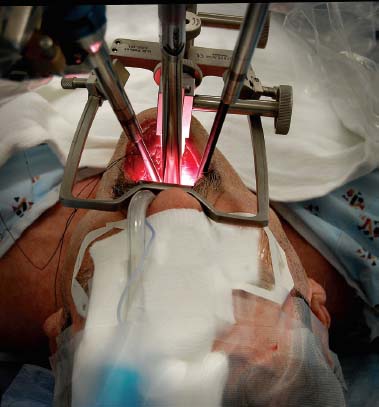
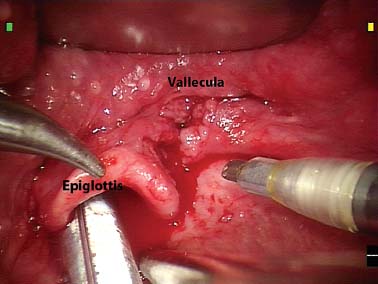
32 Core Messages • The surgical robot is an important tool for expanding the scope of minimally invasive surgery in the head and neck. • The principles for the proper oncologic management of head and neck tumors are unchanged. The goals of resection are to obtain clear surgical margins and maintain normal function whenever possible. • Exposure of the tumor remains the most challenging aspect of robot-assisted surgery of the head and neck. The surgeon should determine before proceeding whether there is a reasonable chance of achieving clear margins. The patient rarely benefits, and, in some circumstances, is harmed by partial tumor resection. • Close collaboration with pathology is mandatory. Minimally invasive tumor resection is not a new concept for head and neck surgeons. In 1893, U.S. President Grover Cleveland had an oral cavity cancer secretly resected transorally by surgeons on his yacht off the coast of New York. He survived and lived another 16 years. For tumors beyond direct transoral view, the operating microscope has been used for decades with cold instruments and subsequently with laser for tumor resection. Adaptation of robotic surgery for the head and neck now promises a significant opportunity to expand our minimally invasive capabilities. In 2003, investigators at Stanford University first documented the use of a robot in head and neck surgery in porcine models. Procedures performed included submandibular resections, selective neck dissections, a unilateral parotidectomy, and thymectomy. The only complication was one incidence of subcutaneous emphysema.1 Work began at the University of Pennsylvania in 2005 on transoral approaches as surgeons investigated proper robotic cart and instrument positioning to allow access to the larynx using mannequin models. Cadaver studies followed, demonstrating safe access to the larynx without significant damage to the teeth, mandible, or pharyngeal integrity. Canine studies then confirmed feasibility, safety, and adequate hemostasis during supraglottic laryngectomy. Finally, the procedure was tried in humans as part of a clinical trial under institutional review board supervision. Elsewhere in 2005, 11 endorobotic submandibular gland resections were successfully performed at the Medical College of Georgia, with an average operating time of 48 minutes.2 Canine and porcine models were also successfully operated on by using transoral approaches at the Walter Reed Army Medical Center in Washington, DC, in 2005.3 The acronym TORS (transoral robotic surgery) was coined in 2006 after Weinstein and O’Malley reported the first three human patients with tongue base cancers treated with this innovative technique.4 In early 2007, other medical centers began to adopt the transoral robot-assisted procedure. At each site, work was originally performed under institutional review board supervision in a clinical trial setting. Reports documenting feasibility, efficacy, and safety began to emerge, indicating that the procedures were reproducible in other settings. In early 2010, the Food and Drug Administration granted approval to use the da Vinci surgical robot for the resection of benign and malignant lesions of the oral cavity, oropharynx, hypopharynx, and larynx, stages T1 and T2. The preoperative work-up for a patient undergoing TORS is similar to that for any patient with head and neck cancer (HNC) and includes physical examination, direct laryngoscopy and biopsy, imaging, metastatic work-up, and appropriate laboratory analysis. Many surgeons also insist that they personally perform a diagnostic examination under anesthesia to assess the feasibility of TORS. The rationale is that the robot is an extremely limited resource and the additional examination under anesthesia helps ensure that only those patients whose tumor is accessible by TORS will be scheduled for the procedure. Exclusion criteria specific for TORS management of an oropharyngeal neoplasm are similar to the exclusion criteria for other transoral procedures.5,6 These include the following: • Anatomic characteristics that make exposure and visualization of the tumor impossible via the transoral approach (e.g., trismus and ill-defined margins). • Lesions fixed to the lateral or posterior pharyngeal wall, indicating deep neck invasion into the parapharyngeal space. • Lesions intimately associated with the carotid artery, internal jugular vein, or prevertebral fascia as evidenced by physical examination or imaging. • Skull base invasion. • Mandibular invasion. • Stage IVC disease, except for curable distant metastasis. • Having a retropharyngeal internal carotid artery in which the artery is located directly behind the tonsillar fossa (a contraindication for TORS radical tonsillectomy but not for the resection of other oropharyngeal sites). • Medical contraindications for either general anesthesia or transoral surgery in which an open wound heals by secondary intention (e.g., the need for chronic anticoagulation). • Bilateral deep tongue base invasion. The da Vinci surgical system is used. The manipulator unit has three laterally placed instrument arms and a centrally located endoscopic arm. For base of tongue (BOT) and supraglottic laryngeal resections, a binocular endoscope angled at 30 degree is positioned in the central arm. For a radical tonsillectomy, a 0-degree binocular endoscope is preferred. Operating instruments commonly include a 5-mm monopolar electrocautery, 5-mm Maryland dissector forceps, 8-mm bipolar scissors, 5-mm needle driver, and 5-mm Debakey forceps. The laryngoscopic clip applier is typically used by the assistant instead of the robotic clip applier to avoid an instrument change on the robotic arms (Fig. 32.1). The surgeon should be prepared that the setup for robotic cases will take extra time initially. As familiarity grows for the surgeon and operating room personnel setup times decrease rapidly. The operation is performed under general anesthesia with nasotracheal intubation. The patient is positioned with the head 180 degrees away from the anesthesia team. Exposure of the tumor is accomplished before moving the robotic cart to the bedside. The teeth are protected with a gauze or molded thermoplastic sheeting. The tumor is exposed with an oral retractor; either the Crow-Davis mouth retractor or the Feyh-Kastenbauer laryngeal retractor is used (Fig. 32.2). Distraction of the tongue outward is accomplished with a heavy silk suture. Exposure of the operative site is often the most challenging portion of the TORS procedure. The surgeon should be willing to try different retractors, different blades, and different tongue positions as required to obtain optimal exposure. The retractor is suspended from the surgical bed by using a heavy endoscope holder to facilitate hands-free exposure. Figure 32.1 Robotic instruments (5 mm): (from top) Schertel forceps, Maryland dissector, Debakey forceps, and needle driver. Figure 32.2 Feyh-Kastenbauer retractor postioned and suspended. Note instrument position: camera midline with working arms on sides in triangular configuration. The scrub nurse is positioned to the patient’s side, and the surgical assistant is seated at the patient’s head. An active and attentive surgical assistant is essential for TORS. The assistant’s job is to suction smoke and blood, to apply countertraction at the surgical site, to help with exposure, and to place ligaclips on prominent vessels. The robotic cart for the da Vinci surgical system is positioned on the side opposite the scrub nurse at a 20- to 30-degree angle from the operating room table. The operating console is positioned at some distance away from the patient. The patient is prepped and draped as indicated. Once the robotic cart is positioned, the robotic arms are moved to the oral cavity with the video endoscope centrally and the surgical arms coming in on either side of the endoscope in a roughly triangular arrangement. Because of space limitations, only two of the three robotic operating arms are typically deployed. We prefer the 5-mm monopolar cautery and Maryland dissector as the instruments of choice. Occasionally, the third arm is used to provide static traction at the surgical site. • Make an incision through the buccal mucosa at the level of the pterygomandibular raphe between the upper and lower molars by using a 5-mm spatula cautery. This landmark is used to guide the surgeon to a dissection plane between the pharyngeal constrictor muscle, which becomes the lateral margin of tumor resection, and the buccopharyngeal fascia. • Use the 5-mm Maryland forceps to grasp and medially retract the incised buccal mucosa. • Develop a plane along the lateral aspect of the pharyngeal constrictor muscles and identify the pterygoid musculature laterally. • Dissect to the level of the styloglossus and stylopharyngeus muscles. • Transect the soft palate as indicated by the degree of cancer involvement. Dissect through the soft palate musculature to the level of the prevertebral fascia. • Elevate the constrictor muscles off the prevertebral fascia by using blunt dissection with the 5-mm spatula cautery. • Identify and divide as necessary the styloglossus and stylopharyngeus muscles. • Reconfirm the position of the carotid artery via imaging and by assessing for carotid pulsations. Clip any transversing veins and arteries. Attempt to protect the thin layer of fat in the parapharynx around the carotid artery and to prevent communication into the neck. • At the level of the BOT, incise across the posterior floor of the mouth to the lateral tongue mucosa. The extent of the BOT resection is based on the extent of the tumor, with the goal of achieving negative margins. Identify and preserve the lingual artery unless there is gross tumor involvement. • Resect the posterior pharyngeal wall from the inferior margin to the level of the soft palate. • Following resection, the tumor is oriented for pathologic evaluation and margins are taken. • Remove robotic instruments and assess hemostasis. • Relax and then reopen retractors to assess for occult bleeding. • Expose the vallecula inferior to the tumor (Fig. 32.3). • Make an initial inferior horizontal cut at the level of the vallecula. This allows determination of the inferior extent of the tumor and aids in determining the appropriate depth of the resection. • Next, adjust the retractor to allow the superior and lateral cuts. The end of the retractor blade should be placed anteriorly with just enough room to visualize the anterior extent of the gross tumor and to expose as much of the inferior extent of the tumor as possible. • Make a mucosal cut at the anterior margin and allow the tumor to fall posteriorly into the field of view. Grasp the normal soft tissue at the edge of the specimen and place it under tension for the remainder of the dissection. • Make the medial and lateral cuts as defined by the extent of the gross tumor. Identify and preserve, as appropriate, the dorsal lingual artery, the lingual artery trunk, and the hypoglossal nerve. • Connect the superior cuts to the inferior cuts at the depth defined by the initial tissue incisions to perform an en bloc resection with clear surgical margins. • Orient the tumor for pathologic evaluation. • Irrigate the wound bed and control for hemostasis with cautery or hemoclip application. • Remove all robotic instrumentation and retractors and assess for inadvertent trauma.
Robotic Surgery for Head and Neck Neoplasms
History of Robotic Surgery in the Head and Neck
Surgical Technique
Preoperative Evaluation
Instruments and Set Up
Operative Procedures
Transoral Robotic Surgery for Radical Tonsillectomy
Transoral Robotic Surgery for Base of Tongue Resection
< div class='tao-gold-member'>
Robotic Surgery for Head and Neck Neoplasms
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree