Endoscopic sinus surgery is an excellent treatment option in the management of medically refractory chronic rhinosinusitis. Continual refinements in endoscopic technique are simultaneously allowing an expanded range of applications and a lower rate of complications for this kind of surgery. However, the potential for serious complications is ever present. The sinus surgeon must always be aware of this, and actively seek to identify high-risk situations preoperatively. The technical points presented in this article should be followed to minimize the risk of complications.
Endoscopic sinus surgery (ESS) is effective in improving the symptoms of chronic rhinosinusitis and thus in ameliorating the quality of life of patients suffering from this common disease. However, one important drawback to this type of surgery remains the potential for serious complications. This is inevitably because of the proximity of critical anatomic structures such as the orbit, the internal carotid arteries, the skull base, dura, and brain.
Several risk factors exist for the occurrence of complications in ESS ; these can be broadly divided into anesthetic, surgeon-related, and disease-related factors. General anesthesia increases the risk of complications because of the lack of patient feedback when approaching sensitive structures like the lamina papyracea and the skull base. Right-sided surgery for a right-handed surgeon is a risk factor, as is left-sided surgery for a left-handed surgeon, because of the angle of the endoscope and instruments. Another risk factor is lack of surgeon experience, for the obvious reasons of unfamiliarity with the anatomy and use of instrumentation. Extensive sinus disease, excessive bleeding, and revision surgery, all of which can obscure or distort the sinonasal structures normally encountered during surgery, are important risk factors.
Although some of these factors are unavoidable, and the avoidance of others such as general anesthesia is impractical, there are several measures and technical points that can be used to remain safe when performing ESS. This article highlights 10 pearls that are routinely taught in our institution and have stood us in good stead. We believe that by adhering to these simple principles, ESS can be made safe and the likelihood of intraoperative complications reduced.
Identify high-risk situations
Before surgery can begin, preoperative imaging must be carefully scrutinized. This is done to identify anatomic variants that, if unrecognized, may lead to adverse outcomes. A high-definition helical multislice computed tomography (CT) scan of the sinuses should be obtained after an adequate trial of maximal medical therapy. Ideally, cuts should measure between 0.5 and 1 mm in the axial plane, and be reconstructed in the coronal and parasagittal planes.
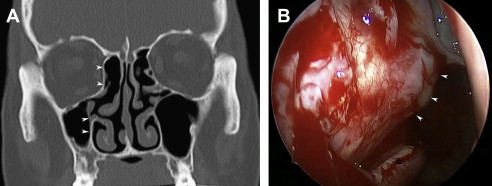
Several key areas must be systematically evaluated on the preoperative CT scan. As a memory aid for performing this thorough checklist, the acronym CLOSE can be used. The “C” stands for cribriform plate, the position of which should be assessed according to the Keros classification. A deeper olfactory fossa with a longer lateral wall ( Fig. 1 ), such as with Keros 2 and 3, exposes a longer lateral wall of thin bone at risk of injury and leaking of cerebrospinal fluid (CSF). The angle that this lateral wall forms with the perpendicular should also be assessed, because those that are more tilted (away from the perpendicular plane) are predisposed to skull base injury during dissections of the frontal recess ( Fig. 2 ). The “L” stands for lamina papyracea, which should be scanned along its entire length, looking for dehiscences or orbital fat protrusion into either the ethmoid or maxillary sinuses ( Fig. 3 ). The lamina may also be in an excessively medialized position relative to the lateral nasal wall, particularly in cases of atelectasis of the maxillary sinus ( Fig. 4 A, B). This situation must be recognized before performing the uncinectomy, or anterior ethmoidectomy, as either of these steps can readily result in orbital penetration. The “O” stands for Onodi cell and optic nerve dehiscence. An Onodi cell is a posterior ethmoid cell that pneumatizes into the superolateral aspect of the sphenoid sinus, and its presence places the optic nerve at risk of injury during instrumentation of the posterior ethmoids. This cell is best detected if there is a horizontal septation within the sphenoid sinus, as seen in the first coronal CT slice in which the complete posterior bony choana can be identified ( Fig. 5 ). The “S” stands for the sphenoid and skull base. The pneumatization of the sphenoid sinus needs to be assessed; if the anterior clinoid is pneumatized, the optic nerve may be in a mesentery across the roof of the sphenoid. In addition, the internal carotid arteries should be assessed for overlying bony dehiscences, a medialized trajectory, or the presence of an aneurysm. It is also important to assess the vertical height of the posterior ethmoids. If unrecognized, a very low-lying ethmoid roof may be inadvertently breached on entering the posterior ethmoids through the ground lamella. The “E” stands for the (anterior) ethmoidal artery. If the anterior ethmoidal artery is in a mesentery hanging below the skull base (see Fig. 1 ), this must be appreciated preoperatively, to avoid severing the artery as the septations on the skull base are removed.




Optimize the surgical field
It is essential to reduce the amount of blood obscuring the visual field in ESS. This will allow proper visualization of the landmarks that are critically important to the safety and success of surgery. Several measures can be taken intraoperatively to reduce bleeding ; these include reverse Trendelenburg positioning, the application of topical and local vasoconstrictors, maintaining the mean arterial pressure at around 75 mm Hg and the heart rate less than 60 beats/min. This is best achieved with total intravenous anesthesia. A preoperative course of systemic steroids may also be beneficial to reduce the size and vascularity of nasal polyps, thus reducing capillary bleeding during ESS. However, the optimal dose, length of treatment, and ideal groups of patients who would benefit from this treatment require further research.
There are several patient factors that predispose to increased bleeding, and thus, a poor surgical field. These should be actively sought and, if possible, dealt with preoperatively. Local factors include acute infection, inflammatory processes including the granulomatous diseases, and excess local tissue trauma during dissection. If suspected clinically, active infection of the sinuses should be treated with an appropriate course of preoperative antibiotics. Systemic comorbidities that can increase surgical bleeding include hypertension, peripheral vascular disease, and liver and renal diseases. Chronic alcohol abuse, malnutrition, and vitamin deficiencies (most notably vitamin K), can also affect coagulation, and must be explored if suspected clinically. Bleeding diatheses such as hemophilia A or B and von Willebrand disease, require clotting factor replacement or specialized pharmacotherapy (desmopressin [DDAVP], tranexamic acid, or aminocaproic acid), and must be planned for. Medications affecting surgical field, including aspirin, nonsteroidal antiinflammatory drugs, warfarin, and antiplatelet agents, must be discontinued for an adequate length of time before surgery, in consultation with the patient’s regular treating physician. Several herbal and alternative therapies, such as ginseng, ginkgo and kava, can affect coagulation pathways, and the surgeon should be aware of these. It is prudent for patients to discontinue all herbal and alternative medicines at least 7 days before surgery.
Even if all preventable causes of excessive surgical bleeding have been addressed preoperatively, cases of excessive bleeding will still be encountered during surgery. The surgeon should reflexively double-check that the patient position and anesthetic parameters are optimal. Care is taken not to suction blood away from raw mucosal edges, because this will promote further bleeding. Rather, saline irrigation is used to wash away excessive blood. Most of the bleeding that clouds the end of the endoscope occurs proximal to the position of the endoscope. The surgeon should actively seek such bleeding sites and coagulate these with the suction bipolar forceps to ensure that when the scope touches the side wall, accumulated blood does not run down the scope and contaminate the end. Suction instruments (such as the Freer dissector and curette) are used to ensure optimal visualization of the dissection in the bloody surgical field.
Optimize the surgical field
It is essential to reduce the amount of blood obscuring the visual field in ESS. This will allow proper visualization of the landmarks that are critically important to the safety and success of surgery. Several measures can be taken intraoperatively to reduce bleeding ; these include reverse Trendelenburg positioning, the application of topical and local vasoconstrictors, maintaining the mean arterial pressure at around 75 mm Hg and the heart rate less than 60 beats/min. This is best achieved with total intravenous anesthesia. A preoperative course of systemic steroids may also be beneficial to reduce the size and vascularity of nasal polyps, thus reducing capillary bleeding during ESS. However, the optimal dose, length of treatment, and ideal groups of patients who would benefit from this treatment require further research.
There are several patient factors that predispose to increased bleeding, and thus, a poor surgical field. These should be actively sought and, if possible, dealt with preoperatively. Local factors include acute infection, inflammatory processes including the granulomatous diseases, and excess local tissue trauma during dissection. If suspected clinically, active infection of the sinuses should be treated with an appropriate course of preoperative antibiotics. Systemic comorbidities that can increase surgical bleeding include hypertension, peripheral vascular disease, and liver and renal diseases. Chronic alcohol abuse, malnutrition, and vitamin deficiencies (most notably vitamin K), can also affect coagulation, and must be explored if suspected clinically. Bleeding diatheses such as hemophilia A or B and von Willebrand disease, require clotting factor replacement or specialized pharmacotherapy (desmopressin [DDAVP], tranexamic acid, or aminocaproic acid), and must be planned for. Medications affecting surgical field, including aspirin, nonsteroidal antiinflammatory drugs, warfarin, and antiplatelet agents, must be discontinued for an adequate length of time before surgery, in consultation with the patient’s regular treating physician. Several herbal and alternative therapies, such as ginseng, ginkgo and kava, can affect coagulation pathways, and the surgeon should be aware of these. It is prudent for patients to discontinue all herbal and alternative medicines at least 7 days before surgery.
Even if all preventable causes of excessive surgical bleeding have been addressed preoperatively, cases of excessive bleeding will still be encountered during surgery. The surgeon should reflexively double-check that the patient position and anesthetic parameters are optimal. Care is taken not to suction blood away from raw mucosal edges, because this will promote further bleeding. Rather, saline irrigation is used to wash away excessive blood. Most of the bleeding that clouds the end of the endoscope occurs proximal to the position of the endoscope. The surgeon should actively seek such bleeding sites and coagulate these with the suction bipolar forceps to ensure that when the scope touches the side wall, accumulated blood does not run down the scope and contaminate the end. Suction instruments (such as the Freer dissector and curette) are used to ensure optimal visualization of the dissection in the bloody surgical field.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


