Telemedicine for Otolaryngology
John Kokesh
Chris Patricoski
Stewart A. Ferguson
Telemedicine utilizes technology to enhance communication and provide services over a distance. In this way, “telemedicine” represents an evolution in health care that has adopted the technologies and communication infrastructure now available in society. The telephone and fax machine were the earliest telecommunication tools used in clinical practice, and are now so ubiquitous that we can hardly imagine medicine without them.
With the rapid advances in technology and telecommunications, and perhaps more importantly, widespread societal acceptance of technology, a new generation will redefine how medicine is practiced in the future. “Telemedicine” will likely become an antiquated term requiring redefinition, no longer describing a niche area in certain medical specialties but rather a methodology by which modern information transfer is used to improve the practice of medicine.
This chapter examines the current telemedicine technologies and present applications of telemedicine in otolaryngology. While telemedicine has grown significantly in the last 10 years, there is a need for further adoption throughout the United States. The realization that improvements are needed in access for care, costs of care delivery, and availability of medical specialists will likely help remove some of the barriers that have thus far thwarted widespread innovation and adoption of telemedicine in otolaryngology. The nature of the specialty, with well-developed and extensive use of endoscopy, microscopy, photographic imaging, and physiologic data, makes otolaryngology a potential beneficiary of an expanded role for telemedicine in the future practice of medicine.
DEFINITIONS
The American Telemedicine Association (ATA) defines telemedicine as “the use of medical information exchanged from one site to another via electronic communications to improve patients’ health status” (1). Telemedicine has been traditionally divided into three areas: Interactive Video Teleconferencing (VTC), Asynchronous Store-and-Forward (S&F), and Remote Patient Monitoring (RPM). While the distinction between these categories has begun to blur with advances in device technology and means of information transfer, it is worthwhile to review each as well their current usage in medicine.
The term “VTC” telemedicine applies to a medical encounter performed over a live teleconference link with video and audio and, in some instances, a live display of data from remote medical devices. As commonly practiced, a “presenting provider” is physically present with the patient to assist with the interview, conduct aspects of the examination, and operate devices to obtain parts of the examination to be transmitted. The presenting provider, for example, may operate an endoscope to provide live video of the examined body system. The “consulting provider” is located at a distance and receives the live video feed. There is synchronous communication between the providers and the patient; questions can be asked and immediately answered. The consulting provider may direct certain parts of the examination. The encounter may be recorded for future reference. Some of the advantages of VTC are that it is interactive, patient movement and affect can be assessed, and a “human” connection between the involved parties can be established. The consulting provider has the ability to conduct an interview similar to an in-person exam and can help direct the encounter. The disadvantages of VTC are that all involved parties must be available simultaneously for the encounter, technical and network support is needed to ensure full function at the time of the scheduled encounter, and sufficient bandwidth is required for adequate video quality. VTC has generally been most successful when used as part of an integrated health system where coordinated scheduling, technical support, training, and funding are provided (2). Examples of medical specialties
where VTC has been successfully used include psychiatry and mental health services, cardiology, and intensive care unit consultation (Tele-ICU) (3,4). VTC has also been used in the recent development of “telestroke” networks, where a remotely located neurologist assesses patients with evolving strokes and decides whether thrombolytic therapy should be administered (5).
where VTC has been successfully used include psychiatry and mental health services, cardiology, and intensive care unit consultation (Tele-ICU) (3,4). VTC has also been used in the recent development of “telestroke” networks, where a remotely located neurologist assesses patients with evolving strokes and decides whether thrombolytic therapy should be administered (5).
“S&F” telemedicine involves the capture, storage, and transmission of data between providers for the purpose of obtaining medical advice and opinion. As commonly practiced, the “creator” is physically present when interviewing the patient, conducting an examination, capturing data, and documenting the encounter in a telemedicine case. The “consultant” at a remote location would then review the transmitted data after it was sent in its entirety. S&F is asynchronous; the providers need not be available at the same time, and the created “case” may be viewed minutes, hours, or days after it was created and transmitted. Typical data that are captured and utilized in S&F include clinical histories, vital signs, digital photos, radiology images, endoscopic images, scanned documents, audiograms, tympanograms, and heart and lung sounds. The advantages of S&F are that it does not require simultaneous availability of providers, thereby avoiding scheduling and logistic problems. It can be extremely time efficient for the consultant as complete data collection and organization of information have occurred during creation of the case, often along predetermined guidelines (Fig. 205.1). S&F can be used with low or interrupted bandwidth, enabling its use in very remote or infrastructure-deprived locations. Finally, once set up with the appropriate software, security, and operational standards, S&F “works like e-mail” requiring much less ongoing maintenance and support than VTC. Disadvantages of S&F are that real-time interaction between providers is not possible; the consulting provider cannot direct the exam (though they can asynchronously request additional information), and sustained movement, voice, and affect of the patient cannot be assessed (though short video files are now easily transferrable). S&F has long been successfully used in those specialties where the assessment or “read” of the consultant regarding static clinical data is the valued service. Well-established examples are teleradiology (6), teledermatology (7), and telepathology (8).
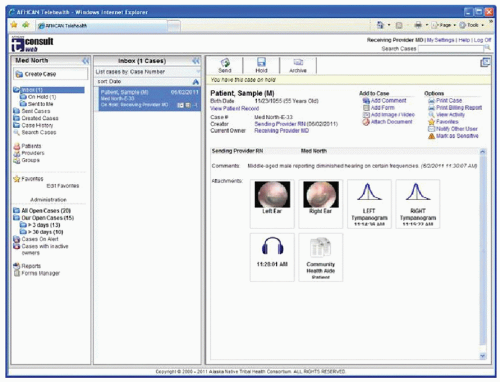 Figure 205.1 Alaska Federal Health Care Access Network (AFHCAN) tConsult software. Clinical information and data have been organized for review by the consultant. |
RMP technology enables the monitoring of patient health data originated from the patient’s home, nursing facility, place of employment, school, and other locations. It is most often employed in the patient’s home and, as such, is often called “home telehealth.” RPM almost always involves capture of data similar to S&F and sometimes includes video. To date, RPM has proven useful for the management of chronic disease states such as diabetes, congestive heart failure, and chronic pulmonary disease (9,10). Used appropriately, RPM facilitates access to care, patient and family involvement and education, and early identification and intervention for acute illness or health status decompensations. RPM holds tremendous promise for cost savings through improved chronic disease management, especially for integrated health systems (11). From a commercial standpoint, RPM represents a large potential market, and device manufacturers are rapidly adding new products to the field. For these reasons, this is the most rapidly growing field in telemedicine, and clinicians will likely have increasing opportunities to use home monitoring in the future.
A final category of telemedicine deserving mention relates to the use of telemedicine technologies in the performance of surgical procedures. In telementoring and teleproctoring, a distantly located “expert” surgeon monitors and assists a surgeon at a distant location performing a surgery. A typical current application would involve using a live VTC link used to mentor an endoscopic procedure (12). Telesurgery, the performance of a surgical procedure by a remotely located surgeon using robotic devices, is currently the subject of feasibility studies and demonstration projects (13).
SECURITY AND HIPAA
Telemedicine is no different from other forms of clinical care in regard to the applicability of regulations governing privacy and security. The use and disclosure of an individuals’ health information (protected health information [PHI]) by providers and organizations are subject to national standards and regulations—regardless of the care delivery model. Most notable among these are the so-called HIPAA Privacy and Security Rules and the more recent HITECH Act:
The Standards for Privacy of Individually Identifiable Health Information (Privacy Rule) was issued by the US Department of Health and Human Services in 2000 to implement the requirements of the Health Insurance Portability and Accountability Act of 1996 (HIPAA). The Privacy Rule standards address the use and disclosure of individuals’ health information called “protected health information” by organizations subject to the Privacy Rule (covered entities) as well as standards for individuals’ privacy rights to understand and control how their health information is used.
HIPAA also mandated the creation of national standards for the security of electronic health care information, which were then released in the final “HIPAA Security Rule” in 2003. This final rule specified a range of administrative, technical, and physical security procedures for covered entities to use to for electronic protected health information (ePHI); the standards were delineated into either required or addressable (optional) implementation specifications.
More recently, the Health Information Technology for Economic and Clinical Health Act (HITECH Act) was passed as part of the American Recovery and Reinvestment Act of 2009 (ARRA). Because HITECH contains incentives designed to accelerate the adoption of electronic health record (EHR) systems and potentially generate a massive growth in the exchange of ePHI, the HITECH Act further broadened the scope of privacy and security protections established under HIPAA.
A good “rule of thumb” is to recognize that a telehealth system should be treated no different than an EHR system in regard to privacy and security. Telehealth systems are designed to capture, transmit, store, and display ePHI— as are EHR systems. Many telehealth systems interface to EHRs and share information in a back-and-forth manner to provide a more complete view of the patient record. Telehealth systems sometimes contain information that is potentially “more identifiable” of the patient as they may contain images of the patients face or other body parts.
It is not possible to provide a thorough review of the HIPAA and HITECH regulations as they apply to telehealth systems, but the following features are recommended in any telehealth system to maximize the ability to comply with HIPPA and HITECH. While the general concepts apply to VTC, S&F, and RPM, the remainder of this section uses S&F telehealth as an example for how these standards and regulations may apply.
All data should be encrypted “at rest” and during “transport.” Data flow (i.e., “transport”) in a telehealth system from a computer (or system) in the patient exam room to other systems where remote providers (or specialists) can view the data. Data may stay on a server (at rest) or a desktop PC for hours or days until a provider can view that data. Data that are encrypted are not “readable” or “viewable” without the right key to “decrypt” the data. This prevents unauthorized users from accessing the data and provides a significant level of privacy and security protection. While some organizations elect to not encrypt data flowing within their private network, telehealth services are becoming much more common between organizations with data flowing outside of organizational networks and potentially across Internet links, further accentuating the need to encrypt the data.
Access to data through a browser—such as Internet Explorer or Safari—should rely on an encrypted connection (e.g., “https” instead of “http”). When this access
occurs across the Internet or outside of an organization’s trusted network, the Web site should provide “https” connectivity using a security certificate from a trusted organization—thereby allowing users to have greater trust in the web server’s authenticity.
Systems that require data to move between organizations or across nonsecure networks should include a mechanism to make sure the data do not change (data validation) and a mechanism to verify the site or provider that originated the data (nonrepudiation). This is usually accomplished through electronic signatures and “hash” algorithms.
The telehealth system should integrate with the user authentication mechanism used by the organization, so the user account can be managed through a central mechanism and password policies can be enforced (e.g., regular changes, minimum password length, and complexity).
All major user activities should be tracked within the telehealth system through an audit mechanism. As a minimum, all successful and unsuccessful log-in attempts should be logged as well as any changes that impact patient data.
Users should have sufficient access for their needs, but no more. Role-based security is an excellent mechanism whereby users are assigned to various roles (e.g., consultant, trainer, clinical administrator) that define their access to telehealth data and functionality. Time-outs should be employed to limit access to data should a provider leave a workstation prior to logging out.
Recognizing that not all telehealth cases are necessarily equal, the telehealth system should provide a mechanism to indicate when a case is “sensitive” or requires tighter security than other cases. Such cases might include abuse cases, mental health cases, or HIV/AIDS cases.
Similar to EHR systems, telehealth equipment (workstations, servers, medical devices) can all contain ePHI and as such need to be physically secured to prevent loss of data due to theft or unauthorized access.
The telehealth system needs to be managed and protected similar to an EHR system. This would include, for example, accepting updates only when tested and provided by a reputable source, backing up data and providing for disaster recovery efforts, active defenses against viruses and other malware, and protecting equipment against loss of power or intermittent power surges.
It is not uncommon to find providers that rely on e-mail as a simple telehealth solution—allowing for the exchange of images and basic textual information about a patient. This should raise significant concern based on the proceeding information, as an e-mail system is often not considered a secure system by most organizations and will limit or impede and organization’s ability to achieve HIPAA compliance.
USES OF TELEMEDICINE IN OTOLARYNGOLOGY
Telemedicine has been used in the field of otolaryngology since the early 1990s. Use has occurred primarily in those situations where there was a remote, isolated population to serve; a shortage or lack of availability of otolaryngologist; or, more recently, backlogs of patients needing otolaryngology care inadequately addressed by the existing delivery system. Applications have been partially driven by available technologies and their cost, and the spectrum of clinical services that can be delivered at a distance has increased with advances in technology and communication infrastructure. Finally, most of the usage and research in the use of telemedicine in otolaryngology has occurred in those settings where the financial and regulatory barriers that have limited the widespread use of telemedicine in the United States are less formidable and where telemedicine programs have been designed to meet a specific clinical or population need. Examples include programs run through the United States Department of Defense and the United States Public Health Service as well as programs in countries with national health plans.
Otology and Neurotology
The ability to obtain and transmit diagnostic quality images of the tympanic membrane and middle ear has been well established. Pedersen, in pioneering work done in Norway, showed that a video otoscope coupled to a VTC network could be used to allow a remotely located otolaryngologist to direct patient examinations and establish diagnoses and treatment plans. This resulted in improved access for otolaryngology care as well as reduced cost for care delivery to isolated populations (14). Additional work using this methodology has verified that high-quality images can be routinely obtained with the video endoscope, even in pediatric populations (15). Still images of tympanic membrane obtained by a video otoscope and accompanied by audiologic and tympanometric data and transmitted using S&F technology were used to deliver otology consultations to patients in remote areas of Western Australia (16). Exam findings and diagnoses based on S&F examination using digital images from a video otoscope for children with previously placed tympanostomy tubes were found to correlate highly with those established by in-person encounters with otolaryngologists using binocular operating microscopes (17). S&F telemedicine using tympanic membrane images, clinical histories, and audiologic data has been shown to allow for accurate planning for chronic ear surgery (18).
This work has demonstrated that telemedicine, whether VTC or S&F, is a useful tool for delivering otology care. As diagnosis depends to a great degree on the physical characteristics of the tympanic membrane, image quality is critically important. Images must be in focus, adequately
illuminated, and free of obstruction. A high-performing video otoscope proves to be a worthwhile investment, and training must be provided to those acquiring the images to ensure consistent high quality. While most video otoscopes do allow for insufflation, and tympanic membrane mobility can be assessed if VTC is used, the addition of tympanometric data has generally found to be a useful adjunct to images. When “packaged” with digitized clinical histories and audiograms, an otology “case” can be created that can be reviewed by the otolaryngologist and in most cases lead to an accurate diagnosis and treatment plan (Fig. 205.2). When used over an S&F platform and coupled with clinical guidelines and standards for the information required by the consultant, telemedicine can become an extraordinarily efficient way to diagnosis, triage, and offer treatment advice for otologic disease.
illuminated, and free of obstruction. A high-performing video otoscope proves to be a worthwhile investment, and training must be provided to those acquiring the images to ensure consistent high quality. While most video otoscopes do allow for insufflation, and tympanic membrane mobility can be assessed if VTC is used, the addition of tympanometric data has generally found to be a useful adjunct to images. When “packaged” with digitized clinical histories and audiograms, an otology “case” can be created that can be reviewed by the otolaryngologist and in most cases lead to an accurate diagnosis and treatment plan (Fig. 205.2). When used over an S&F platform and coupled with clinical guidelines and standards for the information required by the consultant, telemedicine can become an extraordinarily efficient way to diagnosis, triage, and offer treatment advice for otologic disease.
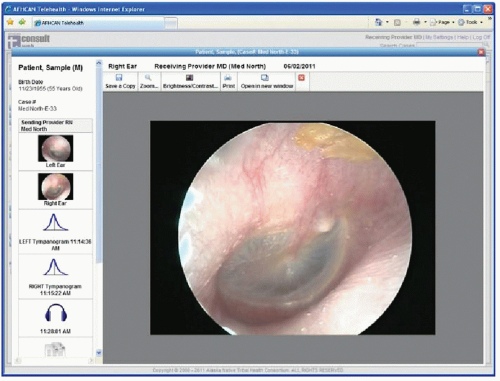 Figure 205.2 Typical otology case in AFHCAN tConsult software. Case includes images, audiogram, tympanogram, and clinical history. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


