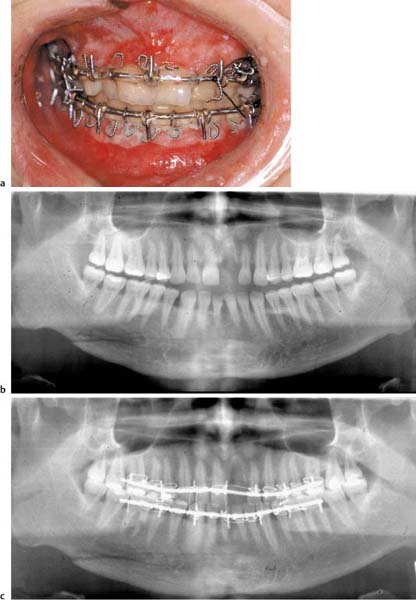
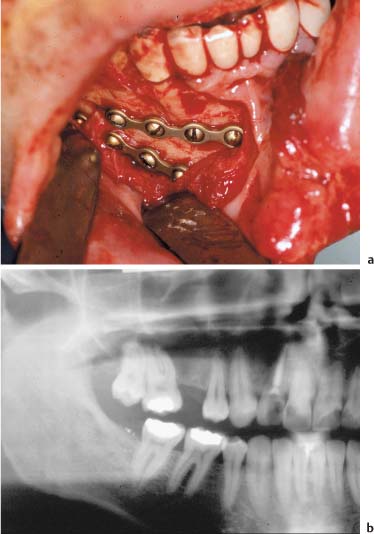
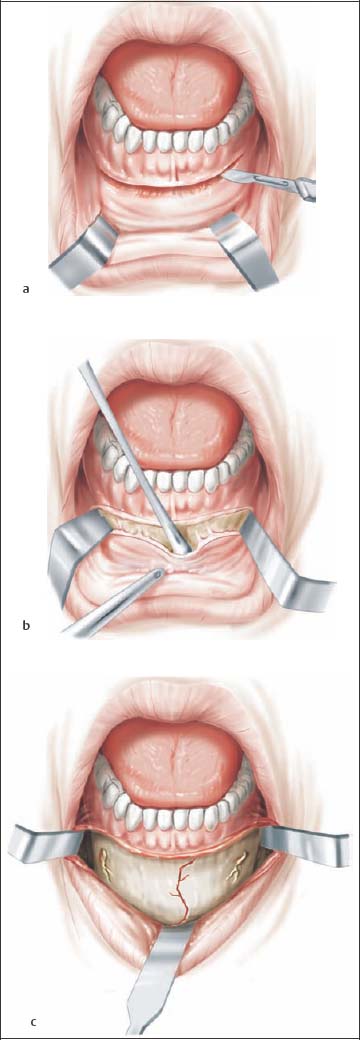
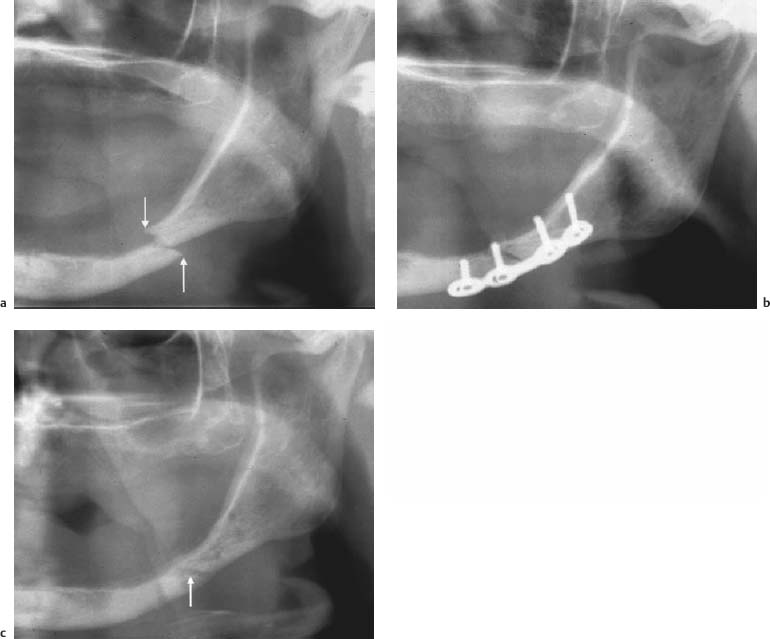
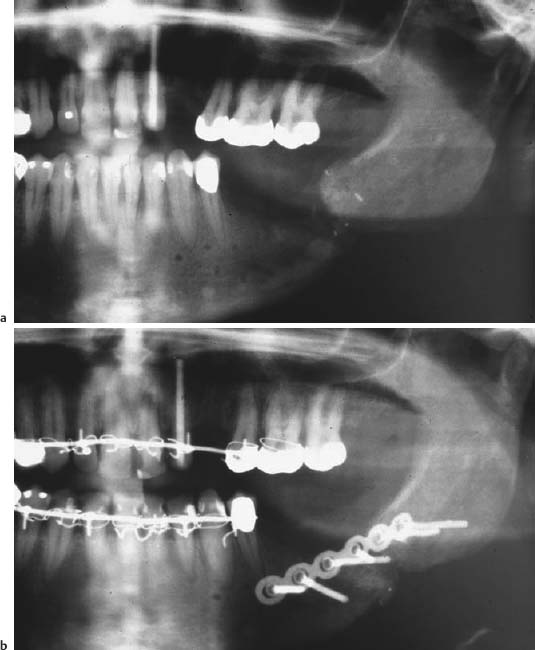
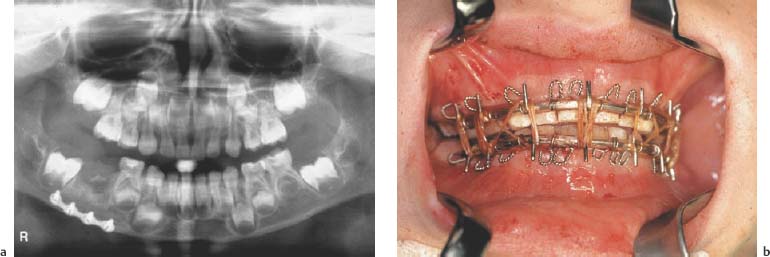
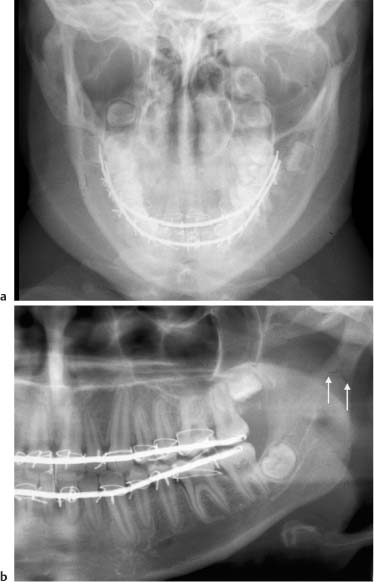
21 Treatment of Injuries of the Mandible Checklist Dental Injuries, Chapter 3, p. 24. Fractures with dentoalveolar involvement are considered open fractures as—even in nondisplaced fractures—there is communication between the oral cavity and mandibular marrow space through the periodontal pockets around the affected teeth. This is especially true of fractures of the mandibular angle: here the fracture line typically travels through the periodontal pocket of the distal root of the last molar, continuing through the socket of the frequently unerupted wisdom tooth. In edentulous portions of the mandible, there are often also lacerations of the mucosa firmly attached to the bone (attached gingiva). Management of these fractures must therefore occur expeditiously, in order to minimize the risk of infection in the fracture gap. Nondisplaced fractures of the mandibular body can be conservatively managed. Following splinting of the upper and lower jaws, intermaxillary wiring (immobilization) for 4–6 weeks is necessary. During this time, the patient is on a liquid diet. Perimandibular circumferential wiring is still used in conservative management of fractures involving primary or deciduous teeth and also for adaptation of splinting in the partially or fully edentulous jaw (Fig. 21.1). Fractures of the mandible including the angle and ramus of mandible to the height of the mandibular foramen are managed using osteosynthesis techniques. The technique of choice is the placement of miniplates, which are fixed using monocortical screws to prevent injury to the roots of the teeth and inferior alveolar nerve. In isolated instances, compression plating (for infected fractures) is used. Fixation is with bicortical screws placed so as to avoid damaging the roots of the teeth or inferior alveolar nerve. An intraoral approach is used to access the fracture. Correct occlusion must be established for surgery. To do so, the upper and lower jaws are splinted and intermaxillary immobilization is placed during the operation. Teeth in the line of fracture can impede fragment realignment or even render it impossible, and they can cause infection at the fracture gap. The indication for retaining teeth in the line of fracture is thus very narrowly assessed. Simple mandibular fractures can be managed with the patient under local anesthesia. Treatment under intubation anesthesia is generally the preferred method. For restoration of occlusion, endonasal or submandibular intubation is necessary. As a general rule, an intraoral approach is used for surgical access to the mandibular body and ramus to the height of the semilunar notch. After injection of a vasoconstrictor for intraoperative hemostasis (local anesthesia with epinephrine 1:100 000), the oral vestibule is opened using suitable retractors. The mucosal incision is made in the mobile mucosa about 5 mm caudal to the border of the “attached gingiva.” The periosteum is incised some 2 mm further to cranial. Alternatively, a gingival margin incision can be used. The periosteum is then stripped to the inferior margin of the mandible, exposing the fracture. The utmost care must be taken to preserve the mental nerve (Fig. 21.2). After fracture fragments are brought into exact realignment with the jaws in proper occlusion, the fracture is stabilized by means of osteosynthesis techniques, for which the fracture line must be checked all the way to the basal arch of the mandible. Fig. 21.1 Conservative management of a slightly displaced atypical comminuted mandibular fracture with splinting and intermaxillary immobilization. a Clinical picture after splinting and intermaxillary immobilization. b Orthopantomogram prior to treatment. c After splinting and intermaxillary immobilization. Fractures involving the symphyseal region are stabilized using two four-hole or six-hole miniplates. One miniplate is placed just caudal to the root tips of the frontal incisors or canines, and the other further to caudal 5 mm cranial to the mandibular margin. Selecting the correct screw length (7 mm) can ensure that damage to the roots of the teeth is avoided. Fractures in the premolar region, and in particular, fractures traversing the mental foramen, can often be adequately stabilized using a six-hole miniplate. Two miniplates may occasionally be necessary. The cranially positioned plate should be placed between the foramen and the root tips of the premolars and the second plate caudal to the foramen (Fig. 21.3). Fractures in the molar and mandibular angle regions can be sufficiently stabilized using a six-hole miniplate. The plate is placed on the sturdy oblique line and thus can absorb tensile forces; compressive forces are transmitted through the bone. Placing a second plate further to caudal is therefore not permitted for repair in this region, as it would impede transmission of compressive forces through the bone (Fig. 21.4). Fig. 21.3 Placement of four-hole miniplates for osteosynthesis in an oblique mandibular fracture in the right canine tooth region. a Clinical picture. b Orthopantomogram. Compression plates, on the other hand, are placed caudal to the root tips and inferior alveolar nerve, often serving as tension bands with fixation at the alveolar process. Tension banding can be achieved by splinting or with a miniplate placed to cranial (Fig. 21.5). After the screws have been securely tightened and intermaxillary fixation released, fragment position and occlusion must be checked. The intervention is concluded with placement of a Redon suction drain and suturing of the mucosa and periosteum using suture materials that are impermeable to oral fluids. Fig. 21.2 Vestibular incision (modified from Kellman and Marentette 1995). a Incision slightly towards buccal from the vestibule. Alternatively, a gingival margin incision can be used. b Subperiosteal dissection of the mandible. c Exposure and preservation of both mental nerves. Incising the periosteum over the nerve makes exposure easier. Fig. 21.4 Fracture of the right mandibular angle. a Proper fragment position after placing a six-hole miniplate. b Properly healed fracture after removing osteosynthesis materials. Fig. 21.5 Plate osteosynthesis of an infected fracture of the right mandibular angle using a compression plate on the basal margin of the mandible and a miniplate on the temporal crest (tension banding). Rules and Pitfalls Procedures do not diverge considerably from those used in treating the dentulous jaw. The indication for surgery, however, is usually more generous. Nondisplaced fractures of the mandibular ramus can be treated conservatively with splinting of the upper and lower jaws and intermaxillary fixation for a period of 4– 6 weeks. Surgical management of displaced mandibular ramus fractures has advantages, as it offers the only means of correct fragment positioning. Access is intraoral. The mucosal incision is placed over the anterior margin of the mandibular ramus and is carried from there into the oral vestibule. The fracture can be exposed after freeing the periosteum from the mandible. The upper and lower jaws are splinted and intermaxillary immobilization is established. After exposing the fracture, it is reduced and stabilized using miniplates with the jaws in proper occlusion and fragments correctly positioned. Wound drainage is with a Redon drain. The wound is closed using suture materials that are impermeable to oral fluids. Rules and Pitfalls Dentition and, in particular, secured occlusion, have an important stabilizing influence on fragments in the healing of mandibular fractures. The edentulous mandible is frequently atrophied and occasionally no thicker than a pencil. Cancellous bone is lacking and the bone is sclerotic and poorly vascularized. Surface contact areas are small in the fracture region. Protracted fracture healing and an increased rate of complications (osteitis of the fracture gap, pseudarthrosis) are therefore to be expected. Without exception, fractures of the edentulous or inadequately dentate jaw must thus be managed with miniplates or compression plates. In the extremely atrophied jaw, compression plating is the superior technique, despite low bone mass. An extraoral approach is preferred in such situations. To preserve the nourishing periosteal vascular system, epiperiosteal dissection and plate placement is an option, if necessary, in conjunction with modified dot-like plates. Only in exceptional situations should extensive intervention, such as autogenous bone grafting or micro-vascular tissue transfer of pedicled fibular flaps, be performed in the mostly elderly patients with multiple morbidity (Fig. 21.6). Because of the high rate of complications and the often unsatisfactory treatment result, conservative treatment with denture splinting and intermaxillary immobilization is only infrequently used in the atrophied, edentulous mandible. Fig. 21.6 Osteosynthesis in a mandibular fracture of an atrophied jaw. a Fracture in the left molar region (arrows). b Stabilization with a four-hole compression plate from extraoral—correct fragment position. c Twelve months post trauma and after removing osteosynthesis materials—normal knitting together of bones at the fracture gap. In mandibular defect fractures (missile wound), one must consider whether: Traditional methods of immobilizing contaminated mandibular fractures include mandibulomaxillary wiring (following splinting of the upper and lower jaws) and external fixation. More recent studies have shown that, if certain stabilization is successful, the presence of foreign materials (plates and screws) does not impair resolution of infections or healing of infected fractures. If infection occurs after fracture stabilization, plates and screws should only be removed if they have loosened. If plate stabilization is certain, the infection can be treated with incision, drainage, and antibiotic therapy (Fig. 21.7). Fig. 21.7 Mandibular defect fractures. a Mandibular defect fracture after osteomyelitis at the fracture gap. b Fracture management with splinting, intermaxillary immobilization, autogenous cancellous bone grafting from the iliac crest, and compression plating. An infected, untreated fracture should be viewed as a defect fracture and stabilized using a rigid plate (compression plate). In some situations, immediate bone grafting is indicated. It is imperative that the screws fixing the plates are inserted into healthy bone and not in tissue with inflammatory changes. Compression plating is in such circumstances preferable to miniplating. Mandibular fractures in patients with primary or deciduous teeth are generally treated conservatively to avoid injury to the tooth germs and influencing growth. However, multiple fractures with joint involvement, widely displaced or wide-open fractures, and comminuted fractures are increasingly seen as indications for operative management using miniplates as they allow early initiation of functional therapy. In these situations, miniplates are atypically applied to the mandibular margin to avoid damaging the tooth germs (Fig. 21.8). Fig. 21.8 Pediatric mandibular fracture. a Osteosynthesis of a mandibular fracture in a child. The four-hole miniplate was placed with short screws (5 mm) on the basilar arch to avoid damage to the tooth germs with certainty. b Splinting of upper and lower jaws in conservative management of a pediatric mandibular body fracture. All fractures of the mandibular neck or condyle require management. The goal of treatment is undisturbed joint functioning and healing of bones in proper fragment position. Posttraumatic displacement caused by muscular pulling forces or mouth opening movements should be prevented. Immobilization of the mandible and the temporomandibular joint in particular, eases pain and accelerates subsidence of swelling. Treatment can be conservative, surgical, or functional. Often, a combination of treatment approaches is advisable. If various courses of treatment are possible, the patient must be thoroughly informed of the advantages and disadvantages of each procedure. Splinting and intermaxillary immobilization are considered the treatment modalities of choice. In patients with mostly dentate jaws and intact buttress zones, the upper and lower jaws should be splinted and then intermaxillary immobilization with proper occlusion established (Fig. 21.9). To relieve the joint, a thin occlusal splint (hypomochlion) can be placed between the last molars for 5–7 days. In joint fractures at lower or middle heights, intermaxillary immobilization is maintained for 3–4 weeks. For fractures of the condylar head, immobilization is for only 8–10 days. Follow-up functional therapy is essential for the prevention of ankylosis. In jaws with missing molars, it should be checked whether the patient’s dentures or other occlusal devices can provide distal support. After intermaxillary immobilization is released, continuous functional follow-up care (physiotherapy, myofunctional exercises, wooden tongue blade, corkscrew appliance) is essential for restoring mandibular mobility. If the patient rejects or cannot tolerate intermaxillary immobilization, and if pure functional treatment appears inadequate, surgical management should be considered for the treatment of nondisplaced fractures of the condylar process. It can occasionally be considered for edentulous patients as well. For concomitant fractures of the facial skeleton, surgery allows early mobilization of the mandible. Operative management of fractures of the condylar process is, as a general rule, performed under intubation anesthesia. Endonasal or submandibular intubation is necessary, as osteosynthesis plating with the jaws in proper occlusion is generally performed with securely wired dental arches. Tracheotomy is not necessary. Fig. 21.9 Conservative management of a (bilateral) nondisplaced condylar process fracture with splinting and intermaxillary immobilization. Radiographs in two planes (A, B). The mucosal incision is placed at the temporal crest and is carried from there into the oral vestibule. The mucosa and periosteum are incised. After exposing the mandible to the temporomandibular joint, freeing the masseter muscle, identifying the semilunar notch, and freeing the temporalis muscle attachment from the coronoid process, the fracture of the condylar process is exposed. The periosteum should be stripped from the bone about 1– 2 cm proximal to the fracture for placing the plates. Care must be taken to avoid displacement of the fracture during dissection. Miniplates, in particular, are used for osteosynthesis. Lag screws can also be used for markedly oblique fractures. After placement of the plates, occlusion is checked. Muscle relaxants are administered for assessing occlusion. The intervention is concluded with placement of a Redon suction drain and suturing of the mucosa and periosteum with suture materials that are impermeable to oral fluids (Fig. 21.10). As the intraoral approach offers only limited visualization, realignment of small fragments is exceedingly difficult, and exact evaluation of fragment position is only possible using endoscopy, at best. Holes are drilled and the screws are inserted from transbuccal or intraorally using an angulated screwdriver. This approach cannot be unequivocally endorsed for surgeons with less experience in using this particular technique. Rules and Pitfalls
 Flowchart and Checklist Injuries of the Facial Skeleton, Chapter 3, p. 20.
Flowchart and Checklist Injuries of the Facial Skeleton, Chapter 3, p. 20.
 Antibiotic Therapy, Chapter 24, p. 210.
Antibiotic Therapy, Chapter 24, p. 210.
 Diagnosing Injuries of the Mandible, Chapter 11, p. 96.
Diagnosing Injuries of the Mandible, Chapter 11, p. 96.
Fractures of the Mandibular Body with Dentoalveolar Involvement
Indications
Conservative Management
Surgical Management
Approaches
Surgical Technique
Complications
 Injury to the mental nerve;
Injury to the mental nerve;
 Injury to the inferior alveolar nerve in the bony canal;
Injury to the inferior alveolar nerve in the bony canal;
 Hemorrhage in the floor of the mouth from vascular injury;
Hemorrhage in the floor of the mouth from vascular injury;
 Injury to the roots of the teeth;
Injury to the roots of the teeth;
 Unstable osteosynthesis;
Unstable osteosynthesis;
 Soft tissue trauma from hook traction;
Soft tissue trauma from hook traction;
 Hematomas from insufficient drainage increase the risk of wound infection.
Hematomas from insufficient drainage increase the risk of wound infection.
 The mental nerve can be preserved by mobilization after carefully slitting the periosteum.
The mental nerve can be preserved by mobilization after carefully slitting the periosteum.
 Submandibular intubation avoids tracheotomy in simultaneous nasal surgery.
Submandibular intubation avoids tracheotomy in simultaneous nasal surgery.
Fractures of the Mandible without Dentoalveolar Involvement or in the Partially Edentulous Jaw
 Diagnosing Injuries of the Mandible, Chapter 11, p. 96.
Diagnosing Injuries of the Mandible, Chapter 11, p. 96.
Fractures of the Mandibular Ramus
Conservative Treatment
Surgical Treatment
Approaches
Surgical Technique
Complications
 Inadequate drainage can result in postoperative hematomas or infections.
Inadequate drainage can result in postoperative hematomas or infections.
 Fracture reduction is difficult because the narrow surgical approach often fails to provide depth perception in the fracture gap region.
Fracture reduction is difficult because the narrow surgical approach often fails to provide depth perception in the fracture gap region.
 Visualization of the operative field can be improved by using endoscopic techniques and instrumentation utilized in surgery for dysgnathia.
Visualization of the operative field can be improved by using endoscopic techniques and instrumentation utilized in surgery for dysgnathia.
Fractures in the Edentulous, Atrophied Mandible
Mandibular Defect Fractures
 primary reconstruction of the mandible should be with autogenous, possibly microvascular pedicled bone transfer, bone/muscle, or bone/muscle/skin grafting (fibula, scapula, iliac crest) or;
primary reconstruction of the mandible should be with autogenous, possibly microvascular pedicled bone transfer, bone/muscle, or bone/muscle/skin grafting (fibula, scapula, iliac crest) or;
 whether the mandibular stumps should be stabilized initially using a reconstruction plate for bridging mandibular defects so as to avoid irreversible warping and atrophy of soft tissues caused by scarring.
whether the mandibular stumps should be stabilized initially using a reconstruction plate for bridging mandibular defects so as to avoid irreversible warping and atrophy of soft tissues caused by scarring.
Contaminated Mandibular Fractures
Fractures of the Mandible in Patients with Primary or Deciduous Teeth
Nondisplaced Fractures of the Condylar Neck and Head
 Diagnosing Injuries of the Mandible, Injuries of the Condylar Process, p. 108.
Diagnosing Injuries of the Mandible, Injuries of the Condylar Process, p. 108.
Indications
Conservative Treatment
Surgical Treatment
Approaches—Intraoral Approach
Surgical Technique
Complications
 Intraoperative fracture displacement;
Intraoperative fracture displacement;
 Hematoma if drainage is insufficient;
Hematoma if drainage is insufficient;
 Suture dehiscence and wound contamination;
Suture dehiscence and wound contamination;
 Malocclusion with even minimal fracture displacement;
Malocclusion with even minimal fracture displacement;
 Injury to the inferior alveolar nerve;
Injury to the inferior alveolar nerve;
 Injury to the facial nerve from hook traction or transbuccal screw insertion;
Injury to the facial nerve from hook traction or transbuccal screw insertion;
 Salivary fistulae with transbuccal screw insertion.
Salivary fistulae with transbuccal screw insertion.
 Ramus hooks for exposing the coronoid process;
Ramus hooks for exposing the coronoid process;
 Hooks with integrated cold light source, arthroscope, 30° Hopkins lens;
Hooks with integrated cold light source, arthroscope, 30° Hopkins lens;
 Administer muscle relaxant;
Administer muscle relaxant;
 Use of endoscopy or operation microscope to improve visualization.
Use of endoscopy or operation microscope to improve visualization.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree