Ultrasonography (US) is the single-most valuable imaging modality in the evaluation of the thyroid gland. This review discusses the US appearances of thyroid nodules, emphasizing sonographic features associated with potentially malignant or, at the other end of the spectrum, likely benign nodules. Diffuse thyroid abnormalities have also been reviewed. The technique of ultrasound-guided fine-needle aspiration biopsy and the emerging role of elastography in characterizing thyroid nodules have also been addressed.
Thyroid nodules are very common; autopsy studies show that nearly half the population of the United States harbors thyroid nodules. However, only 4% to 8% of these nodules are palpable and detected clinically. Many more are discovered incidentally on a computed tomographic scan, magnetic resonance imaging, or ultrasound of the neck performed for an indication unrelated to thyroid disease. In recent years, there has been an explosion of investigation generated by the discovery of these incidental thyroid nodules. Despite the high prevalence of thyroid nodules in the general population, only 5% to 10% of nodules are malignant. The overwhelming majority of thyroid nodules are not true neoplasms but rather represent nodular hyperplasia (also called adenomatoid or colloid nodule). Thyroid cancer is uncommon: in 2008, there were 37,340 new cases diagnosed and 1590 patients died from the disease. Well-differentiated papillary thyroid carcinomas (PTCs) account for 75% to 90% of all thyroid cancers. It is clear from these statistics that one of the important challenges for imagers and clinicians is to identify potentially cancerous lesions and reassure the vast majority of patients harboring benign nodules.
Ultrasonography (US) is the single-most valuable imaging modality in the evaluation of the thyroid gland. Indications for thyroid US include evaluation for a palpable thyroid nodule or suspected thyroid enlargement and workup of thyroid nodules discovered incidentally. It should not be used as a screening test for the detection of nodules. In addition to nodule detection and characterization, US provides optimal guidance for fine-needle aspiration biopsy (FNAB), which, despite some limitations, remains the gold standard for the characterization of thyroid nodules.
This review discusses the US appearances of thyroid nodules, emphasizing sonographic features associated with potentially malignant or, at the other end of the spectrum, likely benign nodules. Diffuse thyroid abnormalities have also been reviewed. The technique of ultrasound-guided FNAB and the emerging role of elastography in characterizing thyroid nodules have also been addressed.
Technique and normal appearance
The thyroid gland is imaged using high-frequency linear transducers, 8 to 15 MHz, depending on the thickness of the patient’s neck. Gray-scale transverse and sagittal images are recorded for each lobe. Occasionally, in large patients, additional scanning with a 6-MHz linear transducer may prove beneficial. If the thyroid gland is enlarged, a curvilinear transducer may be used for better measurements.
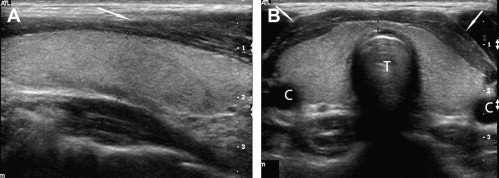
The normal thyroid has a homogeneous, medium gray echotexture ( Fig. 1 ). Anatomic landmarks are best defined on transverse sections: the thyroid gland is found between the common carotid artery laterally and the trachea medially.
Measurements of any detected thyroid nodule should be performed in sagittal, transverse, and anteroposterior dimensions with electronic calipers placed outside any visible halo.
US evaluation of thyroid nodules
Once a thyroid nodule is discovered, the single-most important next step is to decide whether an FNAB should be recommended. Although this procedure is relatively noninvasive, it is desirable to limit its use for nodules that are suspicious or indeterminate to minimize unnecessary costs and anxiety to the patient. In addition, there is a documented 5% false-negative rate for FNAB.
US evaluation of thyroid nodules
Once a thyroid nodule is discovered, the single-most important next step is to decide whether an FNAB should be recommended. Although this procedure is relatively noninvasive, it is desirable to limit its use for nodules that are suspicious or indeterminate to minimize unnecessary costs and anxiety to the patient. In addition, there is a documented 5% false-negative rate for FNAB.
US characteristics of thyroid nodules: a systematic analysis
To encourage a rationale approach to the management of thyroid nodules detected on US, several medical societies, including the American Thyroid Association (ATA), the Society of Radiologists in Ultrasound (SRU), and the American Association of Clinical Endocrinologists (AACE), have recently published a series of guidelines. The US features of thyroid nodules that should be analyzed are summarized in the Consensus Statement on thyroid nodules from the SRU and the AACE. They include nodule size and content (solid, complex, or cystic). For solid thyroid nodules, the following parameters should be evaluated: nodule echotexture, shape, borders (smooth or nodular), the presence and quality of intranodular calcifications, and the presence of a perinodular halo. Table 1 compares the sensitivity, specificity, positive predictive values, and negative predictive values of each of these sonographic criteria from 6 large studies, including a large retrospective study of 849 thyroid nodules recently conducted by the Korean Society of Neuro and Head and Neck Radiology Thyroid study group. Many of the statistics listed below stem from these articles and are summarized in Table 1 .
| Study | Number of Nodules | Clinical | Hypoechogenicity (%) | Shape Spherical/Taller Than Wide (%) | Spiculated Margins (%) | Microcalcifications (%) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivity | Specificity | PPV | NPV | Sensitivity | Specificity | PPV | NPV | Sensitivity | Specificity | PPV | NPV | Sensitivity | Specificity | PPV | NPV | |||
| Takashima et al | 259 | P & NonP | 83 | 49 | 40 | 89 | — | — | — | — | 72 | 63 | 44 | 85 | 36 | 93 | 70 | 78 |
| Kim et al , a | 155 | NonP | 26.5 | 94.3 | 68.4 | 73.5 | 32.7 | 92.5 | 66.7 | 74.8 | 55.1 | 83 | 60 | 80 | 55.1 | 83 | 60 | 80 |
| Papini et al , b | 402 | NonP | 87.1 | 43.4 | 11.4 | — | — | — | — | — | 77.5 | 85 | 30 | |||||
| Nam-Goong et al | 317 | NonP | 68.2 | 52.9 | 27 | — | — | — | — | — | — | — | — | — | 36.4 | 85.5 | 39 | — |
| Capelli et al , b | 701 | NonP | 79.1 | 53.3 | 15.1 | 96 | 83.6 | 81.5 | 32.4 | 97.9 | 47.8 | 74.3 | 16.4 | 93 | 73.1 | 69.2 | 20 | 96 |
| Moon et al | 849 | P & NonP | 87.2 | 58.5 | 60.7 | 86.1 | 40 | 91.4 | 77.4 | 67.4 | 48.3 | 91.8 | 81.3 | 70.7 | 44.2 | 90.8 | 77.9 | 68.8 |
Nodule Content: Cystic Versus Solid Nodules
Before the availability of high-resolution high-frequency transducers, the role of US was limited to distinguishing between cystic and solid nodules. Purely cystic nodules are anechoic. They are almost invariably benign and represent colloid cysts. Some colloid cysts contain echogenic foci with posterior reverberation or comet tail artifact ( Fig. 2 ). A subset of cystic nodules shows a lacelike or honeycomb pattern of multiple small cysts separated by thin septations ( Fig. 3 ). This pattern is strongly associated with a benign hyperplastic nodule and has been dubbed the “leave me alone” lesion. Consequently, purely cystic nodules, with or without comet tails, and cystic nodules with a honeycomb appearance do not need FNAB.
However, many cystic thyroid nodules have a solid-appearing component. Although these complex nodules are often referred for biopsy for concern that they represent a cystic papillary cancer, their most common underlying cause is a degenerated colloid nodule ( Fig. 4 ). Because these nodules contain avascular debris and fibrosis, they tend to yield scant or no follicular cells and are associated with a higher number of inconclusive FNAB.
Careful analysis of any solid area within cystic nodules is imperative to identify the rare papillary thyroid cancer (approximately 2.5%) with a large cystic component. Hatabu and colleagues described the “calcified nodule within a cyst,” a sign of papillary excrescences with microcalcifications protruding into the cyst, as specific for papillary thyroid cancer ( Fig. 5 ). Such an area should be specifically targeted during fine-needle aspiration.
Echotexture
The echotexture (or shade of gray) of solid nodules is another important criterion taken into consideration when analyzing nodules. The echotexture of the nodule is compared with that of the surrounding thyroid parenchyma and the strap muscle ( Fig. 6 ). Nodules are described as isoechoic (same shade of gray as the thyroid), hypoechoic (darker than the thyroid) or markedly hypoechoic (darker than the strap muscle). Hypoechoic and very hypoechoic nodules are classified as suspicious and referred for FNAB. Kim and colleagues found that 26.5% of malignant nodules were markedly hypoechoic (see Fig. 6 ) compared with only 5.6% of benign nodules. The underlying histology for these nodules is usually PTC, and it is postulated that the dense cellularity of PTC produces very few interfaces to the sound beam and hence the hypoechoic appearance. Follicular neoplasms, whether benign adenomas or follicular carcinomas, contain colloid, have a microfollicular structure, and usually display an echogenic or mixed echotexture. Pathologically, they are typically encapsulated and tend to be sharply demarcated from the surrounding thyroid parenchyma on US.
Shape
Moon and colleagues reported that an elongated shape as compared with a wide shape, defined as an anteroposterior to transverse ratio of 1 or greater, is highly specific (91.4%) for malignancy. These results confirmed the reports published earlier. In another series, nodules with a spherical shape (ratio of long to short axis <1.5) were found to be associated with an 18% risk of cancer. By contrast, a ratio of long to short axis greater than 2.5 was found to have a 100% negative predictive value for malignancy. It is speculated that cancers tend to grow across tissue planes and assume a spherical shape to maximize their oxygen supply, whereas benign lesions respect normal thyroid parenchyma.
Borders
Predictably, a spiculated or nodular border is associated with a higher probability of malignancy (see Fig. 6 ). Classically, PTC invades the surrounding thyroid tissue and is poorly encapsulated. In the series published by Moon and colleagues, 48.3% of thyroid cancers had spiculated margins and 32.5% had smooth borders, whereas 75.9% of benign nodules had smooth margins and only 8.2% were spiculated. These results confirm findings from previous studies. Demonstration of a refractive shadow from the edge of a solid nodule is another suspicious finding that warrants fine-needle aspiration.
Perinodular Halo
Some thyroid nodules are surrounded by a distinct hypoechoic halo. Although it was initially speculated that this hypoechoic rim represents thyroid parenchyma compressed by a slow-growing and therefore presumably benign process, correlation with histology has shown that follicular adenomas and carcinomas are well encapsulated and may display a well-defined thick hypoechoic rim. In fact, adenomatous (colloid) nodules can be incompletely encapsulated or poorly demarcated from the rest of the thyroid parenchyma. Therefore, the presence of a halo is not a particularly useful sonographic criterion to suggest a benign process.
Calcifications
Calcifications are detected in almost one-third of thyroid nodules. Microcalcifications are defined as punctuate echogenic foci measuring less than 2 mm. Because of their small size, they do not produce acoustic shadowing. Microcalcifications are thought to represent the psammoma bodies or calcified laminated nidus that are frequently found in PTC. The presence of microcalcifications in a solid nodule has a high specificity of 91.3% to 96.3% and a positive predictive value of 74.8% for malignancy; unfortunately, the sensitivity is only 29% to 51.4% ( Figs. 7 and 8 ).




