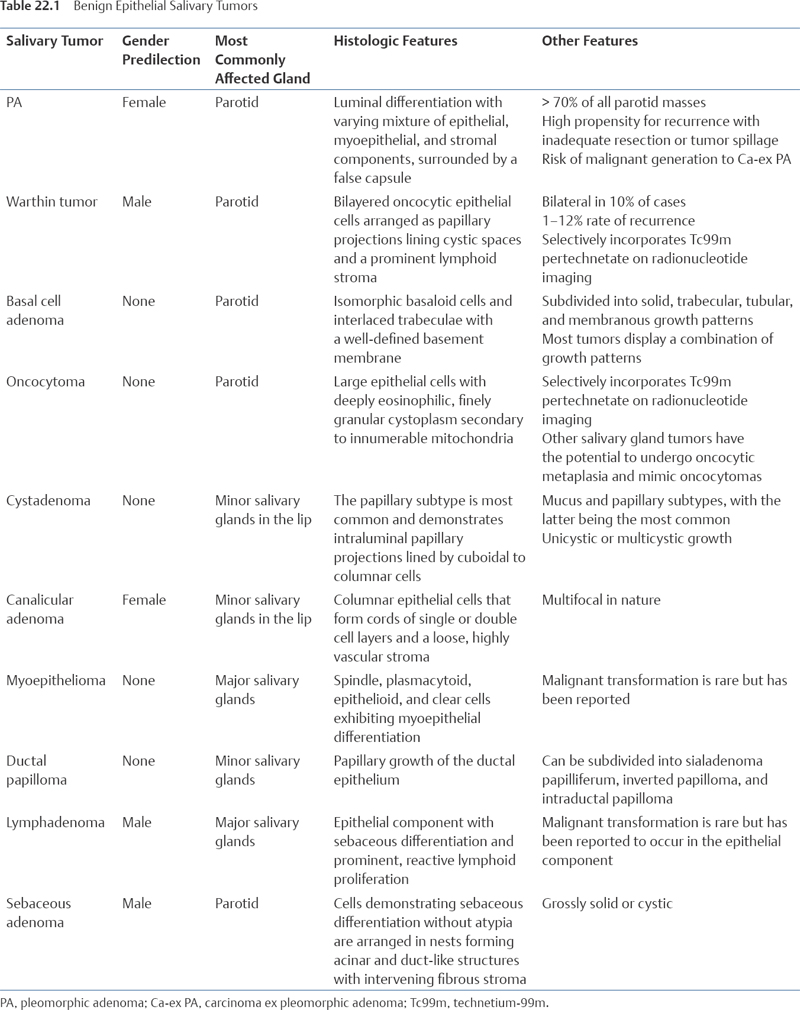
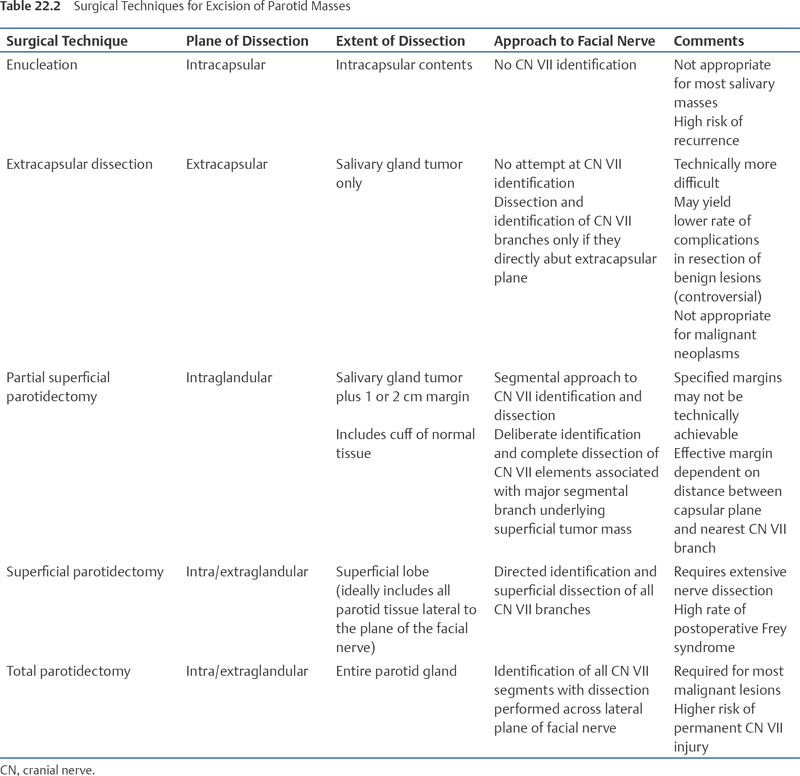
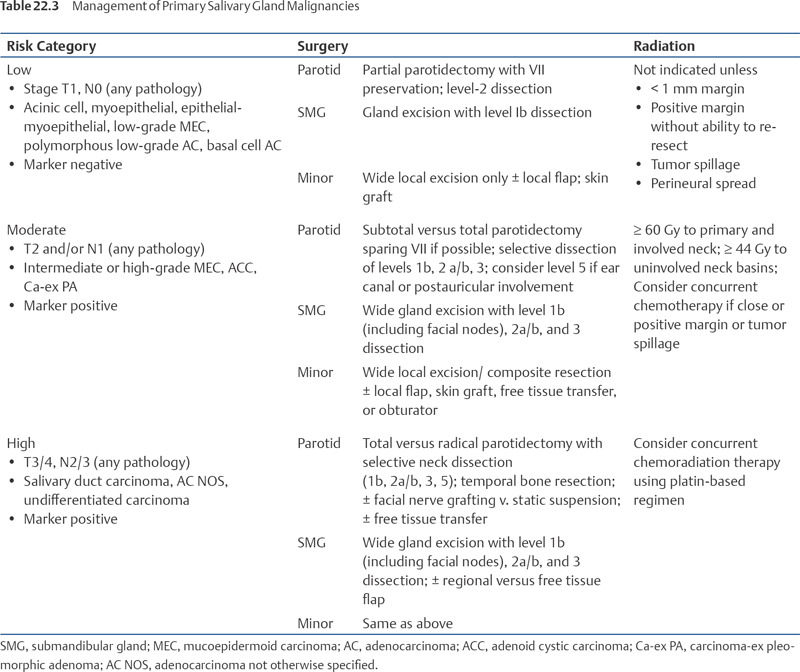
22 Core Messages • The majority of salivary gland tumors present as asymptomatic masses with indolent progression. Timely, comprehensive evaluation and treatment of all salivary masses is critical, because of the complications associated with progression of benign lesions and the risk of malignancy. • Ultrasound is the preferred imaging modality for presumed benign lesions of submandibular, sublingual, and superficial parotid tumors. Magnetic resonance imaging is warranted if any features suggestive of malignancy are present. • Fine-needle aspiration is safe, rapid, inexpensive, and adequately sensitive, and is thus the optimal method for preoperative tissue sampling of salivary neoplasms. • Surgical resection in eligible candidates is required for most benign and all malignant salivary neoplasms. In the setting of malignancy additional treatment, such as neck dissection or adjuvant radiation therapy, is variable and determination is based primarily on tumor stage and grade. • Surgical approaches to excision of benign tumors of the superficial parotid gland vary with regards to planned extent or resection and facial nerve dissection, and the choice of techniques for excision of these masses remains controversial. Salivary gland neoplasms arise within a common group of glands in the head and neck region: the parotid, submandibular, sublingual, and minor salivary glands. Most salivary gland tumors present as an asymptomatic, slowly enlarging mass in the region of a major salivary gland. Salivary gland cancers are relatively rare, accounting for only 20% of salivary tumors and 5% of all head and neck malignancies.1 Up to 75% of salivary gland tumors are benign and the majority are asymptomatic. Both the asymptomatic quality and indolent growth rate of most salivary gland tumors may lead to an undue delay in diagnosis and provision of appropriate care. Comprehensive evaluation of salivary gland tumors is critical, as inappropriate treatment greatly increases the risk for persistent and recurrent disease. Moreover, failure to accurately diagnose and adequately treat malignant salivary disease can have grave consequences. Ultrasound (US), X-ray, computed tomography (CT), and magnetic resonance imaging (MRI) may be used in the detection and assessment of salivary gland tumors. Preoperative imaging may not be necessary in all cases of parotid masses, as surgical extirpation is the standard treatment modality. Imaging studies are mandated, however, in cases of suspected malignancy, and may be helpful in preoperative planning and patient counseling. There are several advantages to imaging salivary gland tumors before treatment. Imaging helps confirm that the mass originates from the salivary gland and is not because of adjacent pathology (e.g., lipoma, adnexal mass, lymph node). Pretreatment scans assist operative planning by defining the relationship between the mass and nearby vital structures such as cranial nerves and blood vessels. Although no imaging modality can accurately depict the relationship of a parotid tumor mass to the facial nerve, the plane demarcated by the lateral border of the retromandibular vein can serve as a reasonable proxy for the level of the facial nerve. Assessment of the depth of the tumor relative to this plane can assist the surgeon in predicting the necessity of deep lobe extirpation.2 Further, imaging can detect possible signs of malignancy not readily appreciable by physical examination, such as ill-defined tumor borders, invasion of surrounding structures (e.g., ear canal, muscle, bone), enhancement or thickening of the facial and trigeminal nerves, the presence of multifocal disease, and local nodal metastases. US is the preferred imaging modality for suspected benign submandibular, sublingual, and superficial parotid tumors. Advantages of US include the fact that it can facilitate fine-needle aspiration (FNA) and it does not require administration of radiation. US is relatively inexpensive and can help characterize the following tumor characteristics: size and border regularity, the pattern of vascularity, multifocality, and adjacent lymphadenopathy. Disadvantages include the fact that US sensitivity and specificity are somewhat operator-dependent and that the ability to depict the deep aspects of the parotid gland and the parapharyngeal space is limited because of acoustic absorption, dispersion, and obscurement by the mandible.3 Moreover, interpretation of US images of the salivary glands is more challenging than corresponding MRI or CT images for those without extensive experience.4 US imaging is also unsuitable for assessing perineural spread, extraglandular invasion of bone or soft tissue, and oropharyngeal or retropharyngeal nodal metastases.5 If a malignant process is suspected, MRI with gadolinium is preferred because of its superior salivary tissue resolution, ability to assess marrow spaces, and capacity for revealing cranial nerve enhancement or thickening.6 CT may be of value if MRI is unavailable or may serve as a useful adjunct to MRI if the tumor is fixed to the temporal bone or mandible, as it is superior in detecting bony involvement. Fluorodeoxyglucose positron emission tomography is rarely indicated in the primary evaluation of salivary gland tumors because of the expense, lack of supporting evidence regarding its diagnostic value, and its high rate of false positives for malignancy in the setting of benign salivary tumors such as pleomorphic adenoma (PA) and Warthin tumor.7 No imaging technique can reliably differentiate between benign and malignant salivary tumors; therefore, radiographic findings alone should not be used as a justification to defer adequate treatment of a salivary mass. FNA biopsy is the preferred method for preoperative tissue sampling of salivary gland neoplasms. FNA is simple, rapid, and relatively inexpensive with little morbidity and low risk of malignant seeding. As surgical excision remains the standard treatment strategy for most salivary gland tumors, FNA may not substantially alter therapy. Therefore, performance of FNA is not mandated in all cases. Potential benefits to FNA include more accurate patient counseling regarding the likelihood of malignancy and operative risk. Surgical approaches may differ based on the expectation of malignancy. Moreover, even if benign pathology is confirmed on FNA, discrimination between the most common types of benign neoplasms may influence surgical techniques.8 The overall sensitivity of FNA for detection of salivary gland neoplasia is 89.4% and its accuracy for discriminating between benign and malignant salivary tumors is 79.1%.9 Diagnostic accuracy is enhanced with the use of US guidance.10 The diversity of tumor types can make cytopathologic diagnosis and subtyping based on FNA difficult. Diagnosis is further complicated by the potential for sampling error and the histologic similarities of tumor types with very different behaviors (so-called look-alike tumors). The common overlap in the cytopathologic morphologies also complicates malignancy determination; however, an experienced head and neck cytopathologist is often able to determine whether a salivary mass is likely benign or malignant based on cellular density, morphology, uniformity, and the presence of mitotic figures with an overall accuracy of 80%.11 Whereas a negative FNA finding does not eliminate the possibility of cancer and should not be used as the sole reason not to treat, a biopsy positive for malignancy greatly increases the true likelihood of cancer. With this information, the surgeon can plan an appropriate surgical approach and counsel the patient concerning the potential need for neck dissection, facial nerve resection, and reconstructive options. The false-negative rate in US-guided FNA of major salivary gland tumors is 4.2%.12 Although approximately 25% of initial FNA specimens are nondiagnostic, repeat FNA specimens may commonly lead to an ultimate cytopathologic diagnosis; sensitivity (85%) and specificity (93%) rates in detecting salivary gland malignancy on repeat FNA are comparable to those of initial specimens.13 Overall, more than 90% of preoperative FNA specimens are interpreted as PA.14 In a review of 879 FNA biopsies of major salivary gland tumors, Christensen et al found that FNA yielded accurate preoperative identification of tumor subtype in 97% of benign lesions and 71% of malignant lesions.15 Roughly 75% of all salivary gland tumors are benign. Benign salivary gland neoplasms typically present as slow-growing, painless masses in the region of a salivary gland. Imaging is not mandated in suspected benign salivary gland neoplasms; however, it can assist with tumor characterization and preoperative planning, as the definitive treatment remains surgical excision. The histopathology of benign salivary gland tumors is extremely diverse, with the most common tumor being PA. Recently, the World Health Organization divided benign epithelial tumors into 10 subtypes.16 A summary of these subtypes and their respective key features is provided in Table 22.1. Soft tissue tumors, such as hemangiomas, and hematolymphoid tumors, such as Hodgkin lymphomas, diffuse large B-cell lymphomas, and extranodal marginal zone B-cell lymphomas can, also be classified as benign salivary gland tumors. Although surgical excision is the mainstay of treatment for benign salivary gland neoplasms, the appropriate choice of surgical technique, particularly regarding the extent of parotid gland dissection, remains controversial. Debate over this issue has been shaped by multiple—sometimes competing—imperatives, including concerns regarding tumor recurrence, facial nerve preservation, and cosmetic considerations. In the first half of the 20th century, the preferred approach to surgical treatment of parotid neoplasms involved simple enucleation alone. Mid-century, a shift in the standard approach toward more extensive facial nerve dissection and comprehensive gland excision occurred. This change in prevailing surgical opinion was driven by multiple factors, including increased recognition of the high rates of PA recurrence following enucleation. This shift in opinion was further supported by the findings of Patey and Thackray, who described the prevalence of microscopic PA extracapsular extension in a landmark histopathologic study in 1957.17 The preferred approach to extirpation thus shifted toward superficial parotidectomy or en bloc excision of essentially all parotid tissue lateral to the plane of the facial nerve as the minimal acceptable degree of resection. In recent years, there has been a resurgence of interest in subtotal parotid excision techniques. Several distinct techniques have been described: enucleation, extracapsular dissection, limited parotidectomy, subtotal parotidectomy, partial-superficial parotidectomy, superficial parotidectomy, and total parotidectomy. The partial-superficial parotidectomy approach, as described by Iizuka and Ishikawa, entails segmental resection in which facial nerve dissection is limited to the main trunk and the distal segmental branch proximate to the tumor.18 The extracapsular dissection method, which uses dissection within the loose areolar plane surrounding the fibrotic PA pseudocapsule without directed facial nerve identification or dissection, was first comprehensively described by Gleave and has subsequently been elaborated upon by multiple authors.19 Minimally invasive endoscopic techniques using facelift-type incisions have also recently been reported.20 Although enucleation may be appropriate for some types of benign lesions, it is inadequate for resection of PA because of the unacceptably high rate of recurrence. However, the appropriate planned extent of excision for salivary benign neoplasms, and PAs of the parotid gland in particular, remains a matter of debate. Some contemporary authors maintain that superficial parotidectomy constitutes the only suitable technique, reporting that complete ablation of the lateral lobe decreases the risk of tumor recurrence and facial nerve injury.21 The body of literature in favor of more limited approaches in selected cases has grown, however, with extracapsular dissection emerging as the favored alternative. Riad et al have noted that even when resection is attempted with a superficial parotidectomy or a specified width of surrounding tissue cuff, close approximation of the tumor to the facial nerve occurs in many cases. Thus, the actual margin that can be obtained in the setting of facial nerve preservation is limited and often entails only a thin plane of tissue between the tumor capsule and the underlying facial nerve. In their recent review of 182 cases of parotid resections for PAs, resection margin had no apparent impact on recurrence rates; the only factor predictive of recurrence was intraoperatively recognized gross tumor spillage or pathologically confirmed surgical tumor puncture.22 Witt compared results of partial superficial parotidectomy for PA using either 1- or 2-cm margins and reported no difference in outcomes or complication rates, while noting the fact that the effective margin of resection in a nerve-sparing approach is dictated not by the surgeon’s planned width of normal tissue cuff, but rather by the distance between the capsular plane and the most proximal facial nerve branch. Their group stressed that close abutment of the capsule to a facial nerve branch is a nearly ubiquitous finding in PA excisions.23 In a review of 100 consecutive cases of superficial parotidectomy for PA, Donovan and Conley found that a significant margin of parotid tissue between the PA capsule and the facial nerve could not be achieved in more than 60% of cases. They argue that the achievement of “en bloc resection of parotid tumors” using superficial parotidectomy is an “illusion” in the majority of cases.24 In a series of 162 parotid resections, Hancock highlighted the potential advantage of extracapsular dissection in decreasing the risk of gustatory sweating or Frey syndrome because of postoperative sympathetic–parasympathetic cross-innervation, with a reported rate of 25% prevalence following superficial parotidectomy as compared with 0% after extracapsular dissection.25 Smith and Komisar reported no instances of capsular rupture, temporary or permanent paresis, or development of Frey syndrome in a series of 27 patients undergoing extracapsular dissection of parotid neoplasms.26 McGurk et al reported significantly decreased rates of complications including transient facial nerve palsy, Frey syndrome, and neuroma when extracapsular dissection methods were employed for “simple” parotid masses; they advocated that the decision to employ an extracapsular dissection or superficial parotidectomy should be made intraoperatively following elevation of the skin flap based on the following characteristics: apparent tumor size, fixation, palpable nodal involvement, or palpable deep lobe extension.27 Table 22.2 provides an overview of the different surgical techniques employed for excision of parotid masses. PAs represent the most common benign neoplasm of the salivary glands. Overall, PAs account for more than 50% of all salivary neoplasms and more than 70% of parotid masses.28 Although the role of risk factors in the development of salivary PAs has yet to be elucidated, PAs do exhibit a female predominance and bimodal age distribution.29 The morphology of PAs is complex and highly variable, making accurate cytologic or histopathologic diagnosis occasionally difficult. Also known as benign mixed tumors because of their diverse morphology, PAs feature luminal differentiation and the presence of epithelial, myoepithelial, and stromal components in varying proportions. The morphologic plasticity demonstrated by PAs stems largely from the proliferative differentiation of salivary myoepithelial cells.30 An additional histologic feature of PAs is envelopment by a false capsule, which develops as the result of a fibrotic reaction by the surrounding salivary parenchyma.31 While PAs often appear to be grossly encapsulated, histologically they feature areas of capsular disruption and small excrescences, often referred to as pseudopodia, the presence of which is related to the propensity for PAs to recur following surgical excision.32 The cytopathologic hallmark of PA is a mixture of bland epithelial cells and chondromyxoid stroma with spindle features, but the relative predominance of epithelial versus mesenchymal matrix varies widely; the overall diagnostic accuracy of FNA for benign PA is 90%.33 Imaging characteristics of PAs have been summarized by Kakimoto et al. On MRI, PAs tend to feature well-defined margins, lobulated borders, inhomogeneity, and intermediate-high signal intensity with high enhancement. Lobulation of borders was a consistent feature of parotid PAs, but was typically not observed in PAs arising from submandibular or minor salivary glands. Although the PA capsule was consistently visualized using MRI, it is detectable on CT imaging in less than 5% of cases.34 Although no imaging modality can reliably discriminate malignant from benign salivary gland tumors, certain imaging findings are suggestive of a malignant aggressiveness including low T1- and T2-signal intensities and muscular invasion.35,36 Grayscale or color Doppler US modalities can help distinguish PAs from Warthin tumors preoperatively based on the degree of lobulation, cystic quality, and echogenicity, with Warthin tumors typically featuring anechoic cystic components and PAs having characteristic lobulations and an absence of anechoic cystic elements.37 The presence of a lobulated contour, which is not observed on radiologic study of other types of benign salivary gland tumors, is the most specific feature of PA on ultrasonography.38 Diffusion-weighted echo-planar MRI techniques are helpful in differentiation of PAs and myoepithelial adenomas from parotid malignancies and other benign histologic subtypes.39 Morphologic distinction of PA from other benign salivary gland tumors can be difficult because of its varying histologic composition and significant morphologic overlap with other benign salivary entities. However, PAs demonstrate consistent expression of the PLAG1 gene irrespective of other gene rearrangements; PLAG1 likely plays a fundamental role in PA development and is a specific immunohistochemical marker that can confirm the diagnosis of PA.40 In addition to PLAG1 rearrangements, HMGA2 translocations have also been found to be specific to PAs; thus, the detection of these specific gene rearrangements using either reverse transcriptase polymerase chain reactions or fluorescence in-site hybridization can aid in diagnosis.41 PAs are also distinct from normal salivary tissue in terms of their microRNA profiles, and the interaction of microRNAs with the 3’ UTR genes that normally inhibit translation may be a critical factor in PLAG1 dysregulation leading to PA tumorigenesis.42 Despite its standard classification and typical behavior as a “benign” neoplasm, PAs do feature a risk of malignant degeneration to carcinoma-ex pleomorphic adenoma (Ca-ex PA). Moreover, in a small set of subset of patients, PAs may feature metastatic potential in the absence of histopathologic or cytologic markers of malignancy. The actual rate of malignant degeneration of PAs is unknown, with a reported overall rate of 6.2%.43 The likelihood of malignant degeneration is correlated to increasing duration of tumor presence, with rates of transformation to Ca-ex PA increasing from 1.6% in tumors present for less than 5 years to 9.6% among patients with PAs for more than 15 years.44 The precise mechanism of malignant transformation has yet to be elaborated, but recent work has begun to elucidate the factors involved and holds the potential for the future development of molecular diagnostic and treatment modalities targeting progression to Ca-ex PA. Although focal capsular invasion or capsule absence has been implicated in the tendency of PAs to recur, such histologic features do not correlate with propensity for malignant degeneration. Transformation to Ca-ex PA involves overexpression of the p16 tumor suppressor protein in the cytoplasm with corresponding decreased nuclear and p16 promoter methylation.45 Quantitative promoter methylation of RASSF1 is a statistically significant epigenetic biomarker of malignant evolution of PAs.46 The influence of fibroblast growth factor receptor 2 on myoepithelial cells has been linked to neoplastic progression of PAs to carcinoma.47 The Wilms tumor 1 gene protein is also a reliable and specific marker for myoepithelial neoplasticity in PAs.48 Additional events implicated in malignant transformation of PAs include overexpression of CDK4, HMGA2, and MDM2.49,50 In addition to frank malignant transformation, PAs may also feature metastatic potential in the absence of histologic characteristics of malignancy. The histologic and molecular factors associated with nonmalignant metastatic PA are unknown, but this “submalignant” metastatic potential may be associated with a propensity for early vascular invasion in the setting of perlecan myxoid stroma facilitating hematogenous spread.51,52 Warthin tumor is the second most common salivary gland neoplasm, representing approximately 4 to 11% of all salivary gland tumors.53 It is also known as papillary cystadenoma lymphomatosum or adenolymphoma, and it occurs almost exclusively in the parotid gland. Patients tend to present in their sixth decade of life. A strong association with cigarette smoking has been demonstrated. Men have traditionally been affected more than women; however, recently the male-to-female ratio has decreased, possibly because of the increasing incidence of smoking in women.54,55 Bilateral involvement occurs in 10% of cases and may either be synchronous or metachronous in nature.56 Patients frequently present with an asymptomatic mass, but pain, swelling, and inflammatory changes can acutely manifest. Grossly, Warthin tumors are encapsulated and have a smooth or lobulated surface. Sectioning reveals papillary cystic spaces with white nodules of lymphoid tissue occasionally visible on the cyst walls. Microscopically, Warthin tumor is characterized by bilayered oncocytic epithelial cells arranged as papillary projections lining cystic spaces. A defining feature is the presence of a prominent lymphoid stroma. The lymphoid component is polyclonal in nature, consisting of predominantly T lymphocytes with a smaller number of B lymphocytes. Follicles with germinal centers are also present. The pathogenesis is controversial; however, it is generally thought that the epithelial component of the tumor represents the neoplastic proliferation of salivary ducts that have been entrapped during the course of embryologic development.57 Imaging can be a useful adjunct in the preoperative work-up of suspected Warthin tumor, but no investigation is mandated. With US examination, these tumors appear rounded or lobulated and may demonstrate cystic change.58 MRI and CT may both be used to define the tumor extent, although MRI is superior in differentiating soft tissue planes. On MRI, the cystic foci appear hyperintense on T2 weighting and the lesion does not enhance following injection of intravenous contrast.59 Warthin tumor, as well as oncocytomas, demonstrate increased technetium-99m uptake, while most other salivary neoplasms are cold or show normal uptake.60 The recurrence rates reported in the literature ranges from 1 to 12%,55,61,62 with superficial parotidectomy being the most common surgical approach. Incomplete excision and multicentricity have been identified as predictors of recurrence.63 However, in some cases recurrent tumors simply represent residual multicentric foci of tumor. The role of radiation therapy in the treatment of salivary gland PAs is limited, but such treatment may be useful in the following circumstances: positive margin status at surgical resection, unresectability of primary tumor, or multifocal recurrence following surgical extirpation.64 Basal cell adenomas are benign salivary gland epithelial neoplasms accounting for roughly 1 to 2% of all salivary gland tumors.65 These tumors are rarely found in minor salivary glands, with the majority occurring within the parotid gland. Clinically, basal cell adenomas present as firm, mobile, asymptomatic masses that slowly increase in size over a period of several months or years. The excised tumors are solid and well-demarcated. Grossly, the cut surface is grayish-white to yellow-brown and frequently resembles an enlarged lymph node. Tumors found in the parotid gland often are encapsulated, whereas those originating from minor glands are not. Histologically, basal cell adenomas are composed of isomorphic basaloid cells and interlaced trabeculae with a well-defined, prominent basement membrane. These neoplasms can be subdivided according to their histopathological features into the following categories: solid, trabecular, tubular, or membranous. The solid pattern predominates, although individual tumors commonly display a combination of the previously mentioned growth patterns.65 Discrimination of basal cell adenoma from other salivary tumors, particularly PA, basal cell adenocarcinoma, and adenoid cystic carcinoma (ACC), can be difficult. An intact basement membrane and lack of a chondromyxoid stromal component help distinguish basal cell adenoma from PA. In addition, basal cell adenomas show uniform cellular arrangement without the loss of polarity typically observed in PAs.66 The histologic features that are helpful in identifying malignant basal cell adenocarcinoma include cellular atypia, mitotic figures, perineural or vascular invasion, and a microinvasive growth pattern. Similarly, ACCs demonstrate cellular atypia, mitotic figures, perineural or vascular invasion, necrosis, and a finger-like matrix material while basal call adenomas lack these features.67,68 Oncocytomas, also known as oncocytic adenoma or oxyphilic adenoma, are uncommon, benign tumors that occur preferentially in the parotid gland and less frequently in the submandibular gland. Minor salivary gland oncocytoma is rare, accounting for less than 1% of all salivary gland tumors.69 Most affected patients are older than 50 years, with a peak incidence reported between 60 and 80 years of age. No gender predilection for oncocytomas has been demonstrated.70 These tumors usually appears as a painless, slow-growing mass in the affected gland. Oncocytomas are well-circumscribed, encapsulated, firm nodules that rarely exceed 5 cm in size.71 The cut surface has a tan-brown color and is usually solid in appearance; however, some tumors show areas of cyst formation. Parotid oncocytomas selectively incorporate technetium-99m pertechnetate and appear as hot spots on radionucleotide imaging.72 The tumor is microscopically characterized by metabolically transformed large epithelial cells with vesicular nuclei and innumerable mitochondria. The abundant mitochondria result in a deeply eosinophilic, finely granular cytoplasm.69 The oncocytic cells are arranged in solid nests of sheets.71,73 Diagnosis can be challenging as other salivary gland tumors have the potential to undergo oncocytic metaplasia and mimic oncocytomas. Cystadenomas are rare, benign epithelial neoplasms that occur predominantly in the minor salivary glands. The lip is the most commonly involved site, but cystadenomas can also develop in the minor salivary glands of the buccal mucosa, tongue, and palate.74–76 Cystadenomas are classified into papillary and mucous subtypes, with the former being the most common.77 On pathologic examination, the tumors appear as smooth nodules that are well-circumscribed, or even encapsulated, by a rim of fibrous tissue.74 Histologically, these lesions are characterized by unicystic or multicystic growth. The papillary subtype demonstrates intraluminal papillary projections lined by cuboidal to columnar cells with limited solid areas. Neoplastic proliferation with variable differentiation is noted in the epithelial layer lining the cysts. This tumor demonstrates microscopic similarities to Warthin tumor; however, papillary cystadenoma lacks the lymphocytic stroma and conspicuous lymphoid follicles observed in Warthin tumor.75 Canalicular adenomas are rare neoplasms that occur almost exclusively in the intraoral minor salivary glands. These tumors demonstrate a predilection for the upper lip and are the second most frequent benign salivary gland tumor at this site, followed by PA. Roughly 70% of tumors can be localized to the upper lip, with the buccal mucosa and palate representing the other anatomic sites most frequently involved.78,79 This tumor is usually present in older adults and demonstrates a slight female predominance.77 It manifests similarly to other benign salivary neoplasms as a slow-growing, asymptomatic submucosal mass. This lesion is usually well-circumscribed, but may appear unencapsulated if the tumor violates its capsule. The overlying mucosa is typically healthy, though ulceration has been reported.80,81 On microscopic examination, canalicular adenomas consist of columnar epithelial cells that form branching, interconnecting cords of single- or double-cell layers. The stroma is loose, poorly collagenized, and highly vascular.82 Unlike most other salivary gland tumors, canalicular adenoma can be multifocal in nature. Multifocality can manifest clinically as distinct lesions or microscopically as foci of tumor cells with intervening, normal-appearing salivary gland tissue. Multifocal lesions have been reported to occur in approximately 20% of cases.77 Despite the fact that this tumor can be characterized by multicentric foci of tumor cells, the recurrence rate remains low and the prognosis is excellent with complete surgical excision.79 The multifocality of these tumors should not be misinterpreted as invasive carcinoma. Recurrent tumors may represent growth of residual microscopic islands of disease after removal of clinically evident masses.83 For this reason, clinicians should consider prolonged postoperative follow-up for patients who have undergone resection of canalicular adenoma, particularly those who initially present with multiple lesions. Myoepitheliomas are rare, benign salivary gland neoplasms, accounting for less than 1% of all salivary gland tumors.84 These tumors develop predominantly in the major salivary glands and less often in the minor salivary glands of the oral cavity. Patients suffering from benign myoepithelioma usually present with a painless mass of long duration. Those affected are typically older adults, with both sexes being equally represented.85 These tumors have a smooth external surface and are typically well-demarcated from surrounding tissue. Histologically, the tumor cells show wide morphologic variation and are composed of spindle, plasmacytoid, epithelioid, and clear cells exhibiting myoepithelial differentiation. The cell type does not appear to have any influence on biologic behavior patterns; however, it has been suggested that the clear-cell type should be regarded as potentially malignant.84,86 Immunohistochemistry can be helpful in identifying tumors of myoepithelial origin. Vimentin and S-100 are sensitive but nonspecific markers for myoepithelial tumors. α-SMA or calponin plus vimentin represent the optimal staining protocol, as neoplastic myoepithelial cells are rarely fully differentiated.87 Differentiation of benign from malignant salivary gland myoepithelial tumors may be challenging. Malignant myoepitheliomas, also known as myoepithelial carcinomas, exhibit extensive local growth and infiltration of adjacent tissues. In contrast, benign myoepitheliomas are typically well-circumscribed and encapsulated. Further, cellular atypia, necrosis, and high counts of mitotic figures are histologic features suggestive of malignancy.88 Malignant transformation is rare.84 Ductal papillomas are rare, benign tumors that predominantly occur in the minor salivary glands. Clinically, these tumors present as raised, submucosal masses most frequently localized to the lip and buccal mucosa.89 While papillary characteristics can be a histologic feature of several other tumors of excretory duct origin, papillary growth of the ductal epithelium is the primary component of ductal papillomas. According to cell type, morphology, and location this tumor can be subdivided as follows: sialadenoma papilliferum, inverted papilloma, and intraductal papilloma.90 Lymphadenomas are uncommon salivary epithelial tumors. The majority of these tumors originate in the major salivary glands. Adults above the age of 50 years are most commonly affected and typically present with an asymptomatic mass that has been present for a prolonged period with slow enlargement. Grossly, lymphadenomas tend to be well-circumscribed and encapsulated. On pathologic sectioning, they are homogenous and grossly cystic, with a gray-tan to yellow cut surface. While sebaceous glands do arise from intralobular ducts in normal salivary tissue, neoplastic proliferation is rare. Histologically, these tumors are usually characterized by an epithelial component with sebaceous differentiation and prominent, reactive lymphoid proliferation. The lymphocytic infiltrate is a defining feature composed of mixed T and B lymphocytes. Germinal centers may or may not be present in the lymphoid stroma.91 Occasionally, tumors may lack epithelial sebaceous differentiation.92,93 Interestingly, this subtype demonstrates a female predominance whereas tumors with sebaceous differentiation more commonly affect men. This may be attributed to the higher number of sebaceous glands associated with facial hair in men. Malignant transformation is rare but has been reported to occur in the epithelial component.91 Sebaceous adenomas are benign epithelial tumors that comprise roughly 0.1% of all salivary gland tumors.94 Sebaceous adenomas are most common in adult males and preferentially affect the parotid gland.95 Rarely, sebaceous adenoma originates from a minor salivary gland. As with most other benign salivary gland tumors, patients frequently note a slow-growing mass in the affected gland. Sebaceous adenomas are typically well-circumscribed and sharply demarcated from surrounding, normal tissue. They can be either solid or cystic.96 On microscopic examination, cells demonstrating sebaceous differentiation without atypia are arranged in nests forming acinar and duct-like structures with intervening fibrous stroma. Areas of squamous differentiation with minimal atypia and pleomorphism are often present.97,98 Oncocytic metaplasia has been reported, although the etiology is unclear.98,99 Lipani et al proposed the following criteria for establishing the diagnosis of sebaceous adenoma: (1) a well-circumscribed tumor with organoid pattern, (2) differentiated sebaceous lobules demonstrating irregularity of size and shape, (3) lobules containing varying proportions of both mature sebaceous cells and small germinal cells that may be arranged in an irregular pattern, and (4) lack of dilated excretory ducts or a common excretory duct.100 Salivary gland cancers are relatively rare, accounting for only 20% of salivary gland tumors and 5% of head and neck malignancies.1 The incidence rate is estimated to be three new cases per 100,000 people per year worldwide, with an average of 2500 new cases per year in the United States. The parotid gland is the most common site for salivary gland cancer; however, only 20 to 25% of parotid tumors are malignant compared with 40% of submandibular tumors, 50% of minor salivary gland tumors, and 90% of sublingual tumors.101 Salivary gland cancer comprises the most heterogeneous group of cancers in the body, with up to 24 different cancer subtypes occurring within the glands. The relative rarity and significant diversity of these cancers prevent broad application of standardized therapy; therefore, it requires multidisciplinary cooperation and decision making to individualize the best course of care for a given patient. Vander Poorten et al have developed a prognostic index for salivary gland malignancy based on a Cox regression analysis model; the most important predictive factors for malignancy are facial nerve paralysis (coefficient = 0.91), facial pain (0.62), and skin involvement (0.63) followed by T stage (0.44) and nodal involvement (0.45).102 Overall, the most powerful determinant of survival across histologic subtypes is regional lymph node metastasis.103 Rates of distant metastasis for salivary gland malignancies are quite high as compared with other types of head and neck cancer, varying from 20 to 50% based on histologic subtype and gland of origin.104 Distant metastases are the most common cause of death in patients with salivary gland malignancies, most commonly occurring in the lungs (80%), bone (15%), and liver and others sites (5%).105 The risk of locoregional and distal recurrences of salivary gland cancer ranges from 15 to 80% at 5 years but is strongly influenced by the underlying tumor type and stage. Patients with recurrent salivary gland cancer can be successfully salvaged for cure with aggressive multimodality therapy in many cases or effectively palliated to improve locoregional control and provide symptomatic relief in the event of distant disease. A key feature distinguishing salivary gland malignancies from other malignant tumors of the head and neck is their propensity for late (more than 5-year posttreatment) recurrence, with more than 20% of patients experiencing late recurrence and the majority of those subsequently succumbing to their disease. This phenomenon is most commonly referenced in the context of ACC; however, a recent study demonstrated no statistically significant correlation between late salivary gland tumor recurrence and malignant subtype.106 Because of the high risk of late recurrence, salivary gland malignancies necessitate lifelong follow-up by a head and neck surgeon. The appropriate role of chemotherapy and biologic agents for salivary gland cancers has yet to be comprehensively delineated. Table 22.3 summarizes the management of primary salivary gland malignancies. Complete surgical excision with negative margins and without tumor spillage continues to be the primary therapy of choice for all salivary gland tumors. The likely extent of surgery can often be determined preoperatively if the tumor is classified as malignant by FNA and staged with physical examination and appropriate imaging. If preoperative FNA is indeterminate or benign, the surgeon should plan to fully excise the mass with a negative margin but be prepared to extend the surgery based on intraoperative findings. Findings such as nerve encasement, extensive soft tissue invasion, or adenopathy should alert the surgeon to the possibility of malignancy. Frozen section analysis of the mass can be done if there is no risk of spillage to help determine if nerve sacrifice and/or neck dissection is indicated. The need for adjuvant therapy is largely dependent on the final pathology of the surgical specimen. Pathologic findings that suggest the need for adjuvant therapy include: • Tumor grade: intermediate (mucoepidermoid carcinoma [MEC], ACC, Ca-ex PA) or high-grade (salivary duct carcinoma, adenocarcinoma) tumors that are T1 or greater • Tumor size: T3 or greater for any grade tumor • Extraparenchymal extension • Neural/perineural invasion • Multicentric tumor • Lymph node metastasis • Lymphovascular invasion • Close (less than or equal to 1 mm) or positive margins Given the limited correlation between tumor grade and biologic behavior, a growing body of research has focused on whether molecular tumor markers have prognostic significance. While no salivary tumor marker is frequently used in clinical practice, the following are among the most studied and/or most promising: 1. Ki-67 is a cellular protein that is involved in cellular transcription and has been used as a marker of cell proliferation. It has been shown repeatedly that MECs and ACCs that express a higher level of Ki-67 have a worse 5-year survival, which has been validated in multivariate analysis.107–109 However, one recent study failed to show that Ki-67 was an independent prognostic indicator in MEC when newer tumor markers, such as MEC translocated 1–mastermind-like 2 (MECT1-MAML2) (see below), were included in the analysis.110 Various cutoffs for expression have been employed, with 5% expression being the most frequently employed. At this point, Ki-67 staining may be considered a useful tool in the evaluation of the aggressiveness of some salivary gland neoplasms. 2. p53 is a tumor suppressor protein that helps control the cell cycle whose mutation is widely implicated in a variety of human neoplasms. Despite this observation, and the fact that it is the most studied of the salivary gland tumor markers, p53 has not been consistently found to be altered in salivary malignancies, with the p53 staining ratio varying greatly among studies. Although p53 accumulation has been shown in some studies to be an independent prognostic indicator of 5-year survival in MEC, several other studies have been unable to corroborate this finding.110–113 There have been similar incongruent findings in ACC and Caex PA. At this point, there is no role for the use of p53 in the prognosis of salivary gland neoplasms.
Salivary Gland Tumors
Imaging of Salivary Gland Tumors
Fine-Needle Aspiration Biopsy of Salivary Gland Tumors
Benign Salivary Gland Neoplasms
Surgical Management of Benign Neoplasms
Benign Epithelial Tumors—Types
Pleomorphic Adenoma
Warthin Tumor
Basal Cell Adenoma
Oncocytoma
Cystadenoma
Canalicular Adenoma
Myoepithelioma
Ductal Papilloma
Lymphadenoma
Sebaceous Adenoma
Salivary Gland Cancer
Surgical Management of Salivary Gland Cancer
High-Risk Molecular Markers
< div class='tao-gold-member'>
Salivary Gland Tumors
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree