Surgical Treatment for Benign Paroxysmal Positional Vertigo
Richard R. Gacek
Mark R. Gacek
Michael J. McKenna
Benign paroxysmal positional vertigo (BPPV) is a disorder of the peripheral vestibular end organ that results in brief but severe bouts of vertigo that are precipitated by change in head position. Although in most cases this is a self-limiting condition lasting from weeks to months, in a small percentage of patients the clinical course may be protracted and not resolve with time or physical therapy. Under such circumstances and when the disorder becomes psychologically or physically incapacitating, surgical intervention may be considered. Until recently, the best and most discriminating surgical approach has been selective posterior ampullary nerve section by a transcanal approach. However, over the past decade another surgical option for the management of BPPV has emerged, the transmastoid occlusion of the posterior semicircular canal. These two techniques have different physiologic effects on the peripheral vestibular system and result in similar rates of success.
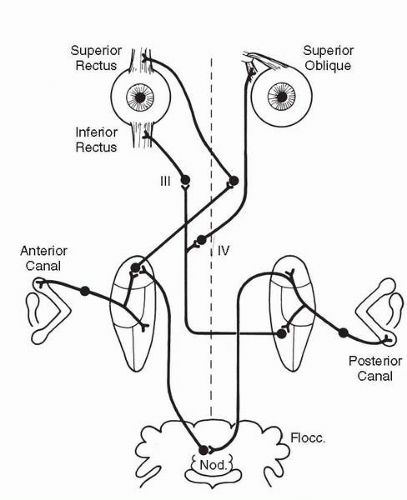
When first described by Barany (1), benign paroxysmal positional vertigo was thought to be a disorder of the otolithic system, specifically the utricular macula. However, the brisk transient rotatory nystagmus produced by the provocative positioning maneuver (Hallpike) cast doubt on a purely otolithic mechanism (2). A reasonable hypothesis supported by human temporal bone histopathology is that the cupula of the posterior semicircular canal is transformed into a gravity-sensitive receptor by the deposition of high specific gravity deposits onto the cupula or floating in the endolymph of the canal (3) (Fig. 31.1). The canal sense organ is then excited by gravitational forces when the characteristic ear-down or head-back position is assumed (Fig. 31.2). Selective surgical denervation or ablation of the posterior canal function has been shown to relieve the subjective symptoms and objective nystagmus of the disorder (4,5), thus affirming that the posterior semicircular canal sense organ is responsible for BPPV. Similarly, disruption of endolymph flow by mechanical occlusion of the posterior semicircular canal results in similar findings, adding further evidence that the symptoms associated with BPPV originate from the posterior canal ampulla. What is not clear at present is the exact pathophysiologic mechanism that results in the symptoms of BPPV. Features of this disorder that are not explained on a purely mechanical basis are the limited duration of the ocular response despite maintaining the provocative position and its fatigability on repeat provocation (3). Recent observations in temporal bone specimens of patients with BPPV reveal focal degeneration of axons in the inferior vestibular division (6,7). This suggests that there may be a neural component to the pathophysiology of BPPV that may account for these features that provoke the vestibuloocular response. Evidence of a primary mechanical etiology includes the observation of pathologic deposits within the cupula of the ampulla of the posterior canal in temporal bone specimens from patients with BPPV (3), evidence of free-floating particles within the endolymph of the posterior semicircular canal that are gravity sensitive and have been observed at the time of posterior canal occlusion (8,9), and the clinical observation that a high percentage of patients with acute BPPV can be cured of their symptoms by a particle repositioning maneuver designed to redistribute free-floating particles within the posterior canal.
The fact that some cases of BPPV have evidence of axonal degeneration on postmortem examination and the clinical observation that the majority of cases result from a stressful precipitating event such as trauma, upper respiratory tract infection, and surgery on other parts of the body are highly suggestive of a viral etiology as is suspected in Bell’s palsy and vestibular neuritis.
SIGNS AND SYMPTOMS OF BENIGN PAROXYSMAL POSITIONAL VERTIGO
Patients with BPPV complain of a rotatory experience accompanied by nausea when the head is placed in the head-back or ear-down position (10). The vertigo and nystagmus typically have a 1- to 4-second latency and duration of 20 to 25 seconds. Repeat positioning results in decreased signs and symptoms.
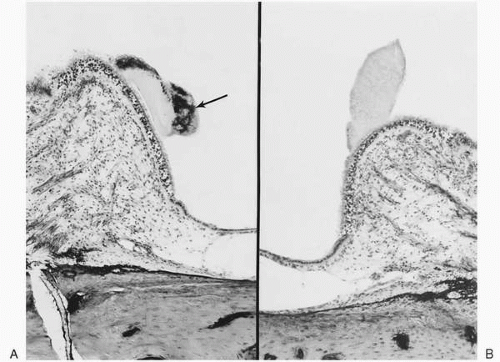 FIG. 31.1 A: Basophilic deposit (arrow) embedded in the posterior canal cupula of the symptomatic ear of a patient with BPPV. B: Contralateral posterior canal crista of patient in A. |
The Hallpike maneuver on the patient fitted with Frenzel’s glasses is used to reproduce nystagmus and symptoms of BPPV (2). In severe cases of BPPV, the nystagmus can be observed without suppression of visual fixation. The direction of nystagmus is usually rotatory in a counterclockwise direction with the right ear down and clockwise with the left ear down. This type of nystagmus is the result of the vestibuloocular projections from the posterior semicircular canal (Fig. 31.3). Occasionally, a horizontal nystagmus may be observed with the same latency, duration, and fatigability as is seen with the rotatory nystagmus (11). The responsible sense organ in this instance is thought to be the lateral semicircular canal crista. Another group of patients experience balance symptoms, not typically paroxysmal positional vertigo, resulting from incomplete ablation of labyrinthine function attempted either by transcanal labyrinthectomy or vestibular nerve transection. Because the posterior canal sense organ and its nerve supply are anatomically inaccessible in these procedures, they may escape ablation. This residual function of the posterior canal sense organ may be responsible for persistent symptoms following vestibular ablation procedures. In these patients, transection of the singular nerve can be performed to provide relief of their symptoms.
PATIENT SELECTION
Because most patients with BPPV undergo spontaneous resolution within a 6- to 12-month period or may be only mildly disabled by their symptoms, surgical treatment is not often employed (6). Exercise programs that use the head and neck and upper trunk muscles may be helpful to reduce the severity of symptomatology and promoting spontaneous resolution (12). Repositioning maneuvers intended to redistribute high density particles in the endolymph of the posterior canal are also effective to relieve symptoms, particularly in acute BPPV (13,14). However, for a small group of patients who demonstrate chronic positional vertigo for more than 1 year despite conservative measures and are sufficiently disabled from their normal activities, singular neurectomy or transmastoid posterior canal occlusion provide an effective means of relief from the disabling symptoms (4,5,7,15, 16, 17). Some patients with chronic BPPV continue to live with their symptoms by avoiding the provocative position and changing their lifestyle. Surgical relief is offered only to those who request it and are willing to accept the low risk of hearing loss.
PREOPERATIVE EXAMINATION
The evaluation and diagnosis of BPPV consist of an accurately obtained history documenting labyrinthine trauma, such as head injury; viral labyrinthitis; inner ear or general surgery; or aging. Tests of auditory and vestibular function are essential. Most patients with this syndrome are middle age (mean age in the sixth decade). There is a 2:1 female predominance. Most patients have a normal ear examination, although occasionally a patient with chronic middle ear inflammatory disease experiences BPPV. Patients with chronic inflammatory disease should undergo attempted surgical eradication of the disease in an effort to control the vestibular symptoms. The functional evaluation consists of pure-tone and speech audiometry, as well as electronystagmographic assessment of the vestibular sensitivity by the caloric method. Auditory brainstem response and electrocochleographic examinations are not necessary in the evaluation of patients with this disorder. The most important diagnostic test is the Hallpike maneuver, properly performed with or without Frenzel’s glasses with the patient on an examining table (Fig. 31.4). The test has been well described in the literature (2) and consists of the examiner taking the patient to a head-handing position, first right and then left, from the sitting position and observing the patient’s ocular response, along with his or her subjective vestibular experience. Posterior canal BPPV typically produces a rotatory nystagmus either clockwise or counterclockwise after a latency of a few seconds. The nystagmus builds to a crescendo and then disappears over 25 to 30 seconds but reappears in reverse direction when the sitting position is again assumed. Repeat testing produces less nystagmus and fewer subjective
symptoms, supporting the peripheral location of the pathology (fatigability). It is important to test both right and left head-down positions because approximately 15% to 18% of patients with BPPV have bilateral disease that is usually worse in one ear (18). In patients with BPPV, nystagmus response is not seen when the contralateral (noninvolved) ear is placed geotropically because the gravity-sensitive cupula is deflected utriculopetally (opposite to hair cell polarization). When the involved ear is geotropic, cupula deflection is utriculofugal and in the direction of hair cell polarization, thereby causing depolarization (Fig. 31.2). Occasionally, the Hallpike test may reveal a horizontal nystagmus with the same time characteristics and fatigability observed with the rotatory nystagmus (11). These patients are not candidates for singular neurectomy or posterior canal occlusion because their symptoms may be caused by pathology in other labyrinthine sense organs, such as the lateral canal crista.
symptoms, supporting the peripheral location of the pathology (fatigability). It is important to test both right and left head-down positions because approximately 15% to 18% of patients with BPPV have bilateral disease that is usually worse in one ear (18). In patients with BPPV, nystagmus response is not seen when the contralateral (noninvolved) ear is placed geotropically because the gravity-sensitive cupula is deflected utriculopetally (opposite to hair cell polarization). When the involved ear is geotropic, cupula deflection is utriculofugal and in the direction of hair cell polarization, thereby causing depolarization (Fig. 31.2). Occasionally, the Hallpike test may reveal a horizontal nystagmus with the same time characteristics and fatigability observed with the rotatory nystagmus (11). These patients are not candidates for singular neurectomy or posterior canal occlusion because their symptoms may be caused by pathology in other labyrinthine sense organs, such as the lateral canal crista.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree