Total Parotidectomy
David W. Eisele
INTRODUCTION
Total parotidectomy describes removal of the entire parotid gland. From a practical standpoint, total parotidectomy is a difficult operation as removal of all parotid tissue with facial nerve preservation is challenging. The benefits of complete removal of all parotid tissue must be weighed against potential morbidity. Total parotidectomy is described. Less extensive resection of the gland may be appropriate based on tumor extent, type, and location.
HISTORY
A thorough history is obtained prior to consideration for surgery. Most patients with parotid neoplasms note a progressively enlarging asymptomatic mass. Pain can be associated with some neoplasms but is not a reliable indicator of malignancy. Symptoms of sensory loss, trismus, and facial weakness are worrisome for local invasion by a malignant neoplasm. A past medical history should include information regarding any prior cutaneous lesions or malignancies. In addition, the patient should be queried about any prior radiation exposure to the head and neck including multiple dental radiographs. Smoking is associated with Wharthins tumor and, therefore, should be investigated.
PHYSICAL EXAMINATION
All patients should have a complete examination of the head and neck. Cranial nerve function should be examined, and facial nerve function should be evaluated carefully. Facial weakness may be subtle, or facial muscle fasciculation may be noted. Facial nerve paralysis is usually an indication of nerve invasion by a malignant tumor. Fixation to the skin, decreased mobility, and associated cervical lymphadenopathy are other signs consistent with malignancy.
INDICATIONS
The most common indications for this operative procedure are a malignant neoplasm involving the entire parotid gland, metastases to parotid lymph nodes, recurrent multifocal neoplasm, and chronic parotid sialadenitis refractory to medical and sialendoscopic management.
CONTRAINDICATIONS
Total parotidectomy is a major operation. Significant medical comorbidities, limited life expectancy, bleeding disorders, and anticoagulated states represent contraindications.
PREOPERATIVE PLANNING
Fine Needle Aspiration Biopsy
Fine needle aspiration (FNA) biopsy is an accurate and useful investigation for the diagnosis of a parotid mass. FNA allows for improved patient selection for surgery since it can identify conditions such as reactive lymph nodes or cysts that might clinically mimic parotid neoplasms. The information gained by FNA is useful for patient counseling, surgical timing and planning, and guidance of preoperative consultations.
Imaging Studies
Imaging studies are helpful to assess malignant neoplasms or neoplasms that are large, have diminished mobility, or have suspected local invasion or deep extension. In general, magnetic resonance imaging is the preferred imaging study for parotid neoplasms.
SURGICAL TECHNIQUE
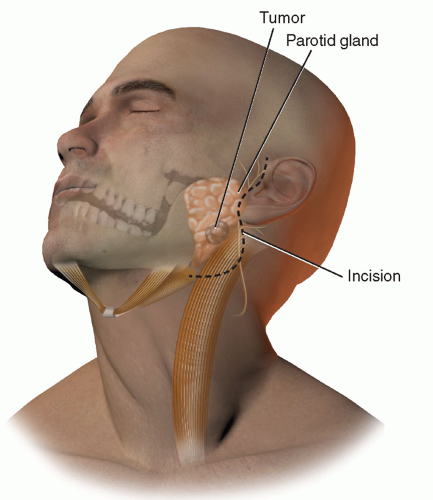
Total parotidectomy is performed under general anesthesia. Long-term paralytic agents are avoided to allow for facial nerve monitoring and stimulation. After the induction of general anesthesia, the endotracheal tube is positioned in the contralateral oral cavity and secured by tape only on the contralateral face. A modified Blair incision is planned in a preauricular crease coursing around the ear lobule and then into an upper neck crease (Fig. 27.1). The ipsilateral face is prepared with an antiseptic solution, and nerve electrodes are placed in the ipsilateral facial muscles if intraoperative electrophysiologic facial nerve monitoring is planned. The surgical field is then draped with a transparent adhesive sterile drape to allow intraoperative visualization of facial motion and maintenance of a sterile operative field.
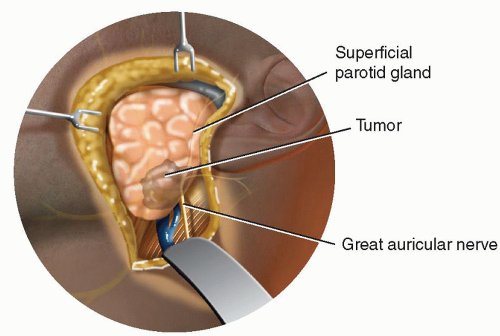
The skin incision is made with a scalpel and carried down through the subcutaneous tissues and platysma muscle inferiorly. Care is taken to avoid division of the greater auricular nerve. An anterior flap is elevated superficial to the greater auricular nerve and the parotid fascia (Fig. 27.2). Elevation of a thick flap is desirable to reduce the occurrence of Frey syndrome. As the flap is elevated toward the anterior aspect of the gland, the peripheral facial nerve branches are carefully avoided. A posterior-inferior flap is also elevated to expose the tail of the parotid gland. After elevation, the flaps are retracted with silk sutures or self-retaining hooks. The flaps are kept moist during the procedure to prevent tissue desiccation.
The tail of the parotid gland is dissected from the sternocleidomastoid muscle by dissecting deep to the posterior branch of the greater auricular nerve, if preservation of this nerve is feasible based on tumor location. Next, the posterior belly of the digastric muscle is exposed with further elevation of the tail of the parotid gland. During elevation of the tail of the parotid, the posterior facial vein is divided and ligated with silk ligatures.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree