17 Core Messages • Evaluation of the unknown primary mandates a methodical process. • A thorough history and physical examination is beneficial in the identification of a primary lesion. • The location of lymph node metastases can guide the identification of the primary tumor. • Although the examination and biopsy in the clinic may be definitive, evaluation in the operating room is often necessary. • Identification of the primary decreases patient morbidity via more focused radiation therapy portals. • A positron emission tomography scan is complementary to history, physical examination, triple endoscopy with biopsy, and conventional imaging. The views expressed in this chapter are those of the authors and do not necessarily reflect the official policy or position of the Department of Navy, the Department of Defense, or the U.S. government. I am a military service member. This work was prepared as part of my official duties. Title 17 U.S.C. 106 provides that “Copyright protection under this title is not available for any work of the United States Government.” Title 17 U.S.C. 101 defines a U.S. government work as a work prepared by a military service member or employee of the U.S. government as part of a person’s official duties. Carcinoma of unknown primary (CUP) is defined as the presence of histologically confirmed metastatic cancer in a patient without an identifiable primary tumor despite a standardized diagnostic approach that includes medical history, physical examination, appropriate laboratories, panendoscopy, and conventional imaging. Metastasis to a regional lymph node is often the initial presentation of a primary head and neck carcinoma. Although the primary lesion may often be readily identified during a thorough head and neck examination, in 3 to 5% of the cases there is no apparent aerodigestive lesion.1 Recent advances in imaging hold promise for improved detection; however, the work-up of the patient with CUP remains a challenge. Discovery of the primary tumor improves patient morbidity by decreasing the necessary volume of irradiated tissue. In a small percentage of patients, the primary will not be identified after a thorough evaluation including fiberoptic nasopharyngeal and laryngeal endoscopy, panendoscopy with biopsies, and appropriate imaging. Controversy surrounds the further evaluation and management of this patient population. The true incidence of CUP of the head and neck has not been definitively determined. American Cancer Society (ACS) data from 2010 lists the incidence of “Other & unspecified primary sites” as 30,680 for an incidence of 2% of all cancers. This number has been consistent with previous years. However, there is no specific data for cervical squamous cell CUP versus other anatomic locations. The estimated number of deaths is 44,030 for an overall cancer death rate of 7%. The larger number of deaths versus incidence may reflect lack of specificity in recording the underlying cause of death or an undercount in the case estimate.2 The true rate of CUP could be estimated at around 2%, possibly lower because of other anatomic sites being included in the ACS numbers or higher because of undercounting of cases. One interesting question that could not be answered in our data review is whether the true incidence of CUP is decreasing in response to advances in imaging technology. This question will probably remain elusive because of the relative infrequency of head and neck squamous cell carcinoma (HNSCC) of unknown primary. In addition, a patient who is identified as having CUP may later develop a primary tumor, thereby removing himself or herself from the CUP population. A commonly quoted estimate of the incidence of CUP in multiple references is 2 to 9% of all head and neck cancers (HNCs). It includes numerous tumor types and locations. Squamous cell carcinoma is responsible for 90% of all cervical metastasis of unknown primary.3 The risk factors for CUP are the same as those for known primary squamous cell carcinoma of the head and neck: alcohol, tobacco exposure, and human papillomavirus (HPV). Different theories attempt to explain the phenomenon of the unknown primary. One thought is that the primary exists and the work-up just failed to locate it; however, even long-term follow-up often fails to identify a primary tumor. Other theories are that the primary tumor regressed after early metastasis or that the tumor sloughed off into the digestive tract. The most common presentation of CUP is a new, painless neck mass, increasing in size, present in a patient with a long history of tobacco and alcohol abuse. HPV-related carcinoma may present in patients without the tobacco and alcohol history. The absence of the most common presentation should not preclude a thorough evaluation. Localization of the primary tumor is paramount to reduction of patient morbidity and will allow for surgical resection and/or a higher radiation dosage to the site of the primary, thereby decreasing overall patient morbidity. The first, and most critical, step in the evaluation of any patient with a new cervical mass is a thorough history and physical examination. The temporal development of the mass, location, and changes in size and color should be noted. The history should include etiologic factors: tobacco and alcohol history as well as standard HNC review of system questions (Table 17.1). Consideration should also be made for environmental exposures that put patients at risk for nasopharyngeal squamous cell carcinoma: wood dust and nickel exposure. Recent immigration from China or Hong Kong could indicate an increased risk of nasopharyngeal carcinoma. Medical and surgical history should be reviewed. Often, the HNC patient population has significant comorbidities that preclude aggressive therapy. Ensure you ask your patient about pertinent drug allergies. All skin areas of the head and neck should be inspected. Careful visualization and palpation of hair-bearing scalp areas is required. Physical examination consists of direct inspection of all pharyngeal and laryngeal mucosal surfaces. Palpation of the tongue base and tonsils can reveal subtle masses not appreciated on visual examination and should be performed on every patient who can tolerate it. The neck should be palpated, and the level of the mass should be determined. A small subset of patients will have multiple neck metastases. Levels II and III are the most common neck levels of presentation. Direct examination with a mirror may allow visualization of the laryngeal anatomy; however, a patient with a severe gag-reflex will often allow only a limited view. Fiberoptic examination is the preferred method for evaluation in nearly all cases (Fig. 17.1). After proper topical anesthesia and vasoconstriction, this modality allows an excellent view that is well tolerated by most patients and is recordable for documentation, peer review, and later comparison. Table 17.1 Questions for History-Taking
The Unknown Primary
Background
Diagnosis
History
Physical Examination
History of head and neck carcinoma/skin cancer |
Dysphagia/aspiration |
Unintentional weight loss |
Night sweats |
Hoarseness |
Odynophagia |
Hemoptysis |
New masses or ulcers |
Stridor |
Change in denture fit |
Otalgia |
Unexplained fevers |
Location of the Mass
The mass location can indicate a likely primary source. Table 17.2 illustrates potential primary sites on the basis of the location of the cervical metastases. Special consideration should be given to occipital nodes for a scalp primary and supraclavicular nodes for a nonhead and neck primary.
Laboratory Studies
Screening laboratory studies of the patient with CUP should include complete blood cell count, liver-associated enzymes, and thyroid function tests, modified as appropriate for any comorbidities. The usefulness of routine screening laboratories has been questioned in the general population,4 however; HNC patients have a higher prevalence of comorbidities and often undergo larger surgical procedures. This fact may justify the routine usage of screening laboratories in these patients.
Figure 17.1 Examination of the nasopharynx may reveal the primary lesion, in this case a nasopharyngeal carcinoma.
Table 17.2 Lymph Node Metastases—Potential Primary Sites
Level | Possible Primary |
Ia | Floor of mouth, oral tongue |
Ib | Mandibular alveolus, floor of mouth, oral tongue, retromolar trigone, pharynx, oropharynx |
II | Ib sites, plus supraglottis, piriform, glottis |
III | Tongue, oropharynx, supraglottis, piriform, glottis |
IV | Pharynx, oropharynx, piriform, supraglottis |
V | Oropharynx |
Occipital | Scalp |
Supraclavicular node | Discuss possibility of nonhead and neck origin and likely sites: breast, lung, gastrointestinal tract associated with thoracic duct |
Adapted from reference 16.
Some authors have recommended testing for Epstein-Barr virus antibody titers in the setting of nonkeratinizing or poorly differentiated carcinoma, when a nasopharyngeal primary might be suspected. As noted by Neel in 1985, positive viral capsid antigen IgA and early antigen tests may indicate the presence of World Health Organization type 2 and 3 nasopharyngeal carcinomas. Patients with type 1 carcinoma exhibit a lower incidence of these antigen responses.5
Tissue Diagnosis
After history and physical examination, fine-needle aspiration (FNA) will provide the best opportunity for the diagnosis of malignancy. Traditionally, incisional/excisional biopsy of neck masses has been discouraged because of the possibility of hindering cure. However, there is contradictory evidence in the literature about the effect of open biopsy on locoregional control and ultimate survival. The most compelling reason to first consider nonsurgical techniques for diagnosis is that there is a high probability that a diagnosis may be made without resorting to open biopsy.
FNA, either direct or under ultrasound guidance, can usually be performed in an office setting. Whenever possible, the aspirate should be assessed for adequacy during the procedure. In our institution, a cytopathology technician is called to the clinic room. Fig. 17.2 illustrates a typical setup for this procedure. The patient’s skin is prepped with alcohol or Betadine swabs and draped with a blue towel. Local anesthesia with lidocaine is infrequently required. A 22- to 25-gauge needle is connected to either suction tubing or a biopsy gun. Insertion into the tumor along the long axis is made. When the bevel of the needle is subdermal, suction is applied. Some surgeons prefer not to use suction. Gentle back-and-forth motion is made for several passes. Then, the needle is withdrawn off suction and passed to the cytopathologist for immediate staining and a preliminary read.
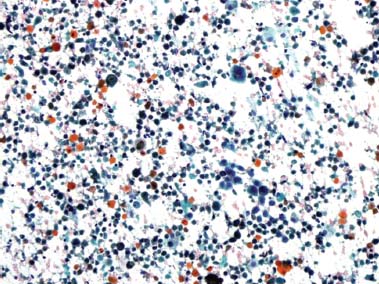
Cellular analysis of the aspirate or surgical specimen by the pathologist with light microscopy, special staining, immunohistochemistry, and even electron microscopy can aid in determining tissue origin. The ease of diagnosis of tissue type is related to the degree of differentiation in the tumor. For poorly differentiated tumors, more complex analysis is often necessary. Special staining for keratin, S-100, or mucin can aid in diagnosis. Electron microscopy can detect cellular features not seen with light microscopy. DNA amplification of Epstein-Barr virus has been used to detect occult nasopharyngeal carcinoma. Figs. 17.3 and 17.4 illustrate the FNA appearance of moderately differentiated squamous cell carcinoma.
The great majority of tumors will be classified as squamous cell carcinoma, likely relating to the most common site of origin in Waldeyer ring. However, other sites of origin should be considered. The thyroid, parathyroid, cervical nerves, and larynx can produce neck masses. The possibility of distant metastasis to the neck should also be considered, especially with level 4 and 5 neck masses. Establishing the tissue diagnosis of squamous cell carcinoma in the first clinical visit can greatly aid in diagnostic and therapeutic planning. This knowledge may also help determine the need for dental extractions. Hematology/oncology and radiation oncology consults can also be made confidently. Once a diagnosis of carcinoma is made, insurance approval for positron emission tomography (PET) scanning can also be secured.
< div class='tao-gold-member'>