Etiology
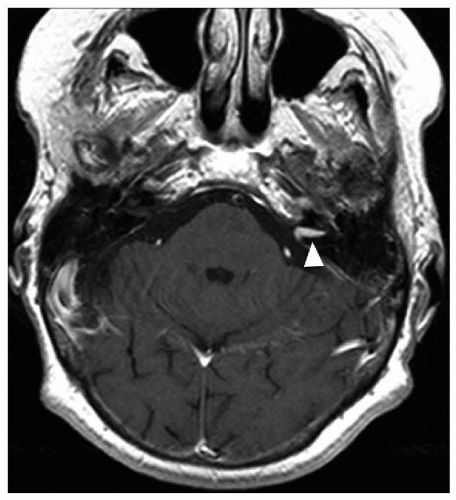
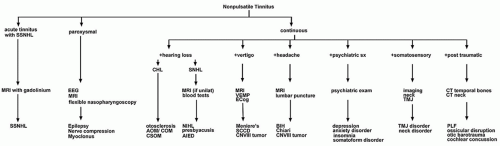
A variety of clinical entities may underlie nonpulsatile tinnitus. Most often, these conditions cause hearing loss, which is thought to be the initial step in the generation of tinnitus in these patients. Noise-induced hearing loss, presbyacusis, ototoxic medications, labyrinthitis, herpes zoster oticus, Meniere’s disease, and genetic hearing losses cause inner ear hair cell damage resulting in hearing loss, which can lead to nonpulsatile tinnitus. Chronic otitis media, cholesteatoma, canal occlusion, and otosclerosis can cause a conductive hearing loss that ultimately may result in tinnitus. Lesions that affect the cochlear nerve and central nervous system (CNS) such as acoustic neuroma, meningioma, multiple sclerosis, and Charcot-Marie-Tooth disease can also induce tinnitus, typically along with a coincident hearing loss (
Fig. 161.1,
Table 161.1).
However, not every patient with a hearing loss will have tinnitus. Additionally, patients without a discernable hearing loss (including evaluation with a high-frequency audiogram) or other identifiable pathology may suffer from tinnitus as well. Other primary causes of tinnitus include pharmacologic or dietary stimulants, head trauma, and psychiatric disorders. Drugs or stimulants
which increase neural firing, such as aspirin, nonsteroidal anti-inflammatory medication, nicotine, ethanol, and caffeine, can cause or exacerbate nonpulsatile tinnitus (
Table 161.2).
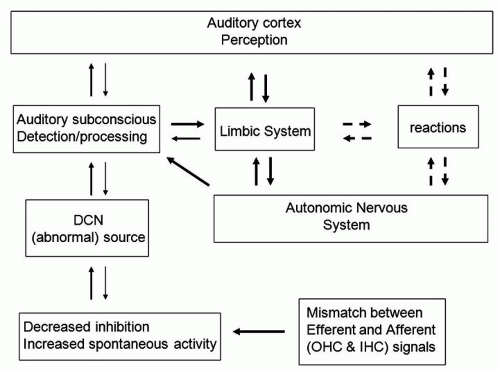
The underlying mechanism of nonpulsatile subjective tinnitus, including the generator of the noise, has not yet been described. Advances in experimental and imaging techniques have revealed significant insights into the etiology of this disorder. These insights may ultimately guide rational treatment of this form of tinnitus.
Initial theories of the generation of nonpulsatile tinnitus focused on the role of the cochlea, specifically the role of certain cochlear structures such as outer hair cells. These theories flowed logically from observations that subjective nonpulsatile tinnitus is frequently seen in individuals with measurable hearing loss or following known ototoxic injuries (such as ototoxic medication exposure, noise exposure, head injury). However, later findings, such as the persistence of tinnitus following truncation of the auditory nerve or ablation of the cochlea, disproved these exclusively cochleogenic etiologies for the majority of sufferers of subjective nonpulsatile tinnitus (
6,
7,
8).
More recently, imaging studies on humans with tinnitus and animal studies have revealed changes in neural activity and connectivity throughout the auditory system following loss of hearing. The spontaneous firing rate of auditory neurons increases during tinnitus, a phenomenon that may generate the tinnitus sound (
9,
10). Another possibility is that increased synchrony of firing within auditory pathway neurons may be perceived as tinnitus (
9,
11). Many studies have noted a decrease in inhibitory neural input at multiple sites along the central auditory pathways, including the dorsal cochlear nucleus (
12,
13,
14,
15). This leads to a net increase in excitatory signaling in the auditory pathway and has been proposed as the neurophysiologic basis for subjective tinnitus.
Others have proposed that neuronal plasticity may lead to tinnitus. Following hearing loss, studies in animals and humans have demonstrated a change in the tonotopic map throughout the auditory system. Some have proposed that these plastic changes in the frequency representation in areas of the brain and brainstem are the origin of tinnitus, while others have suggested that these changes in the tonotopic map are merely epiphenomena of that hearing loss (
16). Many other plastic changes also follow
deafferentation of areas of the auditory system, including changes in synaptic structure and firing patterns, formation of new synapses and elimination of others, and dendritic branching. All of these changes may underlie the complaint of nonpulsatile tinnitus (
16).
None of these etiologies address patients with complaints of tinnitus who fall into two categories encountered in clinical practice. One is the patient who has had hearing loss for years and yet awakens suddenly with tinnitus. The other is the rare patient who has normal hearing, even in the ultra-high frequencies, no other dietary or toxic risk factors, and no psychiatric comorbidities who complains of tinnitus. For these patients, careful historytaking may uncover a traumatic or emotional event that was coincident with the onset of their tinnitus. Similarities between tinnitus and phantom limb pain have fueled the hypothesis that both are “aversive memory networks.” According to this theory, the phantom awareness (tinnitus) only becomes conscious when linked to other brain networks, and then becomes bothersome when linked by learned associations with unpleasant emotions (
17).
Risk Factors
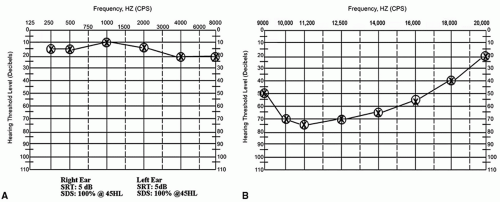
The most prevalent risk factor for subjective, nonpulsatile tinnitus is hearing loss. As discussed above, hearing loss may be the initial instigating factor underlying nonpulsatile tinnitus. Frequently this hearing loss includes significant sensorineural losses at higher frequencies; occasionally, the hearing loss can only be detected using a high-frequency audiogram (
Fig. 161.2). Of note, not every patient with hearing loss will have complaints of tinnitus,
and in fact, at least 27% of patients with profound sensorineural hearing loss (SNHL) will not have tinnitus (
18). Meniere’s disease is associated with nonpulsatile tinnitus that typically worsens during acute vertiginous episodes. Conductive or mixed hearing loss can also be associated with tinnitus, including that caused by otosclerosis, ossicular discontinuities, or obstruction of the external auditory canal by cerumen or other factors.
Other risk factors for nonpulsatile tinnitus include intake of certain dietary, medicinal, and illicit substances. For instance, caffeine, aspirin, ibuprofen, and nicotine can cause tinnitus or exacerbate preexisting tinnitus. Even if the individual patient has used these substances previously, changes in intake patterns due to shift work, injury, or changes in metabolism due to aging can lead to worsened tinnitus.
Hyperacusis
Hyperacusis, or increased sensitivity to sound, is often seen in the context of tinnitus. Patients will complain of discomfort or pain in the presence of sounds that are typically tolerated by normal people, including car horns, sounds associated with cooking, and even loud conversations. Sometimes this sound intolerance will be limited to certain frequencies. As the patient continues to experience hyperacusis, the threshold of sound intensity required to cause discomfort may decrease. In severe cases, patients may significantly alter their behavior (wear ear muffs in public, avoid going outdoors) in order to avoid the discomfort and pain caused by exposure to these sounds. Often, hyperacusis is associated with hearing loss (
19).
For patients with hearing loss, intolerance to loud sounds may result from overrepresentation of the sound frequencies bordering a hearing loss in the central auditory system (recruitment). Exposure to these sound frequencies causes intolerable overstimulation of the auditory cortex due to recruitment. A second possibility is that hyperacusis results from selective loss of efferent input to the inner ear. These efferents are critical in regulating basilar membrane excursion and firing of afferent eighth nerve fibers in response to a sound stimulus (
20).
Patients may develop hyperacusis following a single exposure to a sudden loud noise (e.g., gunshot, car airbag deployment) in the absence of a detectable hearing loss. Other potential etiologies for hyperacusis in the absence of hearing loss include head trauma, migraine, depression, Bell’s palsy, Ramsay Hunt Syndrome, Lyme disease, Addison’s disease, and following stapes surgery (
19,
20). Hyperacusis is seen in over 80% of patients with Williams syndrome, a genetic disorder characterized by craniofacial and dental anomalies, mental retardation, hypertension, cardiovascular disease, and perfect pitch (
21,
22).
Mild hyperacusis can be managed by avoidance of sounds that stimulate an unpleasant reaction (
19). Thus for hearing aid users with hyperacusis, the maximum comfort level should be utilized in programming their aids. Further treatment is required for patients with severe hyperacusis that affects their activities of daily living. For these patients, tinnitus retraining therapy (TRT) can be extremely effective in increasing their tolerance to everyday sounds (
23).
Diagnostic Evaluation
Patients with nonpulsatile, subjective tinnitus should always have a standard, complete audiogram performed as the initial step in their evaluation, as discussed above. For patients with complaints of bilateral tinnitus who have a normal standard audiogram (up to and including 8,000 Hz pure tone thresholds), a high-frequency audiogram may be useful in determining the etiology of tinnitus, particularly in patients with no other risk factors.
Magnetic resonance imaging (MRI) of the brain and brainstem with gadolinium is a requisite test for patients with unilateral tinnitus (
Fig. 161.3). Even in the presence of
normal or symmetrical hearing, patients with unilateral tinnitus may have a vestibular schwannoma or other intracranial anomaly requiring further treatment (
25) (
Fig. 161.1). The complete evaluation of patients with symptoms consistent with Meniere’s disease also should include an MRI.