured as MRD1 + MRD2 and ranges from 9 to 12 mm. (F) The palpebral width ranges from 28 to 30 mm. (G) The upper eyelid height ranges from 8 to 11 mm, depending on gender and ethnicity. (Adapted from Most SP, Mobley SR, Larrabee WF Jr. Anatomy of the eyelids. Facial Plast Surg Clin North Am 2005;13(4):487-492.) |
The tissues that lie deep to the orbicularis oculi vary from superior to inferior and include the frontal bone, orbital septum, and tarsal plate. At the level of the brow, the orbicularis oculi muscle is superficial to the frontal bone and the superior orbital rim. Inferiorly, the orbicularis oculi muscle lies superficial to the orbital septum above and the tarsus below. Three surgical designations of the orbicularis oculi exist according to the tissue beneath the muscle: there is an orbital, preseptal, and pretarsal portion (Fig. 186.4) (4). The fibrous tarsal plate is approximately 8 to 9 mm in height and acts as a skeletal component that shapes and supports the arch of the lid. In addition, the tarsal plate contains meibomian glands at its inferior border. There are several layers of the upper eyelid that fuse and insert onto the tarsal plate, including the orbital septum and upper eyelid retractors.
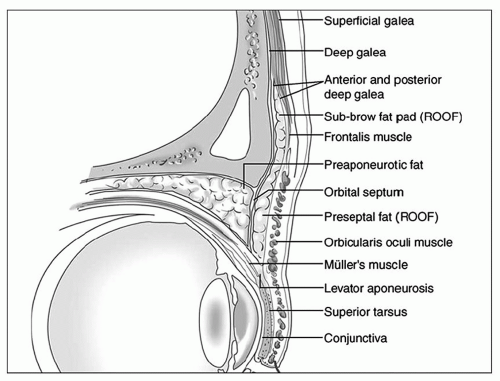 Figure 186.2 Sagittal section through orbit and upper eyelid. The superficial to deep anatomy of the upper eyelid is demonstrated. The thin upper eyelid skin overlies the orbicularis oculi muscle. Deep to the orbicularis oculi muscle is the orbital septum, which contains the preaponeurotic fat. The upper eyelid retractors are beneath the fat pad and consist of the levator aponeurosis and Müller muscle. (Adapted from Most SP, Mobley SR, Larrabee WF Jr. Anatomy of the eyelids. Facial Plast Surg Clin North Am 2005;13(4):487-492.) |
 Figure 186.3 Orbicularis oculi muscle hyperfunction. Static and dynamic excess eyelid squeeze are shown. |
The orbital septum begins superiorly at the superior orbital rim as a reflection of the frontal bone periosteum.
This reflection of the septum orbitale is called the arcus marginalis. The orbital septum has a white appearance (in contrast to the pink color of the orbicularis muscle) and acts as a barrier to infection. As the orbital septum becomes lax with age, underlying fat can prolapse anteriorly and inferiorly, and this can cause visible bulges beneath the thin eyelid skin.
This reflection of the septum orbitale is called the arcus marginalis. The orbital septum has a white appearance (in contrast to the pink color of the orbicularis muscle) and acts as a barrier to infection. As the orbital septum becomes lax with age, underlying fat can prolapse anteriorly and inferiorly, and this can cause visible bulges beneath the thin eyelid skin.
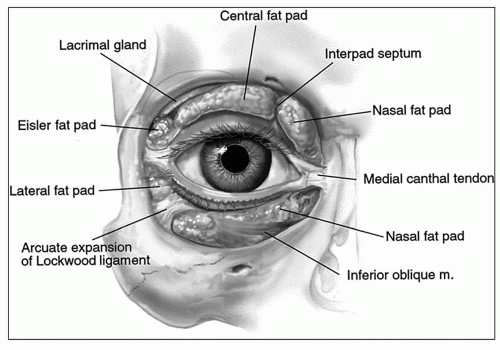
The orbital contents contained by the orbital septum include preaponeurotic fat and the lacrimal gland. The preaponeurotic fat includes a medial fat pad and a central fat pad (Fig. 186.5) (4). The fat pads, in addition to the lacrimal gland, can all descend as the orbital septum connective tissue relaxes with aging. The prolapse of fat can create bulging beneath the thin upper eyelid skin (5). The preaponeurotic fat pads can also become prominent in blepharochalasis, a condition marked by intermittent eyelid edema.
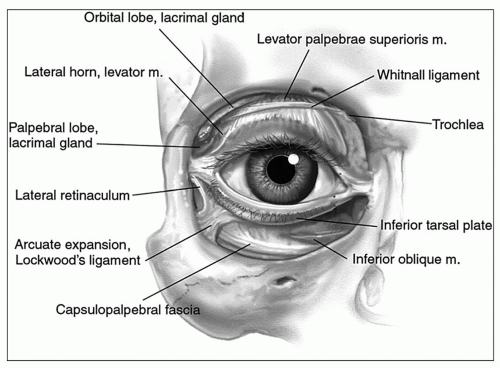
Deep to the preaponeurotic fat are the muscular upper eyelid retractors. The upper eyelid retractors include the levator palpebrae superioris muscle (levator muscle) and Müller muscle. The primary upper eyelid retractor is the levator muscle, which is suspended by the superior transverse (Whitnall ligament). Whitnall ligament extends from the fascia of the lacrimal gland laterally to the trochlea attachment medially. The ligament conceptually suspends the levator muscle and allows it to change directions (Fig. 186.6) (4). As the levator muscle descends from its superior condensation with Whitnall ligament, it becomes a thick aponeurosis that inserts onto the anterior face of the fibrous tarsal plate. The elevation of the tarsal plate by the levator muscle is controlled by motor fibers from the oculomotor nerve (cranial nerve III).
In contrast to the levator muscle, Müller muscle is an involuntary smooth muscle lid retractor that receives
sympathetic innervation. When sympathetic tone is absent, such as in Horner syndrome, the eyelid is noticeably ptotic by 2 mm. During dissection in the postseptal compartment of the upper eyelid, Müller muscle is found beneath the levator aponeurosis. An arcade of vessels travels on the anterior surface of Müller muscle.
sympathetic innervation. When sympathetic tone is absent, such as in Horner syndrome, the eyelid is noticeably ptotic by 2 mm. During dissection in the postseptal compartment of the upper eyelid, Müller muscle is found beneath the levator aponeurosis. An arcade of vessels travels on the anterior surface of Müller muscle.
The deepest layer of the upper eyelid is the conjunctiva, a clear mucous membrane that provides lubrication and protection to the sclera. The conjunctiva consists of a tarsal component that lines the undersurface of the eyelids, fornix, the apex of the orbit/eyelid junction, and a bulbar component that adjoins the sclera of the globe. Preserving the conjunctiva helps protect against corneal damage.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree