Topographic Anatomy of the Eye: An Overview
D. J. John Park
James W. Karesh
Topography is the study of the gross surface relationships between different aspects of the surface of a structure or between various objects related to that structure. The globe is a highly complex object in terms of its own three-dimensional shape and because of the number of other anatomic elements contained within it and surrounding it. In addition, a number of vascular and neural structures pass into and out of the globe, further complicating its topography. However, to adequately understand the globe as an organ of vision, it is first essential to understand its structure and the complex interrelationships that exist between its internal organization and the external elements surrounding it. A number of excellent texts have been written covering the various aspects of ocular anatomy and histology, and the reader is referred to them for more detailed descriptions of these subjects.1,2,3 Much of what is discussed in this overview can be found in these texts.
GENERAL DIMENSIONS AND TOPOGRAPHY OF THE GLOBE
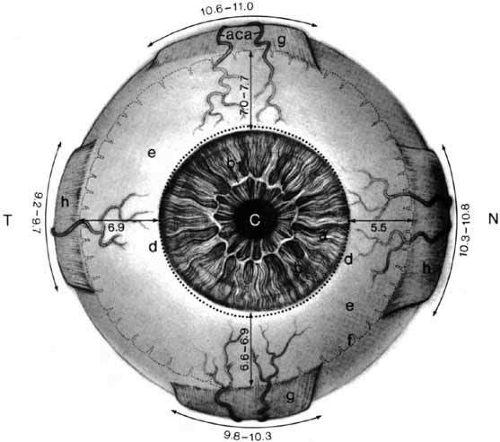
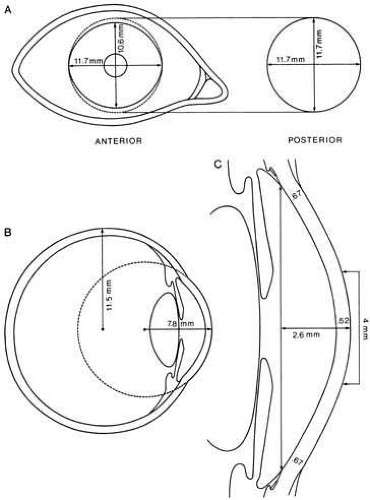
As a three-dimensional object, the globe approximates an irregular oblong spheroid that can be divided topographically into segments of two modified spheres of different radii of curvature. (Figs. 1, 2, and 3) The cornea constitutes the anterior segment, covers one-sixth of the surface area, and has a radius of curvature of approximately 8 mm. The larger posterior segment is composed of the scleral shell and has a radius of curvature of approximately 12 mm. This segment is not perfectly spherical because of the three following features: (1) the anterior portion is flatter and more weakly curved than the posterior portion;1 (2) the entire globe is slightly flattened from above so that its greatest vertical diameter is slightly less than its greatest horizontal diameter; and (3) the scleral bulges outward more temporally than nasally.
Anteriorly, the center of the external surface of the cornea is called the anterior pole. Because the vertical dimension of the cornea is less than the horizontal dimension, this pole is closer to the inferior and superior border of the cornea and farther away from its nasal and temporal border (Fig. 4). Posteriorly, the center of the external surface of the sclera is called the posterior pole. For practical purposes, this point is equidistant from any point along the limbus. The geometric (anatomic), visual, and optic axes describe the globe in the antero-posterior dimension. The geometric axis connects the anterior pole and the posterior pole and is the basis for topographical reference for the gross elements of the globe. When this axis is measured from the external surface of the cornea to the external surface of the sclera, it is referred to as the external axis, and when measured from the internal surface of the cornea to the anterior surface of the retina, it is called the internal axis. The visual axis represents a line drawn from the fovea centralis to the point of fixation passing through the nodal point. It passes slightly nasal to the corneal summit. The optic axis represents a line passing through the anterior pole, the center of the lens, and the nodal point. Whereas the visual and optic axes relate to the fovea, nodal point, and other aspects of visual function, the geometric axis is purely a contrived dimension that is quite variable between individuals.
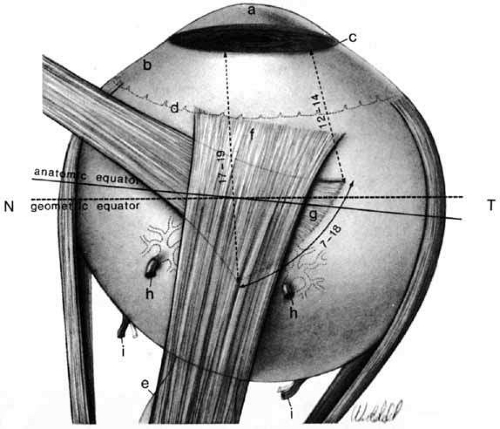
The anatomic equator and the geometric equator are different.1,2 The former represents a circumferential line on which every point is equidistant from the anterior and posterior poles. The latter is a simple circle whose diameter is perpendicular to the geometric axis and whose center is equidistant from the anterior and posterior poles. The anatomic equator divides the globe into two unequal halves, termed anterior and posterior hemispheres. If the globe were an ideal sphere, the anatomic equator would be a perfect circle in the coronal plane, perpendicular to the geometric axis, and thus coincident with the geometric equator. However, because the sclera bulges more temporally, the anatomic axis3 is farther posterior on its temporal side than on its nasal side. On average, the anatomic equator is approximately 13 to 14 mm behind the limbus. This is in contrast to what may be considered the functional equator for purposes of muscle surgery. This latter concept is based on the arc of contact the rectus muscles have with the globe, which is approximately 4 mm posterior to the anatomic equator on the temporal side and 4 mm anterior to it on the nasal side. A meridian is defined as a line encircling the globe in the antero-posterior direction, which passes the anterior and posterior pole and is perpendicular to the anatomic equator. There are two cardinal meridians for purposes of measuring the globe. The sagittal meridian divides the globe into nasal and temporal hemispheres and arbitrarily is based on the 6 o’clock and 12 o’clock positions on the limbus. The horizontal or transverse meridian is perpendicular to the sagittal meridian, being based on the 3 o’clock and 9 o’clock positions on the limbus and divides the globe into superior and inferior hemispheres.
The various dimensions of the globe have been extensively measured.1 These are generally fairly constant in the adult population and are relatively unrelated to either sex or race, usually varying by no more than 1 mm in various studies. However, in extreme degrees of axial hyperopia and myopia, the anteroposterior diameter of the globe may vary by as much as 3 mm from the normal measurement.4 The outer anteroposterior diameter of the globe averages 24.15 mm (range, 21.7–28.75 mm), whereas the internal anteroposterior diameter averages 22.12 mm.1 In high hypermetropia and myopia, the anteroposterior diameter can be as low as 20 mm and as high as 29 mm, respectively.4 The transverse diameter (diameter of the globe at the anatomic equator measured from the nasal to the temporal side) averages 23.48 mm, and the vertical diameter (diameter of the globe at the anatomic equator measured superiorly to inferiorly) averages 23.48 mm.1 The circumference of the globe at the anatomic equator averages 74.91 mm.1 At birth, the globe is more spherical than the adult globe and has an anteroposterior diameter approximately two-thirds that of the adult globe (16–17mm).5 By 3 years of age, this increases to within 1 mm of the average adult size (22.5–23 mm), reaching the normal adult size by approximately 13 years of age.5 When fully developed, the globe weighs approximately 7.14 to 7.5 g,2,6,7 has a volume of approximately 6.5 to 7.2 mL,7 and has a surface area of approximately 22.86 cm2.8
As already noted, the globe is asymmetric. This is demonstrated by the tilt of the anatomic equator, the more anterior placement of the nasal vortex veins compared with the temporal ones, and the more anterior placement of the medial rectus muscle insertion compared with the lateral rectus muscle insertion. Likewise, the optic nerve is positioned 3 mm nasal and 1 mm inferior to the posterior pole. In addition, the lens and pupil are slightly displaced nasally, with the anterior chamber angle being narrower nasally than it is temporally. The ciliary body is 1 mm in the anteroposterior dimension nasally than temporally. In contrast, the temporal retina is positioned approximately 1 mm farther anteriorly than the nasal retina.
RELATIONSHIP OF THE GLOBE TO THE BONY ORBIT
The globe is positioned in the anterior portion of the orbit and constitutes approximately 20% of the entire volume of the orbit. It is slightly closer to the lateral orbital wall than the medial wall and is nearer to the roof than the floor of the orbit. The posterior pole lies approximately 18 mm (14–24 mm)7 from the apex of the orbit. At its closest distance to the bony orbit the globe is approximately 4 mm from the roof, 4.5 mm from the lateral wall, 6.5 mm from the medial wall, and 6.8 mm from the floor.3 The lateral orbital rim is considerably recessed posteriorly compared to the medial orbit, which continues anteriorly to end at the nasal bridge. This leaves approximately one half of the globe exposed laterally, such that a line connecting the lateral orbital rim to the anterior lacrimal crest would pass well behind the ora seratta temporally and near the junction of the ciliary body and iris nasally. Thus the globe is most vulnerable to trauma on its lateral side, and surgical approach is easier here. In contrast, the anterior pole of the globe lies just posterior to a line drawn from the superior orbital rim to the inferior orbital rim and can vary from 12 mm anterior to 10 mm posterior to this line in healthy individuals. The prominence of the globes is dependent on orbital volume, globe size, orbital fat volume, and structure of the eyelids and conjunctiva, all of which vary between individuals and shows significant differences between ethnicities. Based on a study of 681 individuals with no history of orbital or endocrine disease, high myopia, or buphthalmos, Migliori and Gladstone found that white men had a mean protrusion value measured from the lateral orbital rim of 16.5 mm compared to 18.5 mm in black men, and 15.4 mm in white women compared to 17.8 mm in black women.9
The geometric axis of the globe is parallel to the medial orbital wall and is at a 45-degree angle to the lateral orbital wall. Thus divergent axis of each orbit is approximately 23 degrees. The two lateral walls of both orbits form a 90-degree angle.10 The distance between the geometric axes of the globes, or the interpupillary distance, is 58 to 60 mm.
SURFACE ANATOMY OF THE GLOBE AND THE SCLERA
The sclera forms five-sixths of the outer tunic of the eye, consists of dense fibrous tissue, and contains openings and canals for the various vessels and nerves entering and exiting the globe (Figs. 1, 2, and 3). Its mechanical properties and limited distensibility help contain the intraocular pressure and prevent deformations of the globe during extraocular movement. It is relatively avascular and principally composed of collagen with scant fibrocytes and ground substance. Externally it is white, whereas internally it is slightly brown because of the presence of pigmented melanocytes. This most interior layer of the sclera, adjacent to the uvea, is called the lamina fusca, whereas the most exterior layer of the sclera, consisting of delicate fibrous and elastic tissue connecting the bulbar fascia and the sclera, is called the episcleral tissue. If the sclera is thin, as in childhood, or its hydration content decreases to less than 40% or increases to more than 80%, the sclera becomes more lucent, such that it appears blue or slate grey. As the sclera thins, the underlying uvea absorbs more light and the scattering of shorter wavelength light by the scleral collagen imparts a blue hue.
The scleral thickness varies considerably in the anteroposterior dimension. It is thickest near the optic nerve, measuring 1 to 1.35 mm, and gradually thins anteriorly, where it measures 0.4 to 0.6 mm in thickness at the equator. The sclera is thinnest beneath the tendonous insertions of the extraocular muscles, where it measures approximately 0.3 mm in thickness.11,12 At the limbus (the transitional area between cornea and sclera), the sclera thickness is approximately 0.825 mm. In older individuals, it is unclear whether the apparently thinner sclera is caused by age-related atrophy13 or changes in scleral hydration.14
The anterior scleral foramen is defined by a zone in which the scleral fibers merge with the collagen fibrils of the corneal stroma. Usually the sclera is beveled internally to overlap the cornea anteriorly in the sagittal meridian, making the cornea appear as an ellipse. For this reason, the external diameter of the cornea averages 10.6 mm vertically and 11.6 mm horizontally.12 Internally, the anterior scleral foramen is more nearly circular, with a diameter of 11.6 mm. Both the external and internal margins of the sclera at the sclerocorneal junction extend slightly anteriorly, creating an external and internal annular groove, called the external and internal scleral sulcus, respectively. The external scleral sulcus is approximately 1 mm in depth. However, most of this is filled in by the attachments of the conjunctiva and Tenon’s fascia as they blend into the limbus, and thus is less apparent. The external scleral sulcus is more prominent nasally than temporally. The internal scleral sulcus is circular with an internal groove formed by the slight anterior projection of the sclera near the limbus. It is bound anteriorly by Schwalbe’s ring, posteriorly by the scleral spur, and contains Schlemm’s canal, externally, and the corneoscleral meshwork, internally. Along its inner surface, inserts the anterior tendons of the longitudinal ciliary muscles.15 The posterior margin of internal scleral sulcus extends anteriorly as the scleral spur and is the attachment for the ciliary muscle. At the base of the sulcus is Schlemm’s canal. A so-called pectinate ligament can occasionally be found to bridge the internal scleral sulcus.
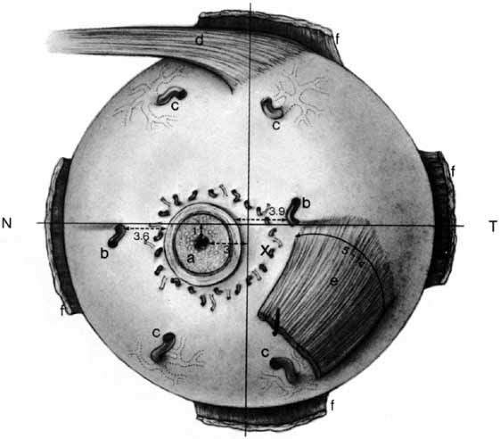
The posterior scleral foramen allows the ganglion cell axons to exit the globe and enter the orbital segment of the optic nerve. It is a short canal located 3 mm nasal to the vertical meridian and 1 mm inferior to the horizontal meridian in the posterior hemisphere. It has an internal diameter of 1.5 to 2.0 mm and an external diameter of 3.0 to 3.5 mm. It is approximately 0.7 mm long and exits the globe in a nasal direction at an oblique angle. The network of collagenous and elastic scleral fibers that traverse the foramen in the innermost one-third of the foramen is referred to as the lamina cribosa. It provides mechanical strength and anchorage points for the neural and vascular elements as they traverse the canal. The inner surface of the lamina cribosa is concave16 and is displaced posteriorly in the presence of sustained ocular hypertension. Fibroelastic fibers from the outer two-thirds of the sclera turn outward to merge with the dural sheath of the optic nerve.
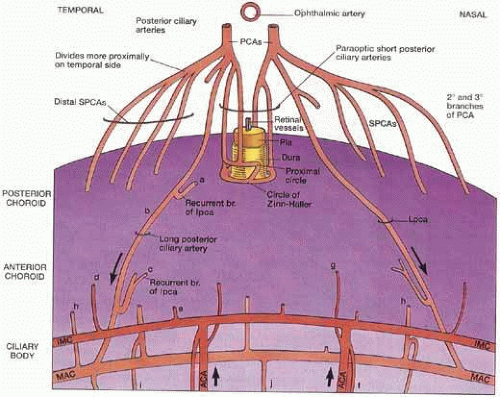
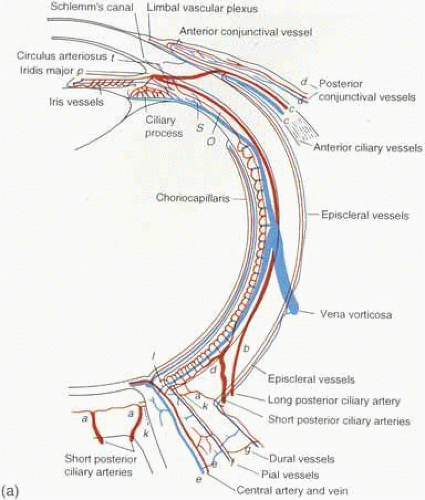
Emissary channels allow the passage of nerves and vessels through the scleral tunic. These can be divided into anterior, middle, and posterior emissary channels (Figs. 5, 6).
The anterior emissary channels are located near the limbus, through which the anterior ciliary arteries and veins and the ciliary nerves traverse. The anterior ciliary arteries travel with the rectus muscles, two in each muscle with the exception of the lateral rectus, which has one artery. Each artery enters the sclera just anterior to the insertions and travels obliquely to supply the ciliary body and feed the major arterial circle of the iris. Smaller branches turn externally toward the limbus, where they anastamose with subconjunctival vessels to form the episceral plexus. These recurrent branches of the limbal vessels supply the perilimbal conjunctiva within 3 to 6 mm of the limbus. The anterior ciliary veins leave the ciliary body and travel in a channel that is frequently shared with a branch of the posterior ciliary nerve, which passes close to the surface before looping into the ciliary body. This neurovascular loop is called the nerve loop of Axenfeld and is present in approximately 12% of individuals.17 Clinically, it appears as 1- to 2-mm dome-shaped gray area, that is often pigmented.
The middle emissary channels are located several millimeters posterior to the geometric equator and transmit the vortex veins. Their position can be somewhat variable. Temporally, these veins are closer to the sagittal meridian, and nasally they are farther away from this meridian. Internally, their position relative to the sclera varies from the equator to 6.36 mm posterior to the equator, with the most common position being 3 mm posterior to the equator.18,19 Externally, their exit position from the sclera varies from 13.75 to 25 mm posterior to the limbus. The superotemporal and superonasal veins exit more posteriorly (20.2 mm and 19.3 mm from the limbus, respectively) than the inferotemporal and inferonasal veins (17.4 mm and 18 mm from the limbus, respectively). The superotemporal vein exits the sclera approximately 8 mm, the superonasal vein 7 mm, the inferotemporal vein 5.5 mm, and the inferonasal vein 6 mm posterior to the equator. The distance each vein travels in the sclera is variable and ranges from 1.25 to 8.5 mm. When they exit the sclera, the vortex veins travel loosely between it and the bulbar fascia for 5 to 10 mm, with the superior temporal vein having the longest episcleral course.
On average, the choroid of each eye contains seven vortex veins (range, 5 to 8). They are more frequent nasally then temporally. In more than 50% of cases, the main trunks of these veins are incomplete, and they leave their scleral canals as branches. Usually only one vein is seen to exit the sclera in the superior temporal quadrant in contrast to the other quadrants where one or more veins may be found exiting. Generally, the veins tend to exit between the extraocular muscles and only rarely exit under the belly of a muscle.
The posterior emissary channels transmit up to 20 short posterior ciliary arteries and 10 short posterior ciliary nerves and two long posterior arteries and nerves. The short posterior ciliary arteries and nerves enter the sclera in an annular fashion around and within 1 to 2 mm of the optic nerve. These nerves and arteries are more closely approximated to the nerve medially than temporally. The two long posterior ciliary arteries and nerves pierce the sclera on either side of the optic nerve approximately along the horizontal meridian. The medial nerve and artery are approximately 3.6 mm from the medial aspect of the nerve sheath, whereas the temporal nerve and artery are approximately 3.9 mm from the temporal aspect of the nerve sheath and in close approximation to the posterior insertion of the inferior oblique muscle. They pass obliquely through the sclera for a distance of 3 to 7 mm. There may be additional long posterior ciliary arteries and nerves that insert into the posterior sclera, most commonly in the inferior aspect of the globe. The entrance of these additional vessels is usually more anterior than that of the vessels along the horizontal meridian.
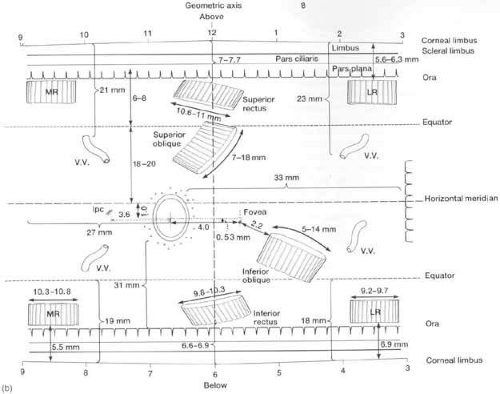
Both the insertions of the rectus and oblique muscles have specific topographical reference points that deserve considerable attention (Figs. 1, 2, 3, and 7). The tendons of the rectus muscles insert into the sclera and its fascial coverings at various distances from the limbus. The tendonous insertions of the medial and lateral rectus muscles are relatively linear, whereas those of the inferior and superior rectus muscles are somewhat curvilinear and obliquely placed so that their nasal insertion is closer to the limbus than their temporal insertion. The distance from the midpoint of the rectus muscle tendons to the limbus varies from study to study but generally is approximately 5.7 mm, 6.7 mm, 7.5 mm, and 7.9 mm for the medial, inferior, lateral, and superior rectus muscles, respectively (Table 1).2,18,20,21,22 This configuration describes the spiral of Tillaux. The distance between the insertions is approximately 7.4 mm between the medial and inferior rectus muscles, 8.5 mm between the inferior rectus and lateral rectus muscles, 7.2 mm between the lateral rectus and superior rectus muscles, and 8 mm between the superior rectus and medial rectus muscles.
TABLE 1. Measurements of the Tendinous Insertions of the Rectus Muscles | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||
The insertion of the superior oblique muscle is beneath the anterior portion of the superior rectus muscle. It has a wide curvilinear tendinous insertion that faces posterolaterally and is convex in that direction. The width of the insertion varies between 7 and 18 mm. The anterior and lateral edge of the tendon is just anterior to the geometric equator of the globe, approximately 12 to 14 mm (average, 13.8 mm)23 posterior to the limbus, only a few millimeters (3–4.5 mm)23 posterior to the lateral insertion of the superior rectus tendon, and close to the lateral edge of the superior rectus muscle. The majority of the tendon is posterior to the geometric equator. The medial and posterior edge of the tendon approximately 17 to 19 mm (average, 18.8 mm) posterior to the limbus and as much as 14 mm (average, 13.6 mm) posterior to the medial insertion of the superior rectus tendon. This edge of the tendon is approximately 8 mm superior to the posterior pole of the globe. The superolateral vortex vein is only a few millimeters posterior to the medial insertion of the superior oblique tendon and very close to the lateral edge of the superior rectus muscle.
The inferior oblique muscle has a very short or absent tendon at its insertion into the sclera. This insertion is inferior to the horizontal meridian and lateral to the sagittal meridian, placing it in the inferior lateral quadrant of the posterior aspect of the globe. The insertion is convex in the superior direction and measures 5 to 14 mm in length. At its most posterior point, the insertion is 3 to 6 mm lateral to the lateral aspect of the optic nerve and approximately 1 mm below and 1 to 3 mm (average, 2.2 mm) temporal to the macula.24 The most anterior aspect of its insertion is approximately 10 mm posterior to the midpoint of the lateral rectus muscle insertion. The posterior edge of the insertion and the muscle are only a few millimeters anterior to the inferolateral vortex vein.
THE CORNEA
The cornea is a tough transparent and avascular tissue that, along with the precorneal tear film, forms the major refracting surface for the eye and serves as a barrier between the environment and the inside of the eye (Fig. 4). The precorneal tear film ranges in thickness from 6 to 20 μm but averages approximately 7 μm.25 This tear film consists of an outer layer of lipid produced by the sebaceous glands of the eyelid and caruncle, a middle layer of aqueous fluid produced by the lacrimal and accessory lacrimal glands, and an inner layer of mucoprotein produced by conjunctival goblet cells. Anteriorly, the conjunctival surface of the eyelids is adjacent to and in contact with the tear film layer. During the course of blinking, this layer is distributed over the surface of the corneal epithelium continually rewetting and renewing the entire surface.
The external dimensions of the cornea are 11.6 to 12.6 mm horizontally and 10.6 to 11.7 mm vertically.12 These measurements are approximately 0.1 mm less in females. When viewed from the anterior surface, the cornea is oval because of a more prominent limbus superiorly and inferiorly.26 When viewed posteriorly, the cornea is circular and has a diameter of 11.6 mm. The thickness of the cornea varies from 0.51 to 0.56 mm centrally to 0.63 to 0.67 mm peripherally.27,28 An increasing number of studies have found that long-term use of contact lenses (hard and soft) is associated with decreased central corneal thickness.29,30,31,32,33,34 However, peripherally the thickness has been measured as high as 0.74 mm in normal individuals.1,12,35,36 Posteriorly, the corneal endothelium is bathed by the aqueous humor. The surface area of the cornea is approximately 1.3 cm3 or approximately one-fourteenth the area of the globe.12 The height of the cornea (i.e., the distance from a plane through the peripheral visible border of the cornea to the apex of the cornea externally) is 2.68 mm.1 The fresh cornea weighs 180 mg and has a specific gravity of approximately 1.05. Because the curvature of the cornea is greater than that of the scleral shell, a slight sulcus, the external scleral sulcus, marks the junction between the cornea and sclera. The radius of curvature of the anterior surface of the cornea ranges from 7.2 to 8.4 mm, and the radius of curvature of the posterior surface ranges from 6.2 to 6.8 mm in white men. The cornea is more curved in Asians than in whites and in women than in men. Although a wide variety of different corneal shapes can be seen between individuals, it is frequently more curved at the temporal cornea than the nasal cornea, and in the vertical plane than in the horizontal plane.37
The optical zone of the cornea is the central one-third, approximately 4 mm in diameter. The anterior and posterior surfaces of the cornea are relatively spherical in this region. However, they tend to diverge as they extend toward the periphery, where the cornea is slightly flattened. However, in individuals with some degree of corneal astigmatism the central optical zone may be somewhat ellipsoidal.
The size and shape of the cornea change throughout life. The size of the cornea in a newborn relative to the adult eye is fairly large, attaining adult size (1.3 cm2) between the ages of 1 and 2 years (Table 2).1 The most rapid period of corneal growth is in the first 6 months after birth. The newborn cornea is flatter than the adult cornea and is usually more curved in its periphery than centrally. On reaching adulthood, the average corneal radius decreases with age and the cornea becomes more spherical, thus contributing to the reduction of retinal image quality through the lifespan.38
TABLE 2. Comparison of the Newborn and Adult Cornea | |||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||
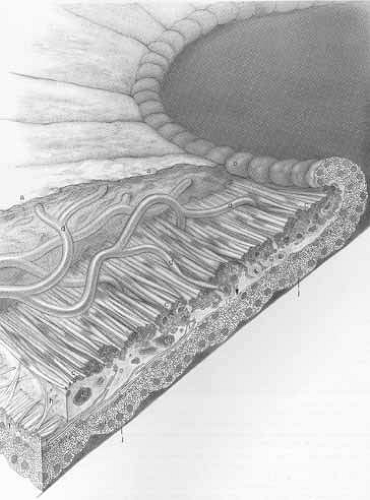
The cornea consists of five layers: (1) the epithelium; (2) Bowman’s layer; (3) stroma; (4) Descemet’s membrane; and (5) endothelium. The epithelium, which makes up approximately 10% of the total corneal thickness and measures approximately 50 to 60 μm, is a stratified, nonkeratinized, nonsecretory squamous epithelium that is 5 to 7 cells in thickness centrally, increasing at the limbus to 15 cells and to more than 20 cells in the conjunctiva. The epithelial layer consists of three distinct cellular types: a single layer of cuboidal basal cells, an intermediate layer of polygonal cells (also referred to as wing cells) that is 2 to 3 cells in thickness, and a superficial layer of flattened epithelial cells that is 3 to 4 cells in thickness. The basal layer consists of columnar cells that are quite regular in shape and size, measuring 18 μm in height by 10 μm in width. As basal cells divide, daughter cells move toward the surface of the cornea and differentiate into polygonal cells, forming the intermediate layer of the epithelium. The cells of the superficial layer are terminally differentiated squamous cells that measure 45 μm in length by 4 μm in height. Basal cells are adherent to its basement membrane, which is 48-nm-thick and is separated from these cells by a layer of granular material that is 23-nm-thick. At the limbus it becomes considerably thicker, forming the basal layer of the conjunctival epithelium. The basement membrane is strongly attached to the underlying Bowman’s layer.39
Bowman’s layer, which consists of interwoven collagen fibrils, is 8 to 14 μm in thickness, with the peripheral one-third being slightly thicker than the central two-thirds. Peripherally, the collagen fibrils of Bowman’s layer become more loosely arranged and end abruptly at the limbus. The deep surface of Bowman’s layer merges into the corneal stroma.
The corneal stroma measures 500 μm in thickness, constituting approximately 90% of the corneal thickness. It consists of approximately 200 to 250 collagen lamellae, each having a thickness of 2 μm and a width ranging from 9 to 260 μm.2 The lamellae span the entire length of the cornea. These lamellae, as well as the collagen fibrils composing them, are parallel, regularly arranged, and layered. The individual collagen fibrils measure 34 to 40 nm in diameter and are separated by a space measuring 20 to 50 nm.2 Peripherally, as the stroma blends into the sclera, the fibrils measure 60 to 70 nm and are less regularly spaced. In contrast, the scleral collagen fibrils measure 28 to 280 nm in diameter, and the collagen bundles measure 30- to 50-μm-wide and 10-μm-thick at the scleral spur and 100- to 140-μm-wide and 10- to 16-μm-thick elsewhere. The periodicity of the corneal stromal collagen fibrils is 62 to 64 nm, whereas that of the scleral stromal fibrils is 80 nm.
Descemet’s membrane consists of regularly arranged layers of very fine collagen filaments and includes at its most posterior limit the basement membrane of the corneal endothelium. In adults this membrane is 10- to 12-μm-thick, whereas at birth it is only 3- to 4-μm-thick. At the edge of the cornea, Descemet’s membrane branches out to form the sheets of trabeculae forming part of the aqueous outflow apparatus. In adults older than age 20 years, Descemet’s membrane demonstrates thickenings (Hassall-Henle warts) that bulge into the anterior chamber.
A single layer of endothelial cells measuring 5 μm in height and 18 to 20 μm in width make up the posterior layer of the cornea. Approximately 500,000 hexagonal cells are present in this layer, and this number decreases with age. Each cell contains 20 to 30 microvilli that project into the anterior chamber and measures 0.1 to 0.2 μm in width by 0.5 to 0.6 μm in height. Corneal endothelial cells are continuous with the endothelial cells that line the space of the iridocorneal angle and the anterior surface of the iris.39
The cornea is richly supplied with sensory nerves. The corneal nerve fibers are derived from the ophthalmic division of the trigeminal nerve. A few superficial sensory nerve endings enter the cornea from the subconjunctival and episcleral areas, but most of the nerve supply is provided transsclerally from the long posterior ciliary nerves. After passing through the choroid and ciliary body, these nerves enter the anterior sclera a short distance posterior to the limbus, where they divide to form the annular plexus. Seventy to 80 large corneal nerves composed of fibers from the branching ciliary nerves enter the cornea radially. Most pass into the middle one-third of the peripheral cornea as myelinated nerve bundles that lose their myelin sheath in the peripheral 1 to 2 mm of cornea. These sensory nerves are found in all corneal layers but are more commonly found in the anterior third of the corneal stroma. The nerves subdivide into smaller side branches and eventually turn abruptly 90 degrees to proceed towards the corneal surface. A well-developed neural net arborizes in the surface corneal epithelium after penetrating Bowman’s layer.
The blood supply and the lymphatics to the cornea are provided by subconjunctival, episcleral, and scleral vessels. These vessels supply the limbus as well and arise from the anterior ciliary arteries.40 Two sets of vessels originate from these arteries: terminal vessels that supply the peripheral corneal arcade before becoming a venous plexus and recurrent vessels that supply a portion of the peripheral cornea measuring approximately 0.5 mm before traveling posteriorly to supply 3 to 6 mm of perilimbal conjunctival and episcleral tissue. These latter vessels anastomose with recurrent conjunctival vessels from the fornix.
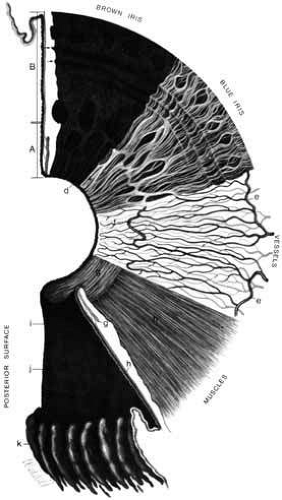
THE IRIS
The iris is the anterior extension of the uvea that forms a mobile diaphragm between the posterior chamber and anterior chamber of the eye (Fig. 8).1,2 The central aperture of the iris forms the pupil, through which light enters the eye. The diameter of the pupil, which varies from 1.5 to 8 mm, is regulated by movement of the iris, thus impacting the amount of light that enters the eye. The iris extends transversely in a radial direction from the center of the eye to approximately 1 mm posterior to the corneoscleral junction where it joins the ciliary body.41 The anterior surface of the iris is visible through the cornea and is separated from the cornea by the anterior chamber of the eye. Its posterior surface faces the posterior chamber, and its central portion is in contact with the anterior surface of the lens. The diameter of the iris is approximately 12 mm. The cornea magnifies the image of the iris by approximately 10%.
The shape of the iris resembles the cut base of a cone, with the apical opening defining the pupillary border surrounding the pupillary aperture (Fig. 9) and the basal aperture defining the peripheral or ciliary border. Thus, in accordance with the convexity of the underlying lens, the pupillary plane of the iris is anterior to its periphery. When compared to the center of the cornea, the center of the pupil is slightly displaced inferiorly and nasally.
The collarette of the iris is a wavy circular line approximately 1 to 1.5 mm from the pupillary border, between the inner one-third and outer two-thirds on the anterior surface of the iris. It marks the zone that separates two concentric rings of the iris: the inner pupillary zone (1–2 mm in width), which contains the sphincter muscle, and the outer ciliary zone (3–4 mm in width). The collarette is the thickest portion of the iris, measuring 0.6 to 1.0 mm; the iris becomes thinner toward the pupil and even thinner in the periphery (0.3–0.5 mm), where it joins the ciliary body.41
The anterior surface of the iris (Fig. 10) is also characterized by small connecting crests in the pupillary zone, deep radial slits known as Fuchs crypts or stomates at the collarette, and deep round ruts, which are mostly incomplete and concentric to the pupillary border in the ciliary zone. The radial ridges are the result of the radially oriented blood vessels and the connective tissue surrounding them in the iris stroma. There is an incomplete circle of arteries (minor circle of the iris) at the collarette. The blood supply to the iris is from the long posterior ciliary arteries that form the major arterial circle of the ciliary body located just peripheral to the iris root.42,43 The anterior surface of a darkly pigmented iris is dense and thickly matted with few visible fibrils, compared with a blue or less darkly pigmented iris. The posterior surface of the iris is black or dark brown, except in albino subjects, and is also characterized by various types of folds or plicae. Schwalbe’s contraction plicae are radial folds in the pupillary region. Schwalbe’s structural plicae are wider than the contraction plicae and are located in the ciliary zone. Circular plicae are fine circular folds present near the papillary margin caused by variations in epithelial thickness.
The iris consists of five layers. The anterior border layer consists of densely packed melanocytes and fibroblasts with little collagen. This layer is thickest at the collarette and thin or absent near iris crypts. It is thinner in nonpigmented irides than in pigmented ones. No endothelium is present over this layer in the adult, although endothelium may cover the iris at birth.1,2 The number of melanocytes present in this layer determines the iris color. Accumulation of Schwann cells is partially responsible for the formation of iris nodules in the anterior border layer, whereas accumulations of melanocytes form “iris freckles.” Capillaries are normally seen in this layer very close to its anterior surface. Peripherally, this layer of cells becomes continuous with cells on the surface of the ciliary body.
The iris stroma consists of loosely arranged collagen as well as melanocytes and fibroblasts. Mucopolysaccharide ground substance and fluid are also present within this iris meshwork. The stroma is loosely connected to the anterior border layer as well as to the sphincter and dilator muscles. The collagen fibrils in the iris stroma are 60 nm in diameter and have an axial periodicity of 50 to 60 nm.44,45
The sphincter muscle is 0.75 to 0.8 mm in width and 0.1 to 0.17 mm in thickness. At the pupillary border, it is separated from the pigment epithelium of the posterior iris surface by a thin collagen band. Posteriorly and peripherally, it is firmly attached to a dense collagen layer that is also attached to the dilator muscle. The sphincter muscle cells are spindle-shaped and oriented circumferentially to the pupillary margin. These cells are wrapped in bundles by a collagen layer. These cells are supplied by parasympathetic nerve fibers from the long ciliary nerves with synapses in the ciliary ganglion. Sympathetic innervation is also supplied to this muscle and its surrounding connective tissue.46
The anterior epithelial layer of the iris and the dilator muscle are approximately 12.5-μm-thick. The cells in this layer consist of an epithelial apical portion and a muscular basal portion. The muscle layer is approximately 4-μm thick and consists of spindle-shaped cells measuring 7 μm in width and 60 μm in length. The muscular portion of these epithelial cells contains numerous myofilaments, whereas the apical portion contains pigment. The dilator muscle portion of the anterior epithelial cell layer extends from the iris root to the stroma posterior to the sphincter muscle. The epithelial cell layer extends onto the ciliary body as a pigmented layer of cells. The dilator muscle is supplied by sympathetic fibers from the superior cervical ganglion. The apical portion of the anterior epithelial layer (i.e., the surface facing posteriorly) is joined to the apical portion of the posterior epithelial layer (i.e., the surface facing anteriorly) by tight junctions and desmosomes. Cilia from both the anterior and posterior epithelial layers often present in areas of separation between the two cell layers.
The posterior epithelial layer of the iris is very heavily pigmented. The cells constituting this layer measure 36 to 55 μm in height and 16 to 25 μm in width. As this layer of cells extends onto the ciliary body, it becomes depigmented. A thin basement membrane is present over the posterior surface of these cells.
THE ANTERIOR CHAMBER AND AQUEOUS HUMOR
The anterior chamber represents an area bordered anteriorly by the posterior surface of the cornea, posteriorly by the anterior surface of the iris and the pupillary portion of the lens, and peripherally by the trabecular meshwork, scleral spur, ciliary body, and iris root, which comprise the anterior chamber angle (Fig. 11). The cellular lining of this space includes the corneal and trabecular meshwork endothelium and the melanocytes and fibroblasts of the anterior border layer of the iris and ciliary body. On cross-section, the anterior chamber appears to be ellipsoidal (shaped like a kidney bean). The greatest diameter of the anterior chamber ranges from 11.3 to 12.4 mm, or approximately the diameter of the cornea. In the horizontal meridian, the anterior chamber angle is 1 mm posterior to the corneal periphery, and in the sagittal meridian it is 0.75 to 1 mm posterior to it.47 The narrowest portion of the anterior chamber is at the angle. However, as the iris changes direction when it inserts into the ciliary body, there is a slight widening of the angle in its furthest recess.
The shortest distance between a coronal plane drawn through the root of the iris and the corneal apex is approximately 4.2 mm, whereas this distance from a coronal plane drawn through the pupil to the corneal apex (anterior chamber depth) is approximately 3.5 mm (1.99–4.75 mm).48 There is considerable variability in anterior chamber depth based on refractive error, age, sex, ethnicity, genetics, and the amplitude of accommodation.4,49,50,51,52,53 The anterior chamber is deeper in myopic eyes relative to hyperopic ones.54 Generally, in hypermetropia, the anterior chamber depth ranges from 3 to 3.5 mm, in emmetropia it ranges from 3.1 to 3.6 mm, and in myopia it ranges from 3.3 to 3.8 mm. The anterior chamber depth also decreases with age, probably because of thickening of the lens.55,56 At age younger than 15 years, the anterior chamber depth is approximately 3.6 to 3.65 mm. Between 15 and 35 years, it has been measured at 3 to 3.7 mm, and between the ages of 35 and 55 years it ranges from 2.8 to 3.3 mm. Finally, at older than age 55, this distance has been variously measured between 2.7 and 3.2 mm. Orbscan topographical evaluations of the anterior chamber depth have shown that men and those with darker irides have deeper chambers than women and those with lighter irides.48 In a study of ocular refraction and its biometric determinants in 114 twin pairs, Lyhne et al. found that the anterior chamber depth had a high degree of concordance between twins and that a dominant genetic effect was the most likely explanation.57 With maximal accommodation, the anterior chamber depth decreases by an average of 0.24 mm.58
The anterior chamber contains aqueous humor. This is a crystal-clear fluid with a specific gravity between 1.0034 and 1.0036. The index of refraction of this fluid is 1.3336 and is less than that of the lens, which is 1.39.59 The volume of the anterior chamber and the aqueous humor it contains is approximately 250 μL. It decreases by 0.11 μL per year of life and is approximately 0.69 μL larger per diopter of myopia.60 In comparison, the posterior chamber is much smaller, with a volume of 60 μL.59 The balance between the rate of aqueous production and outflow determines the intraocular pressure. The aqueous humor provides nutrients for the avascular lens and cornea and the egress for waste products from these structures. It has 0.1% to 0.2% of the concentration of plasma protein (20 mg/100 mL) and a higher concentrations of amino acids than plasma. When the protein concentration increases, the resultant scattering of light (Tyndall effect) is visible as flare biomicroscopically.61 Ascorbate is present at approximately 20 times that of normal plasma concentrations and may be important in protecting the anterior segment structures from the oxidative effects of ultraviolet light.62 Lactate concentrations are relatively high due to the glycolytic activity of the lens.63 The rate of aqueous humor production is approximately 2 to 2.5 μL/min. Approximately 1% of the anterior chamber and 1.5% of the posterior chamber volume of aqueous humor are replaced each minute.61,64
ANTERIOR CHAMBER ANGLE AND AQUEOUS OUTFLOW STRUCTURES
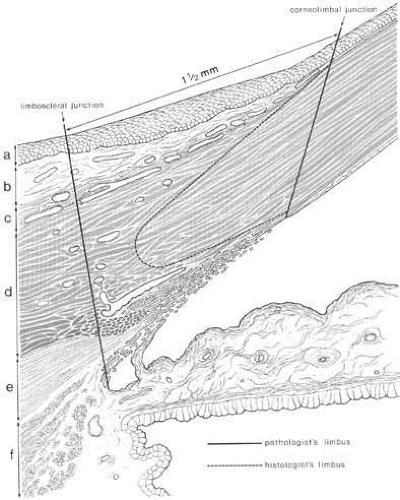
The corneoscleral limbus is the circumferential zone that contains transition of corneal to sclera65,66 (Fig. 11). It is approximately 1 to 1.5 mm in width in the horizontal meridian and 1.5 to 2 mm in width in the vertical meridian. The posterior edge is referred to as the scleral limbus and the anterior edge as the corneal limbus. The corneal limbus is defined by a line that connects the termination of Bowman’s layer (biomicroscopically apparent as the terminations of the marginal corneal vascular arcades) to the termination of Descemet’s membrane (apparent as Schwalbe’s line on gonioscopy). The scleral limbus is clinically less apparent and defined by a line passing through the scleral spur and perpendicular to the external surface. The limbus can be further divided into three zones: (1) the superficial limbus, which is contains the episclera, Tenon’s capsule, conjunctival stroma, and limbal conjunctival epithelium; (2) the middle limbus, which contains the termination of the corneal stroma as it projects posteriorly and transitions into the scleral stroma; and (3) the deep limbus, which consists of the trabecular meshwork and Schlemm’s canal.11
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree