15 The Retina: Vascular Diseases II
DIABETIC RETINOPATHY
Fig. 15.2 (Top) These retinal trypsin digest preparations show early capillary damage and microaneurysms. (Top left) There are small areas of capillary loss, many of the capillaries are acellular, and small microaneurysms can be seen along dilated and more hypercellular capillaries. (Top right) More marked capillary dropout and well formed microaneurysms. (Bottom) An Indian ink injected preparation showing capillary nonperfusion, capillary loops and microaneurysms.
Top figures reproduced with permission from The Retinal Circulation, edited by Wise, Dollery and Hawkin, Harper & Row, 1971.
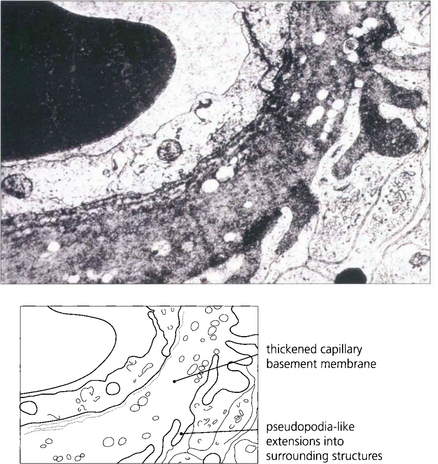
Fig. 15.3 An electron micrograph showing capillary basement membrane thickening and pseudopodia-like extensions into surrounding structures.

Fig. 15.4 A trypsin digest preparation showing eosinophilic staining of degenerate capillary pericytes.
CLASSIFICATION OF DIABETIC RETINOPATHY
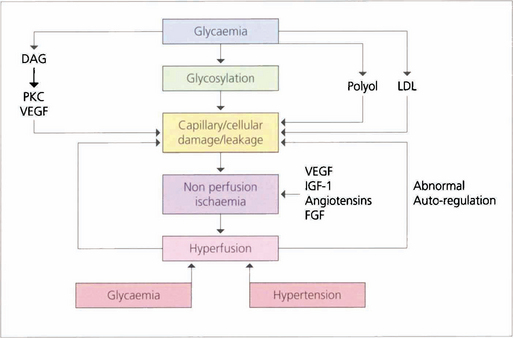
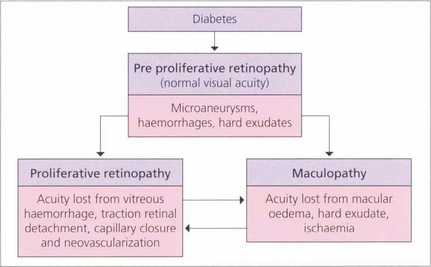
The initial clinical features of diabetic retinopathy are microaneurysms, small retinal haemorrhages and small areas of capillary closure (Table 15.1). Visual acuity is commonly normal at this stage, although subclinical changes in colour vision and contrast sensitivity might be found. This is followed by vascular leakage, hard exudate and cotton-wool spots. Retinopathy may progress to compromise vision in two ways: (1) maculopathy develops with oedema, lipid exudation or ischaemia, or (2) a proliferative retinopathy occurs, in which retinal hypoxia and neovascularization predominate and reduce vision by vitreous haemorrhage or traction retinal detachment. Not uncommonly, both mechanisms coexist in the same patient. Diabetic retinopathy is staged by its clinical features. Maculopathy is classified by extent as focal or diffuse, and by mechanism as exudative, ischaemic or mixed.
Table 15.1 Classification of diabetic retinopathy
| Descriptive term | Features |
|---|---|
| No diabetic retinopathy (DR) | |
| Mild or moderate nonproliferative DR | Microaneurysms, retinal haemorrhages and exudate |
| Severe nonproliferative DR | Deep retinal haemorrhages in four quadrants, or venous beading or loops in two quadrants, or the presence of IRMAs |
| Proliferative DR without high-risk characteristics | New vessels on the disc smaller than one-third of a disc diameter without vitreous or preretinal haemorrhages or new vessel elsewhere only |
| Proliferative DR with high-risk characteristics | New vessels on the disc larger than one-third of a disc diameter or any new vessel with vitreous or preretinal haemorrhages |
| Advanced proliferative DR | Tractional retinal detachment, unresolved vitreous haemorrhage, rubeotic glaucoma |
NATURAL HISTORY
Risk factors for the progression of retinopathy are the duration of diabetes and the type (type I is worse than type II). Recent clinical trials have shown that meticulous long-term glycaemic and blood pressure control retards the onset and progression of diabetic retinopathy. Tightening poor glycaemic control may, however, initially markedly worsen retinopathy and cause neovascularization, possibly because initiating good control lowers retinal blood flow and exacerbates ischaemia. Careful monitoring of diabetic retinopathy when altering glycaemic control is therefore critical. Pregnancy, renal disease and cataract surgery may worsen the retinopathy whereas high myopia, optic atrophy, glaucoma, central retinal artery occlusion and carotid artery stenosis appear to protect, possibly by reducing retinal metabolic demand (Table 15.2). Diabetic retinopathy is not seen before puberty.
Table 15.2 Risk and protective factors for progression of retinopathy
| Risk factors | Protective factors |
|---|---|
| Duration of diabetes | High myopia |
| Poor long-term control | Optic atrophy |
| Tightening of poor control | Glaucoma |
| Hypertension | Carotid stenosis |
| Pregnancy | Retinal artery occlusion |
| Renal failure | |
| Hyperlipidaemia | |
| Puberty |
MILD AND MODERATE NONPROLIFERATIVE DIABETIC RETINOPATHY (NPDR)
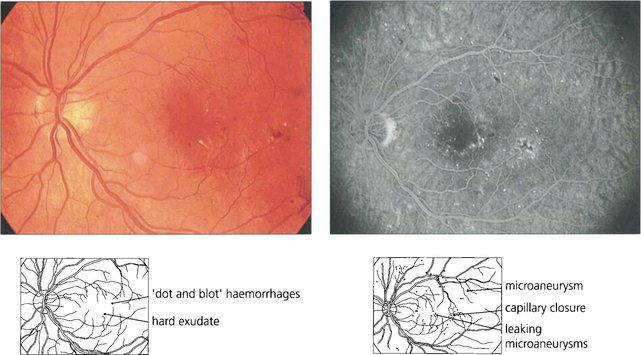
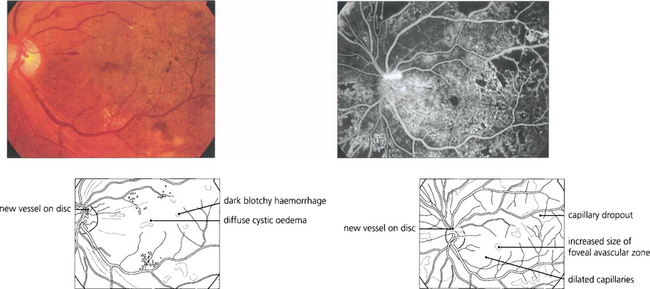
Fig. 15.6 This patient shows the typical changes of early retinopathy with scattered microaneurysms, blot haemorrhages and hard exudates and cotton-wool spots in the posterior pole. The macula and visual acuity are normal. The retinopathy can fluctuate, improving or deteriorating over a period of time. Fluorescein angiography demonstrates extensive microvascular changes throughout the posterior pole with scattered microaneurysms and minimal vascular leakage. Many more microaneurysms are visible that can be seen clinically. Although in some areas capillary patterns around the macula are irregular and show minor areas of capillary closure, they are, in the main, complete.

Fig. 15.7 With early retinopathy, the retina temporal to the macula is often susceptible to earlier and more pronounced changes; elsewhere in the posterior pole of this patient, retinopathy is comparatively sparse.
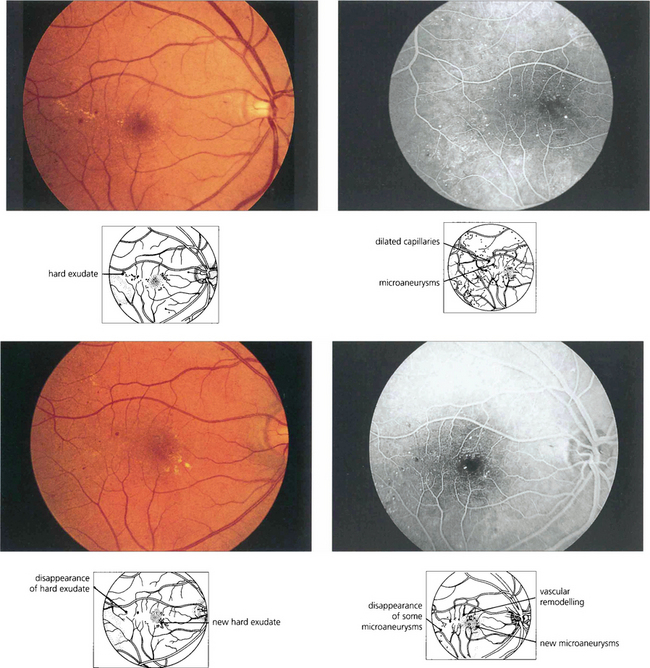
Fig. 15.9 Background retinopathy appearances can fluctuate and do not progress relentlessly. These photographs were taken 18 months apart. The later photograph (top right) shows that the exudates temporal to the macula have been absorbed spontaneously and new exudate has appeared inferior to the macula. Comparison of angiograms from the same patient shows there has been a considerable change in the pattern of the microaneurysms. New microaneurysms have formed and others, on the temporal side of the macula in particular, have disappeared over the same period of time.
SEVERE NONPROLIFERATIVE DIABETIC RETINOPATHY
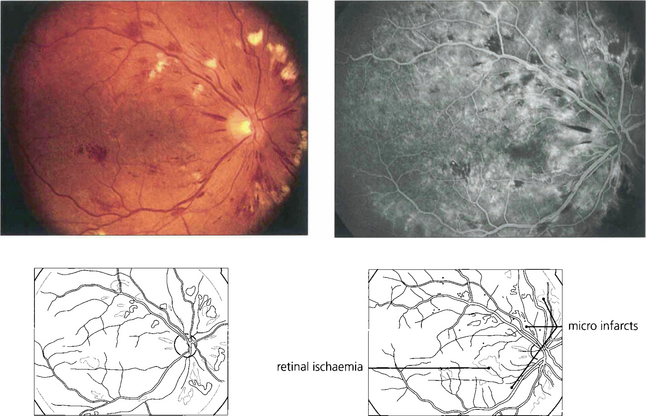
Fig. 15.10 Numerous cotton-wool spots, which persist for longer in diabetes (up to 3 months) than with other causes indicate marked retinal ischaemia, as confirmed on angiography.
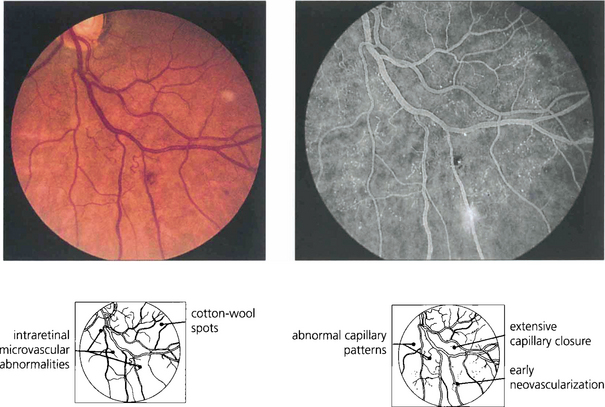
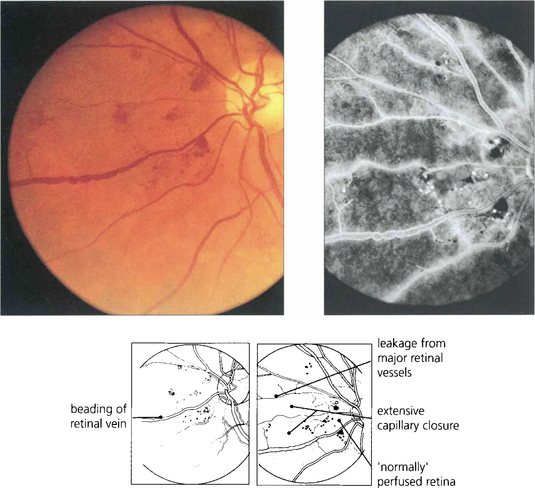
Fig. 15.11 Areas of intraretinal microvascular abnormalities (IRMAs) with dilated tortuous veins along the inferior temporal arcade are seen in this patient. IRMAs represent intraretinal neovascularization and are found at the border of areas of nonperfusion. They are entirely intraretinal and do not leak fluorescein. As they are associated with nonperfusion it is not surprising that they are associated with an increased risk of PDR.
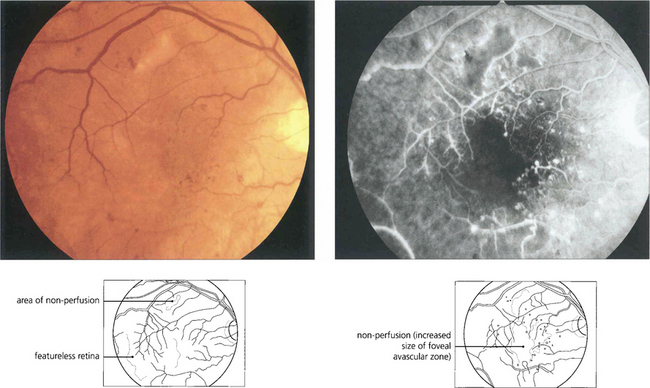
Fig. 15.12 Areas of nonperfusion can often be recognized ophthalmoscopically by their flat featureless appearance and relative absence of microvascular changes.
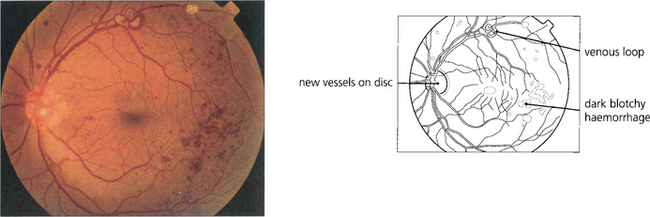
PROLIFERATIVE DIABETIC RETINOPATHY (PDR)
In common with neovascularization elsewhere in the eye these vessels have fenestrated endothelial cell junctions and tend to leak, while minor trauma and vitreous traction causes them to tear and bleed to cloud the ocular media. Subsequent formation of fibrous tissue produces traction bands between the retina and posterior vitreous face; these eventually contract and detach the retina (see Ch. 12).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree