43
Submacular Surgery
Nancy Holekamp
INTRODUCTION
ubmacular surgery evolved during the 1990s in an attempt to offer patients with subfoveal choroidal neovascularization (CNV) an alternative treatment to observation or laser photocoagulation. With the advent of intravitreal anti-vascular endothelial growth factor (anti-VEGF) injections for the treatment of CNV, submacular surgery is rarely used. Nevertheless, the surgical techniques of submacular surgery have refined and they are now an established part of the vitreoretinal surgeon’s armamentarium. Submacular surgical techniques can be used to access the subretinal space to remove many types of CNV: subfoveal, juxtafoveal, extrafoveal, peripapillary, occult, and hemorrhagic. They can also be used to address other subretinal pathology such as fibrosis, parasites, and intraocular foreign bodies. The surgical techniques and their application in the treatment of submacular CNV are discussed in this chapter.
SURGICAL TECHNIQUE
Submacular surgery begins with a standard 20-gauge three-port pars plana vitrectomy (PPV). The trocars used in small-gauge transconjunctival sutureless vitrectomy surgery do not allow the angled instruments required for submacular surgery. According to the surgeon’s preference, a combination of 20-gauge and small-gauge vitrectomy may be used. The locations of the right- and left-handed sclerotomies are chosen to provide comfortable access to submacular pathology. It is helpful to have a preoperative angiogram available when choosing sclerotomy sites in cases of CNV. A sclerotomy site should provide straight line access to the retinotomy site and thus to the underlying subretinal pathology. In selective cases, it may be helpful to rotate away from the conventional 12’ o clock surgeon’s position so that direct access avoids previous laser scars, the papillomacular bundle, and the optic nerve (1).
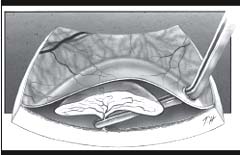
After a core vitrectomy, the posterior hyaloid membrane is stripped from the retinal surface out to the equator in eyes without a posterior vitreous detachment (PVD). This may be accomplished with a vitrectomy probe or soft-tipped silicone cannula using active aspiration (2) over the optic nerve (Fig. 43-1) or with a 130-degree angled flat-tipped pick, a “hyaloid lifter” (3) (Fig. 43-2). Triamcinolone acetonide (TA) may also be used as an adjunct to vitrectomy to visualize the posterior vitreous cortex and assist with surgical separation of posterior hyaloid from retina (4). A Weiss ring should be seen to confirm the surgical PVD. This step is necessary because macular retinotomies are not treated with laser photocoagulation.
After a peripheral vitrectomy, the retinotomy site is chosen. Its location should provide straight line access to the subretinal pathology from the dominant-hand sclerotomy, avoid major vessels and be as far away from the foveal center but still within reaching distance of the submacular CNV. Small retinotomies near the papillomacular bundle do not cause postoperative visual-field loss (5). Therefore, a right handed surgeon operating on a left eye can use a retinotomy superior nasal to the fovea for subfoveal CNV access. A commonly selected retinotomy site may be the area temporal to the fovea near the horizontal raphe (6). The retinotomy can be made by using a 36-gauge 130-degree angled subretinal pick to perforate neurosensory retina (Fig. 43-3). Care must be taken not to scrape underlying retinal pigment epithelium (RPE) or choroid to avoid bleeding or subsequent development of CNV (7). A 36-gauge angled pick creates a small, almost imperceptible access site to the subretinal space. It is ideal for small subfoveal CNV. Alternatively intraocular diathermy can be lightly applied to the edge of a large of extrafoveal membrane to create the retinotomy site. In this fashion, a retinotomy can be performed through the area of diathermy with a myringotomy blade (8). This creates a larger, more visible access site to the subretinal space. Any retinal capillary hemorrhages can be easily controlled by temporarily raising intraocular pressure to 100 mm Hg pressure. If utilizing the first technique, attention must be paid to the precise location of the small, almost imperceptible retinotomies, so that other instruments can be introduced in the subretinal space at the same site. If necessary, a retinotomy can be carefully lengthened with vertical scissors (6).
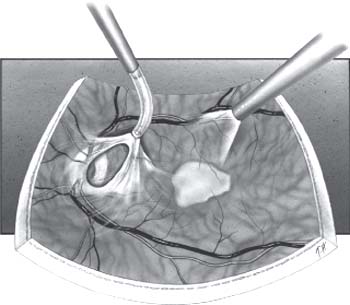
Figure 43-1. A soft-tipped silicone cannula is used to separate the posterior hyaloid from the retinal surface.
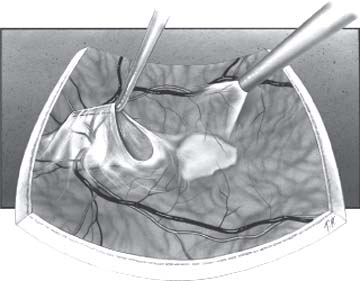
Figure 43-2. A “hyaloid lifter“ is used to hook a Weiss– ring and create a surgical posterior vitreous detachment.
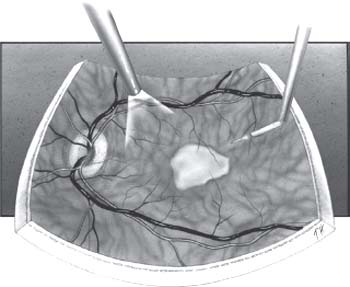
Figure 43-3. A 36-gauge angled subretinal pick is used to create a retinotomy.

Figure 43-4. A 33-gauge angled cannula is used to create a limited neurosensory retinal detachment.
A shallow, limited neurosensory detachment is created to provide working space under the retina and to gain access to the submacular CNV. A 130-degree angled 33-gauge cannula is introduced through the retinotomy, and a trace amount of balanced salt solution is infused in a slow controlled manner into the subretinal space by the surgical assistant (Fig. 43-4). A vigorous infusion can blow a hole through the fovea or create a retinal dehiscence at points of retinal-subretinal adhesion. The angled 33-gauge cannula and concomitant hydrodissection can be used to separate the overlying retina from the underlying subretinal pathology gently. Scars from previous laser surgery, fibrotic CNV, chronic lipid from the CNV, and chorioretinal anastomoses can prove particularly adherent. It is important to release all attachments to the neurosensory retina so that removal of CNV will not result in macular tears. There is also a 36-gauge microcannula available for subretinal use (9).
The 130-degree angled subretinal pick is used through the retinotomy to bluntly dissect the CNV from the surrounding tissue (Fig. 43-5). If the CNV lies anterior to the RPE, as in the case of a membrane secondary to ocular histoplasmosis, the pick can be used to lift the edges of the CNV off the underlying sheet of RPE. There is a rim of fibrin that may also be elevated. All edges of the CNV can be dissected off the RPE, so that only the vascular ingrowth stalk remains attached to the choroid. If the CNV lies beneath or within the RPE layer as in membranes secondary to AMD, the pick can be used to dissect the CNV free from surrounding tissues and limit the area of RPE lost with extraction of the CNV. Pick dissection is carried out under normal intraocular pressure, but pressure is elevated quickly at the first sign of hemorrhage. If necessary, the endolaser probe can be placed behind the retina to achieve hemostasis by photocoagulation (6). After dissection and separation of the CNV, the 130-degree angled horizontal forceps are introduced through the retinotomy to grasp and slowly remove the CNV (Fig. 43-5). When the CNV has been dissected free except for the vascular ingrowth stalk, the tissue is extracted easily, leaving behind intact RPE. It is important to raise the intraocular pressure for hemostasis prior to disconnecting the vascular ingrowth stalk. Intraocular pressure is lowered slowly, with careful observation for any bleeding. When being pulled out from the subretinal space, CNV complexes usually fit easily through small retinotomies and can then be aspirated with the vitrector. Alternatively, the CNV complex can be removed from the eye through the pars plana, if histopathologic examination is desired. Occasionally, the tissue may be so fibrotic that it cannot be cut by the vitrector and may require enlargement of the sclerotomy and extraction through the pars plana. If the retinotomy is enlarged, additional endothermy may be applied at the edges sufficient to visualize the edges of the retinal defect (6). It may be desirable to laser large, irregular retinotomies if they are well extrafoveal.
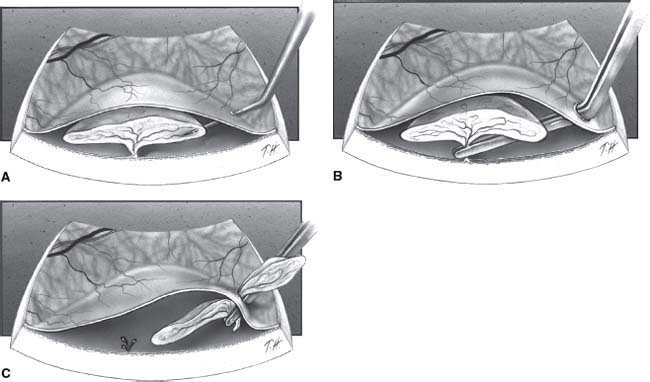
Figure 43-5. The angled subretinal pick is used to bluntly dissect the choroidal neovascularization from surrounding tissue. The edge of the membrane can then be grabbed with horizontal subretinal forceps. Hemorrhage at the vascular ingrowth stalk is prevented by raising the intraocular pressure.
In cases in which the RPE will probably be extracted along with the CNV, one must watch carefully for the cleavage point of the RPE. If it appears as though a large area of healthy RPE need to be removed, horizontal subretinal scissors can be used to cut healthy RPE from the diseased tissue. This can also be done to cleave CNV from adherent laser scars.
Indirect ophthalmoscopy is carried out to confirm that no iatrogenic retinal tears have occurred from passing sharp, angled instruments into the eye. If tears are seen they can be treated with cryopexy or laser followed by gas tamponade. If a large tear is visualized, then a buckle may also be placed. The retinotomy site is usually not treated with laser photocoagulation due to its macular location. Laser may be considered for certain circumstances such as large retinotomy, extensive subretinal blood or extramacular location. A complete air-fluid exchange is carried out, aspirating over the optic nerve head with a soft-tipped extrusion cannula. A 33-gauge cannula can be used to aspirate at the retinotomy, removing any residual subretinal fluid or hemorrhage. In uncomplicated cases, fluid may be reintroduced into the vitreous cavity with a soft-tipped cannula pointing away from the macula and retinotomy until only a 10% to 15% gas bubble remains. A full air or gas fill may be indicated in patients who cannot maintain face-down positioning after surgery. Postoperatively, the patient is instructed to remain strictly face-down overnight so that the air bubble can seal the retinotomy.
A surgeon may use a nonexpansile concentration of perfluoropropane gas (C3F8) in aphakic or pseudophakic eyes to eliminate the need for prone positioning or to achieve prolonged gas tamponade. In phakic eyes, sulfur hexafluoride gas may be used. In cases of a large retinotomy or inability to position, silicone oil may be rarely employed (6).
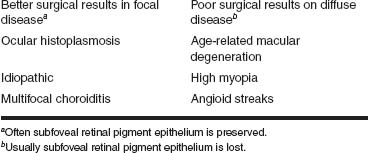
TABLE 43-1 SUMMARY OF SURGICAL RESULTS
ANATOMICAL FINDINGS IN SUBMACULAR SURGERY
Submacular surgery was pioneered for the removal of subfoveal CNV resulting from a number of causes including AMD, ocular histoplasmosis, multifocal choroiditis, high myopia, angioid streaks, and idiopathic causes. With the advent of therapy utilizing agents targeting VEGF submacular surgery is less commonly used.
Surgical success after removing subfoveal CNV depends on the underlying disease. Eyes with subfoveal CNV caused by focal disease of the RPE-Bruch’s membrane-choriocapillaris complex have a good chance for better postoperative visual acuity (VA) (10) (Table 43-1). Postoperative VA of 20/40 or better, in 30% to 40% of eyes with subfoveal CNV caused by ocular histoplasmosis, multifocal choroiditis or idiopathic causes have been observed in several retrospective series (11–16). With focal disease, the CNV membrane lies anterior to the RPE (Fig. 43-6). If the CNV is removed surgically, the subfoveal RPE is preserved. In contrast, eyes with subfoveal CNV caused by diffuse degenerative diseases of the RPE-Bruch’s membrane-choriocapillaris complex have little chance for better postoperative VA (10) (Table 43-1). Examples of diffuse degenerative disease of the RPE-Bruch’s membrane-choriocapillaris complex include age-related macular degeneration, angioid streaks, and myopic degeneration. In cases of CNV secondary to degenerative disease, the CNV lies under or within the RPE (Fig. 43-7), when the CNV is removed, subfoveal RPE is removed as well. Following submacular surgery, intact native RPE is critical to foveal photoreceptor function and return of good VA (16).

Figure 43-6. If the choroidal neovascularization has a single ingrowth stalk and lies anterior to the retinal pigment epithelium, there is a favorable surgical prognosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


