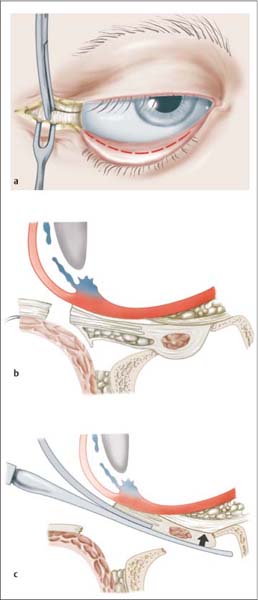
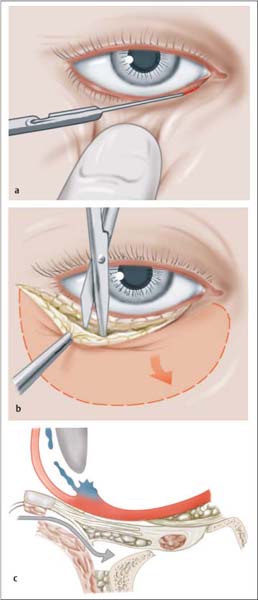
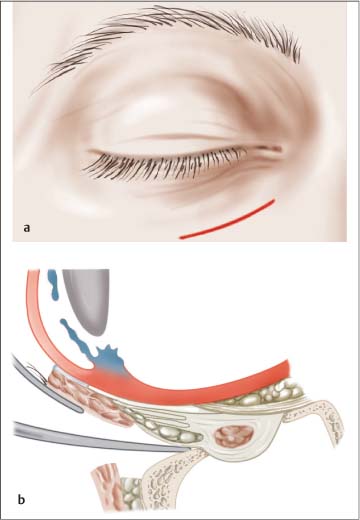
20 Treatment of Orbital Injuries Every fracture of the orbital floor with herniation of globe contents (fat, muscle) or displacement of bone fragments into the orbit demands surgical repair. The patient should undergo surgery as soon as possible following injury in order to avoid damage to fatty tissue (necrosis) or ocular muscles (scarring). If surgery within the first 24 hours is not possible, it is advisable to wait until swelling begins to subside. Various approaches to the orbit are used: Following exposure of the periosteum at the orbital rim, further exploration of the orbital floor proceeds subperiosteal, following incision of the periosteum, under visualization. The periosteum is undermined with a small periosteal elevator. The orbital contents are elevated with a dural elevator, without creating pressure on orbital contents or in the orbital apex. The fracture is exposed in its entirety and herniated orbital tissues are returned to their preinjury position. If there is entrapment of tissue (“trap door” mechanism) a small hook is used to elevate the “trap door.” A number of different materials are available for reconstruction of the orbital floor. Small defects can be closed with porous polydioxanone (PDS) sheeting. For larger defects (3 cm2) or comminuted fractures, autogenous grafts (cartilage, bone) should be used. These may require fixation to the orbital rim with osteosynthetic techniques. The graft must be exactly adapted to the defect, as it will otherwise later be visible and palpable over the orbital margin (Fig. 20.4). Packing of the maxillary sinus (packing, balloons, plugs) should be avoided, as it causes damage to the mucosa and cannot offer adequate stabilization of the orbital floor for the duration of healing. In rare cases, blindness can occur following orbital reconstruction. Causes may be hematoma and edema of orbital contents. It is essential that routine postoperative vision testing is conducted. Any deterioration in vision demands prompt orbital decompression. Persistent diplopia, which is not caused by scar fixation (traction test), is usually caused by nerve injury or injury to muscle tissue. Fig. 20.1 Transconjunctival incision with lateral canthotomy (modified from Kellman and Marentette 1995). a Illustration of the incision. b Dissection in front of the orbital septum and subperiosteal. c Elevation of orbital contents with a dural elevator. Fig. 20.2 Subciliary incision (modified from Kellman and Marentette 1995). a Incision just below the lid margin. Exposure of the orbicularis oculi muscle. b After transecting the muscle, dissection along the orbital septum to the periosteum; after incision, further dissection continues subperiosteal. c Overview of the preparation in the horizontal plane—after trans-section of the muscle, the preparation follows the lid spetum until it reaches the periosteum of the zygoma which is tunnelled after transsection. Fig. 20.3 Infraorbital incision (modified from Kellman and Marentette 1995). a Incision placed in a skin crease. b After dissection of the muscle, locating the orbital margin and periosteal incision. Insufficient support of orbital contents due to inadequate grafting material, insufficient fixation of the graft, or incomplete return of orbital contents to their anatomic position, leads to enophthalmos, sometimes with diplopia. In such situations, orbital reconstruction must be repeated using autogenous (bone) grafting. Persistent lymphedema in the lower lid region is more commonly observed in infraorbital incisions if the incision extends too far to lateral. If dissection of skin layers is inexact in the subciliary incision, there is a risk of entropion, which must be treated with a free skin graft. Rules and Pitfalls
 Flowchart and Checklist Injuries of the Orbits, Chapter 3, p. 22.
Flowchart and Checklist Injuries of the Orbits, Chapter 3, p. 22.
 Antibiotic Therapy, Chapter 24, p. 210.
Antibiotic Therapy, Chapter 24, p. 210.
 Diagnosing Injuries of the Orbit, Chapter 10, p. 86.
Diagnosing Injuries of the Orbit, Chapter 10, p. 86.
Fractures of the Orbital Floor
Indications
Approaches
 Transconjunctival incision, lateral canthotomy: The lower lid is drawn to inferior using a lid hook or two traction sutures. After incising the conjunctiva beneath the tarsus, dissection continues in front of the orbital septum to the periosteum. Lateral canthotomy can be used to widen the approach, if necessary, incising the lateral canthus to the periosteum of the orbital rim. To close the wound, suturing the conjunctiva in the canthus is recommended. Attention should be paid to exact reconstruction of the lid margin (Fig. 20.1).
Transconjunctival incision, lateral canthotomy: The lower lid is drawn to inferior using a lid hook or two traction sutures. After incising the conjunctiva beneath the tarsus, dissection continues in front of the orbital septum to the periosteum. Lateral canthotomy can be used to widen the approach, if necessary, incising the lateral canthus to the periosteum of the orbital rim. To close the wound, suturing the conjunctiva in the canthus is recommended. Attention should be paid to exact reconstruction of the lid margin (Fig. 20.1).
 Subciliary incision: The incision begins just lateral to the lacrimal punctum and continues 2 mm below the eyelashes within the existing skin creases. To create a skin-muscle flap, the skin and the pretarsal portion of the orbicularis oculi muscle are incised. The incision then runs along the orbital septum to the periosteum of the orbital rim. Wound closure is in layers (Fig. 20.2).
Subciliary incision: The incision begins just lateral to the lacrimal punctum and continues 2 mm below the eyelashes within the existing skin creases. To create a skin-muscle flap, the skin and the pretarsal portion of the orbicularis oculi muscle are incised. The incision then runs along the orbital septum to the periosteum of the orbital rim. Wound closure is in layers (Fig. 20.2).
 Infraorbital incision: The incision is placed in the lower lid crease and must continue diagonally to inferior lateral. After skin and muscle dissection, the orbital rim is exposed. Wound closure is in layers (Fig. 20.3).
Infraorbital incision: The incision is placed in the lower lid crease and must continue diagonally to inferior lateral. After skin and muscle dissection, the orbital rim is exposed. Wound closure is in layers (Fig. 20.3).
Surgical Technique
 Grafting and Osteosynthesis Materials, Chapter 25, p. 211.
Grafting and Osteosynthesis Materials, Chapter 25, p. 211.
Complications
 To prevent development of orbital hematoma, a fenestrated graft (PDS screen) should be used, allowing drainage of blood to the maxillary sinus.
To prevent development of orbital hematoma, a fenestrated graft (PDS screen) should be used, allowing drainage of blood to the maxillary sinus.
 To prevent the graft from shifting, a strap can be cut in the graft, and advanced beneath the anterior fracture margin.
To prevent the graft from shifting, a strap can be cut in the graft, and advanced beneath the anterior fracture margin.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree