Vestibular schwannomas are benign tumors that usually originate from the balance portion of cranial nerve VIII. The treatment options currently available for vestibular schwannomas include observation with serial imaging, stereotactic radiation, and microsurgical removal. Although the ultimate goal in treatment of vestibular schwannomas is preservation of life, the best option for each patient depends on symptoms, tumor size, tumor location, and the patient’s general health and age. Surgical exposure of the cerebellopontine angle for removal of vestibular schwannomas can be performed safely via a translabyrinthine, retrosigmoid, and middle fossa approach. Each approach has its advantages and disadvantages. The goal of surgery is complete eradication of tumor with preservation of hearing and facial nerve function when possible.
Vestibular schwannomas (VS) are benign tumors of Schwann cells that originate on the vestibular portion of the eighth cranial nerve. Found in the internal auditory canal (IAC) and cerebellopontine angle, VS account for nearly 6% of intracranial tumors. Although surgical excision previously had high mortality rates, the advent of the operating microscope and neurotologic and neurologic monitoring has allowed surgical techniques to evolve and morbidity and mortality to be reduced significantly. Currently, complete surgical excision with preservation of facial nerve function is often an achievable goal. The increasing sensitivity of MRI has allowed for diagnosis of smaller tumors and has increased the ability to preserve hearing. Three basic surgical approaches are used for removal of VS: the translabyrinthine, retrosigmoid, and middle cranial fossa (MCF) approaches, which are described in this article. Although many factors influence the choice of surgical approach, personal experience of the surgeon often determines the surgical approach. This article presents the different approaches, their advantages and disadvantages, common complications, and mechanisms to prevent complications.
Surgical history
The first documented case of VS was an autopsy report during the late eighteenth century by Eduard Sandifort . It was nearly 100 years later when Thomas Annandale performed the first complete surgical excision with patient survival. Surgical excision had high mortality rates—in excess of 50%—until the early 1920s, when Harvey Cushing refined techniques and lowered mortality rates to 21% . Cushing’s protégé, Walter Dandy, further lowered mortality rates to 10% by the early 1940s .
The modern era of tumor dissection began in the early 1960s with the introduction of the operating microscope and the introduction of the translabyrinthine and MCF approaches by William House. Sterile technique, microscopic magnification, and precise otologic drills have continued to lower mortality rates to approximately 1%. Continued earlier diagnosis with the advent of MRI with gadolinium has changed the goals of surgery from complete excision and survival to maintenance of facial nerve function and preservation of hearing when possible .
Treatment options
After proper diagnosis, four treatment options are available for VS: observation, stereotactic radiation therapy, complete surgical excision, and subtotal resection with planned radiation therapy.
Observation
The indolent nature of VS has led many physicians to observe tumors that may remain dormant or grow slowly enough to never require treatment. Treatment decisions may be based on patient characteristics, such as age, general health, status of hearing in the contralateral ear, and patient preference, or tumor characteristics, such as size, location, and growth rate . Observation is performed via a set schedule of MRI. We scan our patients initially at 6 months and then every year until a general growth rate can be established. If minimal growth has been observed, the MRI every 2 years is possible.
The natural history of VS is enigmatic. The percentage of tumors that grow is generally unknown and has varied widely in studies from 40% to 80% . A long-term follow-up of 14 years in more than 1800 patients with observed acoustic neuroma was published recently in which 83% of intrameatal tumors remained intrameatal and 70% of extrameatal tumors did not grow more than 2 mm . All tumors that exhibited growth did so in the first 4 years and maintained consistent growth rates throughout observation . Tumor growth rates can be stratified into slow growing (<2 mm/y) and fast growing (>2 mm/y). Tumors with slower growth rates often do not require treatment .
There are difficulties with observation. First, MRI is expensive and patients may be lost to follow-up. Rarely, tumors may undergo accelerated rates of growth after multiple years of stable growth. Patients who require surgery after observation also are older and may suffer from more comorbidities, which makes surgery potentially more risky. Finally, tumors with continued growth may no longer meet criteria for hearing preservation approaches or radiation therapy and may make facial nerve preservation more difficult.
Advantages to observation are the obvious delay and potential elimination of the need for surgical or radiosurgical intervention. Older patients may develop or have exacerbation of existing disease that may take precedence over treatment of the tumor (ie, cancer, stroke, cardiac disease). Younger patients may choose to observe the tumor to determine growth and choose intervention only when growth has been established. Economic reasons, such as retirement, job changes, or insurance issues, may compel a patient to choose observation as an initial option. Family issues, such as a wife/husband or child with an illness or other family issues (child starting school/college), also may compel a patient to choose observation.
Radiation therapy
A complete discussion of radiation therapy or surgery is beyond the scope of this article and is covered elsewhere in this issue. Although surgical resection has the goal of complete tumor removal, radiation therapy has the primary goal of tumor control. Leksell performed the first stereotactic radiosurgery for VS in 1969. Techniques have evolved and outcomes with fewer side effects are currently possible. Although most tumors are controlled successfully, nearly 9% of tumors exhibit growth after radiation therapy. Surgery after failed radiation therapy is more difficult to perform because intense scarring and fibrosis obscure surgical planes. As a result, facial nerve outcomes are poorer than in patients with nonirradiated tumors . Because VS are known to be slow growing, it is difficult to study techniques (radiation therapy) that slow or eliminate tumor growth. Long-term studies are needed to determine the effectiveness of radiation therapy over observation and surgery to treat VS.
Surgery
The goal of surgery is complete tumor removal while preserving neurologic function and hearing, if possible. Each of the three main approaches for surgical removal of VS has advantages and disadvantages ( Table 1 ). The retrosigmoid and MFC are the two surgical techniques most commonly used in VS surgery when attempting to preserve hearing. Hearing preservation may be attempted when the pure-tone average is 50 dB or less and the speech discrimination is more than 70%. Tumor size also determines whether hearing preservation is attempted, because a tumor ≥2 cm is rarely amenable to hearing preservation despite initial hearing status. Location also may play a role in hearing preservation because tumors far lateral in the IAC with extension into the cochlea or vestibule may not be amenable to hearing preservation.
| Translabyrinthine | Middle fossa | Retrosigmoid | |
|---|---|---|---|
| Advantages |
|
|
|
| Disadvantages |
|
|
|
All procedures are performed under general anesthesia with neurophysiologic monitoring. Facial EMG electrodes are inserted into the obicularis oris and occuli muscles for continuous facial nerve monitoring. Auditory brainstem response is used in hearing preservation cases with an acoustic ear insert in the external auditory canal, a recording electrode placed at C0 on the vertex, a reference in the ipsilateral ear lobule, and a ground in the shoulder. Perioperative antibiotics and steroids are used. Mannitol (1 g/kg) is given just before opening the dura in all cases.
The translabyrinthine approach provides wide access to the posterior fossa with little or no need for brain retraction. The anatomy is familiar for the neurotologist but often is unfamiliar to the neurosurgeon. The facial nerve is identified early in the case laterally at the fundus of the internal IAC and medially at the brainstem. This lateral surgical approach allows for the facial nerve to be in a favorable place deep in the IAC and places the vestibular nerves laterally, where the surgeon encounters the vestibular nerves initially on IAC dissection. The main disadvantage of this approach is the lack of ability to preserve hearing.
The MFC approach was seldom used for tumors until recently because most tumors remained undiagnosed until they were too large to be removed by MCF. Its popularity has increased recently as imaging technology has allowed for detection of small tumors and tumors with up to 1 cm in the cerebellopontine angle are amenable to this technique. Although this approach has the most favorable hearing preservation rates, the technique is challenging because the facial nerve lies between the surgeon and the tumor and the principal anatomic landmarks for identification of the IAC are less reliable and may be obscured. The superior approach to the IAC makes the facial nerve and the superior nerve the first encountered by the surgeon on dissection through the temporal bone. Elevation and retraction of the temporal lobe also carry the risk of brain injury, including aphasia, seizures, and stroke.
The retrosigmoid approach traditionally has been the most widely used approach because of its popularity among neurosurgeons and its wide versatility. It affords wide exposure of the posterior fossa, can be used for excision of small and large tumors, and offers an opportunity for hearing preservation. Intradural drilling of the IAC is required. Like the translabyrinthine approach, lateral surgical approach allows for the facial nerve to be in a favorable position deep in the IAC and places the vestibular nerves laterally, where the surgeon encounters the vestibular nerves initially on IAC dissection.
Surgical approaches
Retrosigmoid approach
The patient is positioned in a modified park bench position, lying supine with the ipsilateral shoulder and hip bumped with rolls and padding. The patient’s head is flexed and rotated toward the opposite shoulder and secured with Mayfield pinions. This simple and straightforward position enables excellent visualization of the contents of the posterior fossa. Extreme rotation and flexion may cause venous occlusion and should be avoided. Somatosensory evoked potentials are monitored throughout the case. Potential changes in the waveforms may indicate compromise of the vascular system or spinal compression. Hair is prepped with betadine solution and shaved for four finger breadths behind the ear.
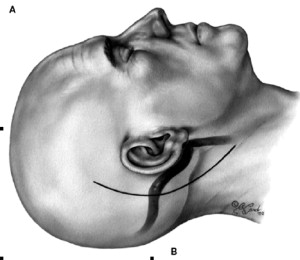
As shown in Fig. 1 , a curvilinear “C” incision is made into the posterior scalp down onto the neck. The incision is approximately 4 cm posterior to the ear canal. The incision is carried through the skin and subcutaneous tissues and an anterior flap is dissected for nearly 1 cm. Electrocautery is used to incise the musculoperiosteum down to the bone. Offset incisions allow for overlapped closure and a reduced incidence of incisional cerebrospinal fluid (CSF) leaks.
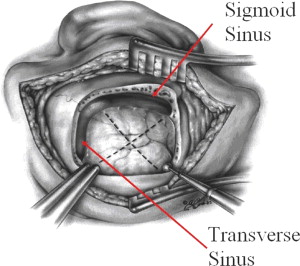
As shown in Fig. 2 , a 4 × 4 cm craniectomy is performed. The anterior and superior limits of the craniotomy are the sigmoid and transverse sinuses, respectively. As a general rule, the external ear canal approximates the level of the transverse sinus. Laterally exposed mastoid air cells near the sigmoid sinus are occluded with bone wax to prevent transgression of CSF at initial opening and again at the end of the case. The dura is then opened, as shown along the dashed lines in Fig. 2 , and the dural flaps are reflected laterally and secured with sutures. The dural flaps are routinely irrigated throughout the case to avoid desiccation. Moist cottonoid pledgets are placed over the cerebellum to avoid intraoperative injury and prevent desiccation throughout the case. The cisterna magna is opened anteroinferiorly to the cerebellum with a right angle pick to allow CSF egression, which maximizes posterior fossa relaxation and minimizes the need to retract the cerebellum during the case.
The tumor and the seventh to eighth nerve complexes are identified at the brainstem and dissection is performed in a cooperative fashion between the neurosurgeon and neuro-otologist. The lateral surface of the tumor is examined for a rare lateral displacement of the facial nerve or major vascular structure. Visual inspection of the IAC is often difficult until large tumors are internally debulked. If still difficult to visualize, the IAC can be palpated with blunt instrumentation. The dura above the IAC is coagulated with bipolar cautery in an arc several centimeters above the posterior lip of the IAC before making a similar incision. The dura is then elevated down to the porus acousticus of the IAC and reflected over the tumor. Several cotton balls are placed medially to the IAC to prevent bone dust from accumulating in the cerebellopontine angle.
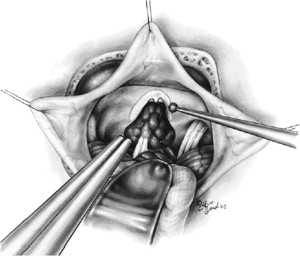
Dissection begins with an otologic drill and medium-sized cutting burs until the IAC is approached. Diamond burs are then used to create superior and inferior troughs closer to the IAC until nearly 180° to 270° of bone is removed around the posterior IAC ( Fig. 3 ). Exposure of the IAC continues laterally until the IAC appears normal and the end of the tumor is encountered. For hearing preservation to be accomplished, the common crus of the bony labyrinth and the vestibule must not be injured during dissection. Drilling continues until a thin layer of bone remains over the IAC dura. This bone is removed with careful dissection and the IAC dura is then opened. It is preferred to gain exposure of the IAC lateral to the tumor before opening the dura. Keeping the dura intact provides a protective layer to the contents of the IAC during drilling. Opening the dura too early requires further drilling laterally to gain tumor control with an open IAC. The superior vestibular nerve, inferior vestibular nerve, and tumor are identified in the posterior aspect of the canal. Gentle retraction of the superior vestibular nerve reveals the facial nerve, which is identified physiologically with a stimulator at minimal settings (0.05 mA). The vestibular nerves are sectioned laterally, and tumor dissection is performed in the plane between the tumor and the facial and cochlear nerves in a lateral to medial fashion. Endoscopic assistance with a 30° endoscope also may be valuable to inspect the lateral IAC and reduce the risk of residual disease.
Once the tumor dissection is complete, the operative field is copiously irrigated and hemostasis is achieved with bipolar cautery. The entire bone surrounding the IAC is sealed with bone wax applied with a cotton pledget. Gelfoam is then placed over the remaining seventh and eighth nerve complex and fibrin glue is used to reinforce the seal of the IAC. The dura is then closed with running 3-0 nylon closure. Fibrin glue is placed over the closure of dura. The subcutaneous tissues and skin are closed in several layers with absorbable 2-0 and 3-0 vicryl sutures and staples are placed in the skin. A compressive dressing is placed over the wound to apply pressure in the postoperative period. The patient is kept in the neurointensive care unit for 24 to 48 hours and kept on steroids and antibiotics.
Translabyrinthine approach
The patient is placed in the supine position and the head is turned away from the operative side. The initial positioning is much simpler with this approach than with the retrosigmoid approach—no pins, head holders, or park bench positioning is required. The hair is prepped with betadine solution and four fingerbreadths of hair are shaved above and behind the auricle. As shown in Fig. 4 , a C-shaped incision is made extending from one finger breadth above the ear and two finger breadths behind the postauricular crease down to one finger breadth posteroinferiorly to the mastoid tip. The incision is made through the skin and a skin flap is elevated for 1 cm toward the ear through the entire incision. The stepped incision allows for easier closure and prevention of CSF leak. A large superficial temporal fascial graft is harvested and placed on a block. As shown in Fig. 4 , a C-shaped musculoperiosteal incision is made with electrocautery from just above the temporal line to the mastoid tip. This incision is offset from the cutaneous incision by 1 cm throughout the incision. The periosteum is elevated to the external auditory canal and retracted with dura hooks. Several large pieces of digastric or sternocleidomastoid muscle are harvested for later use in packing the middle ear.

The bony exposure is performed in three stages: complete mastoidectomy, labyrinthectomy, and IAC dissection. Most of the drilling is performed with cutting burs; however, diamond burs are used when dissection is around critical areas. A complete mastoidectomy is performed, skeletonizing the bone overlying the sigmoid sinus and the tegmen. As shown in Fig. 5 , the facial nerve is identified throughout its mastoid course with a large diamond bur. In previous reports the facial recess was opened, the incudostapedial joint was separated, and the incus was removed. Currently, the senior author does not open the recess or remove the incus unless needed for exposure, leaving less exposed area to seal from CSF leak. All bone is removed from the middle fossa dura, sinodural angle, sigmoid sinus, and posterior fossa down to the level of the labyrinth. Nearly 1 cm of bone is also removed from the posterior fossa dura behind the sigmoid to allow for sinus retraction if necessary.
A complete labyrinthectomy is performed using a diamond bur after the labyrinth is skeletonized and the jugular bulb is identified. The three semicircular canals are removed starting with the horizontal canal. The posterior canal is then opened from its midportion to the common crus. The superior canal is removed and the inferior portion of the posterior canal is removed. The vestibule is opened widely.
Bone from the inferior, posterior, and superior aspects of the IAC is removed with diamond burs. The orientation of the IAC is roughly parallel to the external auditory canal. All bone surrounding the IAC is skeletonized to an eggshell thickness from the middle and posterior fossa dura onto the IAC before removing any bone or opening the dura. The inferior border of the IAC is skeletonized before the superior as the facial nerve is in the superior IAC. The fundus of the canal is exposed just medial to the vestibule, and the transverse crest that separates the vestibular nerves is identified.
The dura of the IAC is then sharply opened. The transverse and vertical crests in the lateral aspects of the IAC are identified with a right angle pick. The superior vestibular nerve is gently displaced while palpating the vertical crest or “Bill’s bar” to allow visualization of the facial nerve, which is confirmed electrophysiologically with stimulation at minimal settings (0.05 mA) ( Fig. 6 ). A small right angle hook is used to avulse the superior vestibular nerve laterally and expose the facial nerve. The inferior vestibular nerve and cochlear nerves are then separated laterally. The contents of the IAC are dissected from the facial nerve in a lateral to medial fashion. The posterior and middle fossa dura surrounding the IAC is opened for visualization of the cerebellum, brainstem, and cerebellopontine angle component of the tumor. Internal debulking of the tumor is performed with ultrasonic aspiration or a laser to allow for infolding of the tumor and dissection away from the facial nerve and brainstem. The remainder of the tumor is dissected from the facial nerve and brainstem until completely removed.
The surgical field is then copiously irrigated. Meticulous attention to closure is important for preventing CSF leak. The packing of the eustachian tube orifice and the middle ear is important in that regard. The bone of the promontory is abraded with a small right angle pick and the middle ear, vestibule, and eustachian tube are occluded with previously harvested muscle. The fascia graft is then used to cover the antrum. No attempt at primary reconstruction of the opened posterior fossa dura is performed at our institution because it is removed at initial opening. Abdominal fat is cut into strips and used to pack the mastoid defect down to the level of the IAC. The mastoid periosteum is then closed with interrupted 2-0 vicryl sutures. The skin is closed watertight with 3-0 vicryl sutures and staples externally. A compressive dressing is placed on the incision.
Middle fossa approach
The patient is placed in a supine position with the head turned to expose the ear of interest. The hair is prepped with betadine solution and four fingerbreadths of hair are shaved above the auricle. The patient is then prepped and draped in the usual fashion. Unlike other surgeries, the surgeon sits at the head of the bed. Although some surgeons prefer a vertical incision through the skin, a broad, posteriorly based, U-shaped skin flap is designed. The anterior aspect of the incision should be left posterior to the natural hairline to camouflage the scar. As shown in Fig. 7 , an anteriorly based U-shaped incision is made through the musculoperiosteal layer to skull after the entire skin flap is elevated posteriorly. A Lempert elevator is used to elevate the periosteum to the anterior limit of the incision.
Careful palpation with blunt instrumentation allows identification of the external auditory canal. A 4 × 4 cm craniotomy is performed with the opening roughly two-thirds anterior to the external auditory canal and one-third posterior. A 4-mm cutting bur is used for most bone removal, but a diamond bur is used to remove the last layers of bone over the dura. The bone flap is dissected free from the underlying dura and preserved for reconstruction at the end of the case. The bone inferior to the craniotomy is removed down to the level of the external auditory canal.
Using the microscope and a freer elevator, the middle fossa dura is then elevated off the temporal bone medially to the petrous ridge. Dissection proceeds in a posterior to anterior direction to avoid trauma to the geniculate ganglion and greater superficial petrosal nerve, which may be dehiscent in up to 15% of patients. Anteriorly, dissection stops short of the foramen spinosum and middle meningeal artery.
As shown in Fig. 8 , a House-Urban retractor facilitates retraction after dural elevation. Pressure from CSF is relieved with hyperventilation to lower p co 2 and mannitol. The temporal floor is inspected for clues to identifying the IAC, including the arcuate eminence overlying the superior semicircular canal, the greater superficial petrosal nerve, and the external auditory canal. The semicircular canal is blue-lined in an anterolateral direction to expose the lateral extent of the canal near the IAC.




