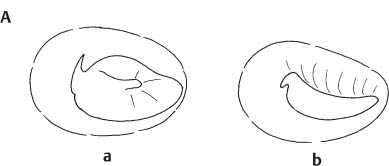
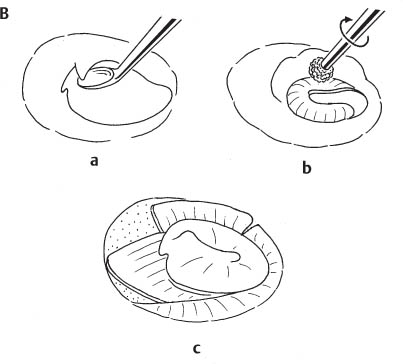
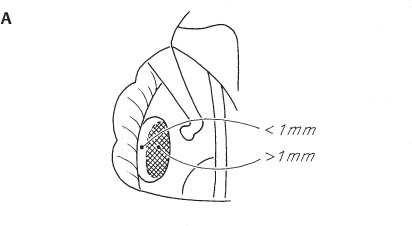
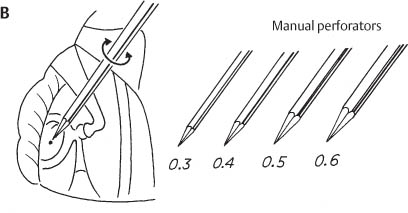
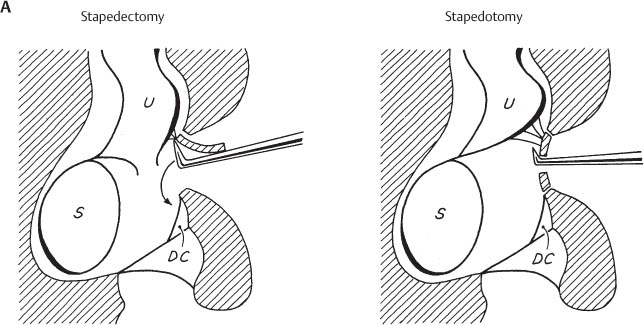
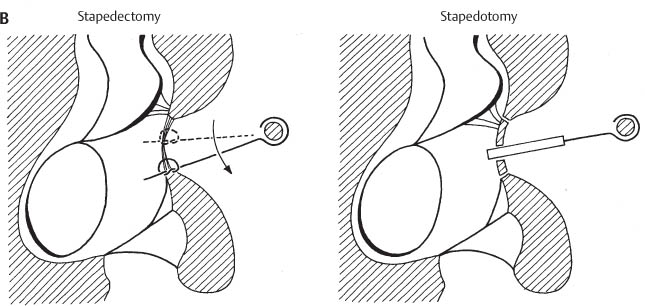
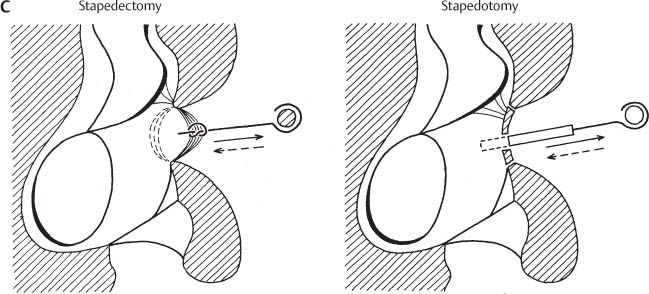
Chapter 7 Stapedotomy and Stapedectomy In our hands, the limited central perforation of the footplate (stapedotomy) has replaced the partial (small fenestra) or total removal of the stapes foot-plate (stapedectomy) since 1978 for reasons illustrated in Figures 106A–C. During stapes surgery the stapes prosthesis can be attached to the incus (incus-stapedotomy [IS]) or to the malleus handle (malleo-stapedotomy [MS]). Fig. 106A A 0.4-mm stapedotomy carries less risk of inner ear damage than a total or subtotal stapedectomy. Correct total removal of the footplate may induce a sensorineural hearing loss and vertigo because of unavoidable damage to the utricle when superior fibrous adhesions are present in the vestibule. Fibrous adhesions between the superior footplate and the utricle were found in two-thirds of the normal temporal bones of our histologic collection. U: utricle; S: saccule; DC: cochlear duct. Fig. 106B A limited perforation through the footplate (stapedotomy) prevents lateral displacement of the prosthesis due to traction of postoperative scarring. A wire connective-tissue prosthesis used with stapedectomy can migrate toward the inferior or superior edge of the oval window. This has been found to induce conductive or even sensorineural hearing loss and vertigo (lesion of the endolymphatic duct and/or utricle). Fig. 106C The membrane, which covers the open oval window after stapedectomy, may be displaced laterally by (1) an increase in perilymphatic pressure, (2) scar retraction, particularly with a wire connective-tissue prosthesis that is too short, or (3) by movements of the incus following sneezing or rapid changes in middle ear pressure. Revision surgery shows that the lateral displacement of the oval window membrane can cause lateralization of the properly sized prosthesis with incus erosion. It is also possible that incus movements due to barotrauma (flying, crossing mountains by car) may cause a sudden hearing loss years after a successful stapedectomy. This complication is less likely to occur after stapedotomy since, in the latter case, the prosthesis may be pulled out from the stapedotomy opening without adversely affecting the inner ear. The surgical steps of stapedotomy are demonstrated for otosclerosis since this condition is the most common indication for the procedure. In 1978 we began to reverse the classic steps of stapes surgery using a 0.4-mm Teflon platinum piston (TPP). The reversal consisted of making the stapedotomy opening as well as the introduction and fixation of the piston before removal of the stapes arch. In September 1996 we discontinued the Teflon platinum piston and introduced the 0.4-mm Titanium stapes prosthesis (see p. 374). We maintained the reversal of the classic steps of stapes surgery. This reversal permits formation of a central stapedotomy opening without mobilization or fracture of the foot-plate. Furthermore, the prosthesis loop can be better attached while the incus remains stabilized by the intact incudostapedial joint. This avoids the danger of incus luxation or excessive displacement of the prosthesis into the vestibule while crimping. The use of a 0.4-mm piston is essential to reverse systematically the classic steps of stapes surgery. The limited space between the stapes arch and facial nerve prevents the consistent use of larger (0.6-mm or 0.8-mm) pistons. There is no evidence that larger pistons give better results than a 0.4-mm prosthesis (Hüttenbrink 2003, 10-R). In the late 1980 s, we began to perform stapedotomies with attachment of the prostheses to the malleus handle. This operation has become increasingly dominant in our practice since the introduction of the Titanium stapes piston (TSP) because more attention was paid to the role of the anterior mallear ligament in partial fixation of the malleus in otosclerotic patients. To distinguish the stapedotomy performed with the prosthesis attached to the incus from that carried out with the prosthesis attached to the malleus handle, we have introduced the terms incus-stapedotomy and malleo-stapedotomy. The following surgical technique of IS is described as it has been performed for 18 years (1978–1996). The changes which have occurred since will be mentioned in the course of the description (in italics).
General Considerations
 Stapedotomy versus Stapedectomy
Stapedotomy versus Stapedectomy
Less risk of inner ear damage in stapedotomy
Less probability of prosthesis migration after stapedotomy
No lateral displacement of the oval window membrane in stapedotomy
Specific Surgical Techniques
 Stapedotomy
Stapedotomy
Surgical Technique
 Incus-Stapedotomy
Incus-Stapedotomy
Surgical Highlights |
|
Surgical Steps
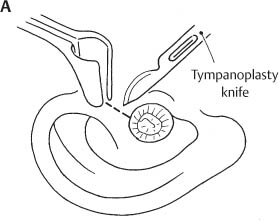
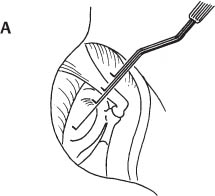
Fig. 107A
Endaural skin incision
A helicotragal skin incision is carried out using a No. 15 blade on a flat scalpel handle (7-I) while enlarging the external canal with a nasal speculum.
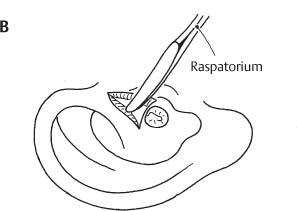
Fig. 107B
Widening of the EAC
An endaural raspatory (75-I) is used to separate the soft tissue from the underlying bone at the superior edge of the EAC.
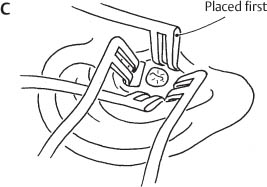
Fig. 107C
Widening of the EAC (cont.)
Two Fisch endaural retractors (1-I) are placed perpendicular to each other over the entrance of the EAC to give the necessary exposure.
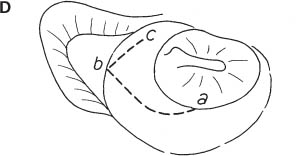
Fig. 107D
Meatal skin flap
The meatal portion of the tympanomeatal flap is called the meatal skin flap. This is to stress the fact that the tympanic portion of the flap should not be elevated before completion of flap elevation and possible anterosuperior canalplasty. This prevents contamination of the tympanic cavity with rinsing solution placed in the EAC. The triangular meatal skin flap has a posterior limb (a–b) that begins at 8 o’clock, ascending spirally from the tympanic annulus to the lateral edge of the EAC at 12 o’clock. The anterior limb of the meatal skin incision (b–c) descends from the lateral opening of the external canal along the upper end of the tympanosquamous suture in front of the lateral process of the malleus. The meatal incisions are carried out with a No. 11 blade on a round scalpel handle (see Instrumentation).
Modifications: Since the discovery of the role of the anterior mallear process and ligament in malleus fixation, the tympanomeatal flap has been extended to determine the condition of these structures in all cases of stapedotomy. In consequence, the tympanomeatal flap used since 1996 encompasses the anterosuperior canal wall. To achieve this, the anterior limb of the flap extends along the anterior canal wall until 3 o’clock (right side) and descends thereafter a few millimeters medially as for MS (see Fig. 119A1).
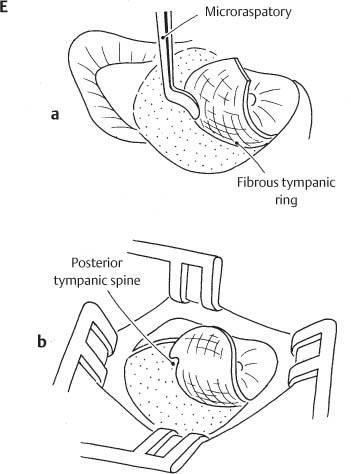
Fig. 107E
Meatal skin flap (cont.)
a The meatal skin flap is elevated from the underlying bone with the Fisch microraspatory (23-I, 24-I).
b The most important landmark in this step is the posterior tympanic spine (posterior end of the tympanic notch).
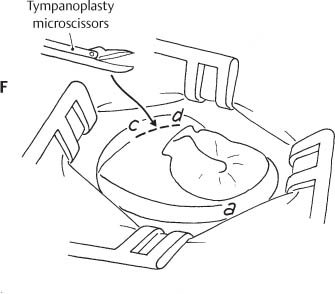
Fig. 107F
Meatal skin flap (cont.)
After exposure of the posterior tympanic spine, the anterior limb of the meatal incision is extended with tympanoplasty microscissors (52-I) toward the anterior tympanic spine (c-d), remaining above the short process of the malleus.
Modifications: See Figure 107D and 119A1.
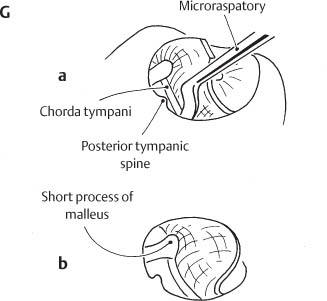
Fig. 107G
Tympanomeatal flap
Elevation of the meatal skin flap has been completed. The tympanic portion of the tympanomeatal flap can now be detached from the bone.
a Elevation of the tympanic ring from the tympanic sulcus begins at the posterior tympanic spine, using a Fisch microraspatory (23-I, 24-I).
b The chorda tympani is left attached to the retracted drum. The pars flaccida of the tympanic membrane is elevated with the microraspatory over the neck and short process of the malleus. A cartilaginous apophysis may be found over the lateral process of the malleus. This cartilage is elevated with the tympanomeatal flap. Exposure of the short process of the malleus keeps the tympanomeatal flap away and allows early determination of the mobility of this ossicle. Gelfoam soaked in 1% lidocaine solution is placed in the exposed middle ear cavity for 2 minutes if pain is experienced by the patient during elevation of the tympanomeatal flap.
Fig. 108A
Canalplasty
Correct elevation of the tympanomeatal flap implies good visualization of the lateral process of the malleus. A prominent tympanosquamous spine (a) or a prominent anterior wall of the external canal (b) may prevent adequate visualization.
Fig. 108B
Canalplasty (cont.)
The large end of a curette (a,15-I) or a diamond burr (b) is used to enlarge the anterosuperior portion of the external canal until the lateral process of the malleus and the anterior tympanic spine become visible. Using the burr requires irrigation, which can lead to contamination of the middle ear. Therefore, canalplasty should be carried out before separating the tympanic annulus from its sulcus.
c Correct exposure of the malleus following canalplasty.
Modifications: The anterosuperior canalplasty is nearly the rule for correct exposure of the anterior tympanic spine. As already stated in the previous figures, we prefer the diamond burr to the curette for prolonged work on the bony EAC. The proper exposure is reached when the posterior tympanic spine, the anterior tympanic spine, and the lateral process of the malleus are visible. Posterior to the lateral process of the malleus is the chorda tympani. Anterior to the lateral mallear process, the anterior mallear process with its ligament is exposed. The chorda tympani lies just medial to these structures and should remain intact (see Fig. 119C2).
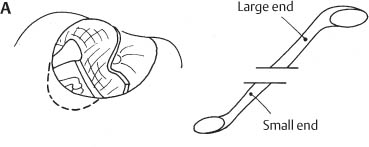
Fig. 109A Exposure of the oval window
After elevation of the tympanomeatal flap, the bone covering the oval window niche is removed with the small end of a sharp curette (15-I). Care is taken to avoid trauma to the chorda tympani.
Fig. 109B
Exposure of the oval window (cont.)
The rotational movements of the sharp curette are directed from medial to lateral when exposing the oval window. Bone fragments should be continuously removed to avoid inadvertent luxation of the incus by pushing them medially with the curette.
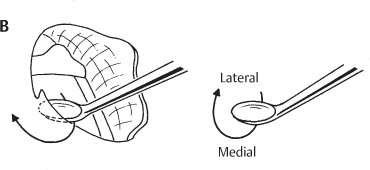
Fig. 109C
Exposure of the oval window (cont.)
Correct exposure of the oval window is obtained when the short process of the malleus, the tympanic segment of the facial nerve, and the pyramidal process are visible. Visualization of these three landmarks is essential for correct execution of the further surgical steps.
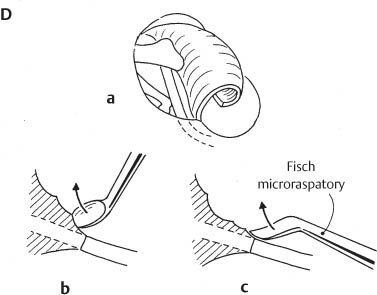
Fig. 109D
Mobilization of the chorda tympani
At times the chorda tympani runs within the bony posterior canal wall, preventing correct exposure of the oval window (a). If this is the case, the bone covering the chorda has to be removed using the small end of a sharp curette (b, 15-I) or with the Fisch microraspatory (c, 23-I, 24-I).
The chorda tympani should be preserved whenever possible. However, if mobilization is impossible without lesion, the chorda is cut with ultra fine tympanoplasty microscissors (51-I).
Fig. 110A
Determination of prosthesis length
A malleable measuring rod (37-I) is used to determine the distance between the foot-plate and the lateral surface of the incus (average length 4.7 mm); 0.5 mm is added to account for the protrusion of the pros-thesis into the vestibule. The average total length of the prosthesis is, therefore, 5.2 mm. Manipulations of the mucosa of the oval window may cause pain. In this case, a Gelfoam pledget soaked in 1% lidocaine is placed in the oval window for 2 minutes.
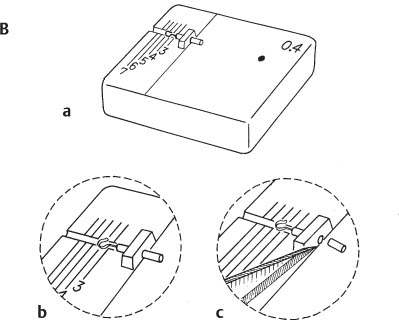
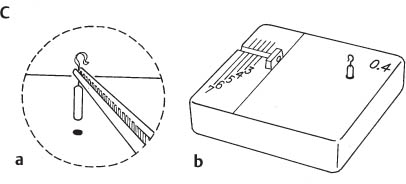
Fig. 110B
Trimming the prosthesis
A special cutting block has been developed so that only one size prosthesis, a Teflon platinum piston (TPP) measuring 0.4 mm in diameter and 7 mm in length, is stocked (since September 1966 we have been using a 8.5 mm × 0.4-mm titanium stapes piston; see Modifications, p. 231). The prosthesis is trimmed on the cutting block (a). The prosthesis is placed on a groove of the cutting block and advanced with a watchmaker forceps (10-I) through the perforated bridge until the desired length is reached (b). The excess of the Teflon piston is cut away using a No. 11 blade (c).
Modifications: A special cutting block (57-I) has also been developed for the titanium stapes prosthesis. This block is used for all types of titanium prostheses (see Fig. 119H1). The cutting block for titanium pros-theses allows storage of a 0.4 mm × 8.5 mm titanium stapes piston (normal size), which is trimmed to the desired length (within 0.1 mm). The cut end of the titanium piston oxidizes within milliseconds, thus there is no danger of ionic transfer occurring when the prosthesis is introduced into the perilymph. The malleability of titanium prevents the formation of sharp edges on the cut end of the prosthesis.
Two other lengths of prosthesis (0.4 mm × 7 mm and 0.4 mm × 10 mm) are available. These prostheses differ from the 8.5-mm TSP by a longer (2 mm) and shorter (1 mm) shaft between loop and piston. The longer and shorter TSP are used for stapedotomy in shallow middle ear cavities (e.g., open cavities) or in deep middle ear cavities (e.g., congenital ears).
Fig. 110C
Storage of the prosthesis
The trimmed prosthesis is grasped with a watchmaker forceps and placed in the 0.4-mm hole of the cutting block for later use.
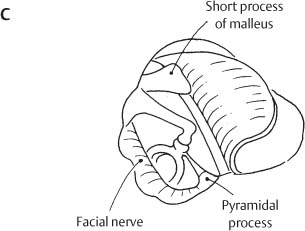
Fig. 111A
Safe area for stapedotomy
Measurements made in normal and otosclerotic bones of our temporal bone collection have shown that the saccule and utricle are more than 1 mm below the inferior central two-thirds of the stapes footplate (Pauw et al. 1991, 20-R). This is, therefore, the safest place for the stapedotomy opening.
Fig. 111B
Perforation of the footplate
A set of four manual perforators (0.3, 0.4, 0.5, and 0.6 mm in diameter) (40–43-I) is used to make the stapedotomy opening in the footplate. The perforators are rotated back and forth between the thumb and index finger of the right hand. The tip of each perforator is only partially introduced into the vestibule; in this way the 0.6-mm diameter perforator produces the desired opening of 0.5 mm. The pressure applied to the perforator tip is minimal. The actual work is carried out with the perforator’s shoulder. The perforator should be kept along the posterior surface of the incus and perpendicular to the footplate of the stapes (future position of the stapes prosthesis).
Modifications:Alternatives for perforation of the footplate are: (a) the burr and (b) the laser beam. The burr (0.6 mm and 0.8 mm diamond) is used with the Fisch micro handpiece which was specially developed for work in the middle ear and oval window (see p. 376). The burr is particularly helpful in an obliterated oval window, but can also be used in a thin foot-plate after reducing the drill speed to a minimum.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Local or general anesthesia.
Local or general anesthesia. Endaural skin incision.
Endaural skin incision. Formation of meatal skin flap.
Formation of meatal skin flap. Anterosuperior canalplasty.
Anterosuperior canalplasty. Elevation of tympanomeatal flap.
Elevation of tympanomeatal flap. Evaluation of mobility of the malleus and incus.
Evaluation of mobility of the malleus and incus. Exposure of oval window.
Exposure of oval window. Evaluation of mobility of the stapes.
Evaluation of mobility of the stapes. Trimming and storage of a 0.4-mm TPP or TSP on the special cutting block.
Trimming and storage of a 0.4-mm TPP or TSP on the special cutting block. Stapedotomy with manual perforators or laser.
Stapedotomy with manual perforators or laser. Introduction and fixation of TPP or TSP with intact incudostapedial joint and stapes arch.
Introduction and fixation of TPP or TSP with intact incudostapedial joint and stapes arch. Division of stapes arch with prosthesis in place using crurotomy scissors.
Division of stapes arch with prosthesis in place using crurotomy scissors. Sealing of stapedotomy opening with connective tissue, venous blood, and fibrin glue.
Sealing of stapedotomy opening with connective tissue, venous blood, and fibrin glue. Packing with Gelfoam.
Packing with Gelfoam. Closure of endaural incision.
Closure of endaural incision.