Introduction
Fungi are ubiquitous organisms. Most fungi are not pathogenic to man with only about 50 species known to be capable of invading man and less than a dozen known to cause fatal infections. Fungi that affect humans can be either pathogenic or opportunistic in nature. The difference between these two divisions is that opportunistic fungi are incapable of infecting healthy hosts, while pathogenic forms can infect both immunocompromised and non-immunocompromised patients.1
Usually, fungi like Aspergillus cannot actively penetrate undamaged and intact mucus membranes and skin, as they lack keratolytic enzymes.2 Body defences also help to keep these fungi in check, but even minor disturbances such as change in acid–base balance, lowered body resistance, atopy or ingestion of an antibiotic can disrupt the delicate balance of holding fungi in check, thus causing paranasal mycosis.3
Paranasal sinus mycosis is a relatively new area of interest not only for otorhinolaryngologists but also for pathologists, immunologists, and mycologists. It can affect both immunocompetent as well as immunocompromised hosts, especially in this era of rampant use of antibiotics. The disease in an individual depends on a complex interplay between environmental load of fungus, local tissue condition, and the immune status or atopy of the host.
Global and Indian Historical Background
The first case of fungal sinusitis was reported way back in 1791 when Plaignaud reported a case of possible fungal sinusitis in a 22-year-old soldier with maxillary pain having “fungus tumor”, which was said to be cured by cautery.4 The first case of primary Aspergillus infection of the paranasal sinuses in an otherwise healthy individual was reported by Oppe in 1897.5 The Frenchman Texier6 was the first to exclude the syphilitic origin to mention the possible dental origin and to recognize a “pseudo tumoral” form of sinus Aspergillosis in 1906. Aspergillus granulomas were first reported as the most common cause of unilateral proptosis in Sudan by Milosev in 1969.7 Jahrsdoerfer et al8 reviewed 103 cases from the world literature other than in Sudan and noted a mortality rate of 16% with Aspergillus sinus infection. In 1980, McGill et al 9 reported four immunocompromised patients with a different type of disease that was more aggressive than previously observed paranasal mycoses and termed it “fulminant aspergillosis”. The first report of human rhinocerebral mucormycosis was made by Paltauf10 in 1885. In 1943, Gregory et al11 described the clinical triad of diabetes mellitus, orbital infection, and meningoencephalitis with mucormycosis. The first reported survival of this rapidly fatal disease was described by Harris12 in 1955.
With increasing awareness, fungal sinusitis is being recognized more and more in India also.13–15 The hot and moist climate of India may be the reason for development of fungal infection. Species of Aspergillus are especially prevalent in infected grain or decaying vegetation in agricultural areas of our country. Farmers and others handling these products may be exposed to this fungus, especially if they are exposed to dust from hay, grains, straws, corn, and animal dander.16 This can explain high number of cases being reported from India.
Categorization of Fungal Rhinosinusitis
Fungal rhinosinusitis comprises a spectrum of diseases ranging from a benign non-invasive form to an aggressive invasive type. It can be categorized according to tissue invasion and host characteristics.
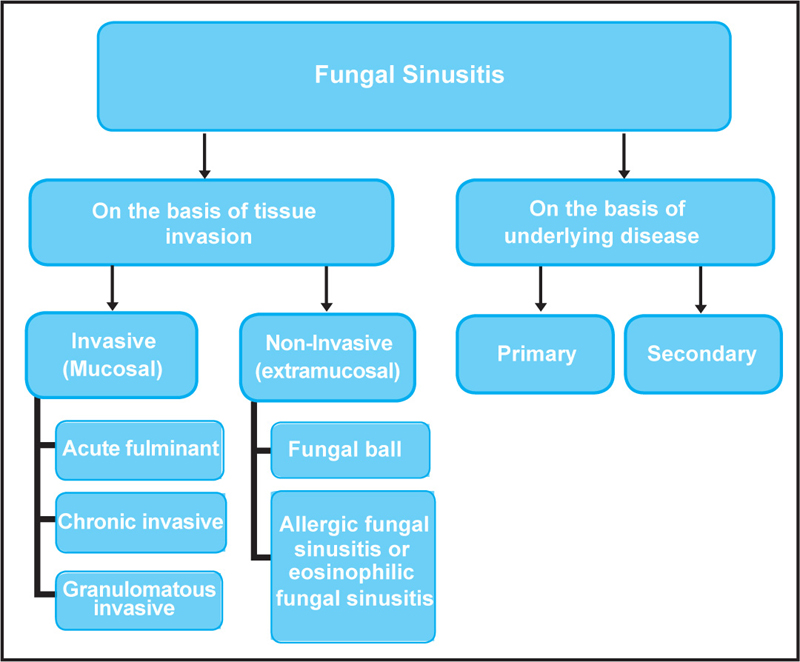
Based on tissue invasion, fungal sinusitis can be grouped into two subtypes, invasive/mucosal/penetrating fungal sinusitis and non-invasive/extramucosal fungal sinusitis (Figure 1). Hora17 recognized these two discrete forms way back in 1965. These two subtypes are discussed in detail in the subsequent sections in this chapter.
Fungal sinusitis may also be classified based on the host status into primary or secondary infection. Primary infection is seen in an otherwise healthy person and mostly manifests as allergic fungal sinusitis, fungal ball, granulomatous fungal sinusitis (most of the cases), and chronic fungal sinusitis (some cases). Secondary infection is seen in immunocompromised host and usually manifests as invasive fulminant sinusitis. The primary cases can be due to local anatomical or functional problems in the sinuses. High concentration of atmospheric fungal spores in hot and dry climate is thought to be the predisposing factor for primary disease.18
Invasive Fungal Sinusitis
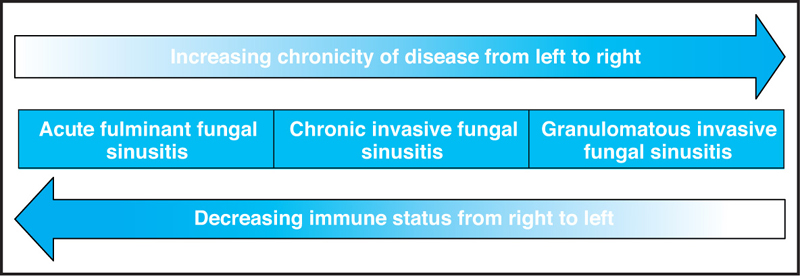
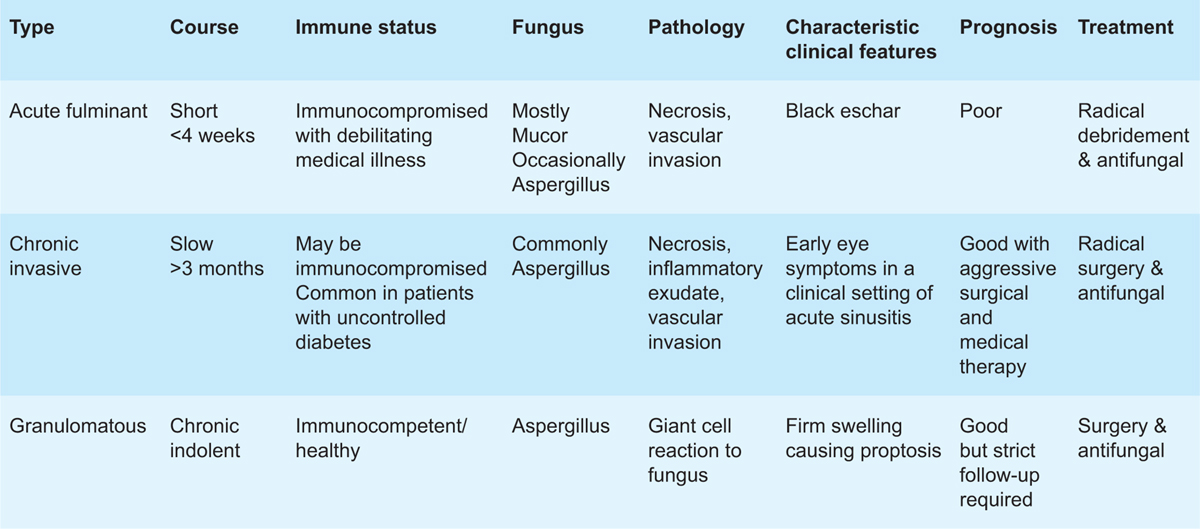
Invasive fungal sinusitis (IFS) consists of a spectrum of diseases dependent on the immune status of the patient (Figure 2). On one extreme is the immunocompromised patients who develop acute fulminant fungal sinusitis, which has very poor prognosis. On the other extreme is immunocompetent patients who develop granulomatous pathology. In between lie the patients with diabetes developing similar disease as acute fulminant but with a chronic presentation. A comparison of clinically relevant aspects of various types of invasive fungal sinusitis is given in Table 1.
Table 1 Comparison of Various Types of Invasive Fungal Sinusitis
Acute Fulminant Invasive Fungal Sinusitis
Acute fulminant invasive fungal sinusitis is found in immunocompromised individuals, usually secondary to some underlying systemic illness like diabetes mellitus and drugs or diseases affecting the immune system. The diseases that predispose to this condition include tuberculosis, leukemia, AIDS, sarcoidosis, renal failure, and lymphomas. Diabetic patients are known to develop unusual opportunistic infections. Neutrophils are important in host defense against mycotic infections19; in patients with less number of viable neutrophils (acute leukemia) or qualitative defects of neutrophil function (decreased phagocytic activity seen in diabetics), opportunistic fungi frequently cause infection. There is a strong correlation between absolute neutrophil counts below 500 cell/mL and invasive fungal disease.20
Therapy with antineoplastic or immunosuppressive drugs and prolonged injudicious use of steroids and antibiotics can also increase susceptibility to this disease. With more and more organ and bone transplants being done, fungal sinusitis is also being recognized in this group of patients.21 Patients with immunoglobulin disorders are not unusually susceptible to fungal infections, but conditions causing defective cellular immunity, such as lymphomas and immunosuppressive therapy, do predispose patients to mucormycosis and aspergillosis.22 Other predisposing factors include severe anemia, azotemia, severe trauma as well as any severely debilitating medical condition. This has been firmly established in several animal models.23–25
Etiopathogenesis
The etiologic fungi usually belong to the family Mucoraceae and genera Rhizopus, Mucor and Absidia. Some cases are also caused by Aspergillus species. Once the fungus enters the tissue, it invades the internal elastic lamina of local arteries, causing thrombosis.26 Thrombosis results in vascular insufficiency leading to dry gangrene. Progression of the disease from nose and paranasal sinuses leads to vascular embarrassment of orbital contents via ethmoid arteries. There is also invasion of lymphatics and regional nerves. The fungus commonly ascends to the apex of the orbit, and through the lateral wall of the cavernous sinus invades and obstructs the internal carotid artery. Because of the predilection of mucormycosis for arteries, complete cavernous sinus thrombosis often occurs after carotid artery occlusion.27 Once the internal carotid artery is obstructed, cerebral ischemia and death ensue. This entity has the highest morbidity and mortality of any of the sinus fungal infections.
Clinical Presentation
The clinical picture of mucormycosis has been described as an acute, fulminating infection with a violent and often catastrophic clinical course unless recognized early and managed with aggressive surgical and medical treatment.28 Acute invasive fulminant sinusitis may initially present with nonspecific signs like severe acute febrile illness associated with a bloody nasal discharge or pain and swelling of face and involved sinus.
The earliest lesion is crusting of the inferior turbinate or the cartilaginous septum that spreads rapidly to surrounding structures. At this stage, the patient may be asymptomatic or may mimic acute sinusitis with complaints of nonspecific rhinorrhea or nasal obstruction. Within days, the disease extends to involve the lateral nasal walls and the paranasal sinuses.
Examination of the patient in later stages shows facial swelling and gangrenous necrosis of nasal mucosa. There may be purulent nasal discharge with black necrotic crusts draining from the nose. There is tenderness over the involved sinus with characteristically present black areas of necrosis (called black eschar) (Figure 3). The eschar may be seen in the nose, medial maxillary bone, turbinate, and septum and may spread on to the hard palate. With further progression and involvement of the fronto-ethmoid complex there may be swelling and ecchymosis around the eye.
Extension to the orbit causes chemosis, proptosis, and decreased vision. Orbital signs of the disease include progressive loss of function of the second, third, fourth, and sixth cranial nerves with proptosis, ophthalmoplegia, ptosis, dilated pupils, and loss of vision. It may be confused with cavernous sinus thrombosis.
Intracranial extension occurs via vascular route or direct extension. Intracranial spread causes headache, lethargy, or even coma. The illness often progresses rapidly and may not respond to aggressive medical or surgical intervention. With greater clinical vigilance for these infections in patients at risk, there have been many reports of chronic form of mucormycosis. This may represent a certain clinical overlap with other mycotic infections known for slower progression.
Radiology
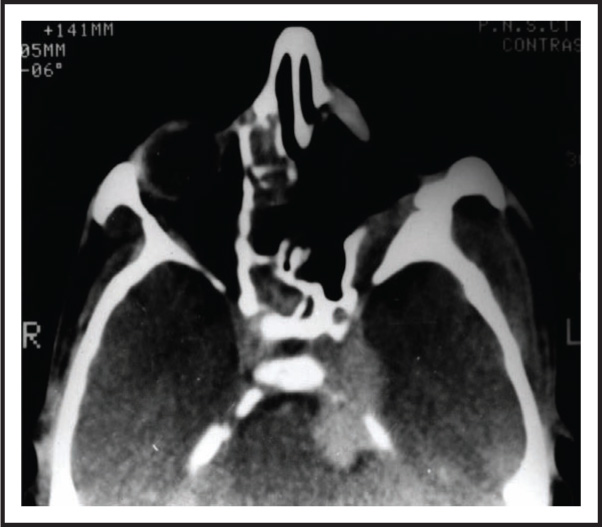
Computed tomography is the radiological investigation of choice in all cases of invasive fungal sinusitis. Though the findings on CT are nonspecific and do not help in diagnosis, CT is helpful in showing the extent of extracranial disease. MRI is a better modality than CT scan to know the extent of intracranial invasion.
Histopathology
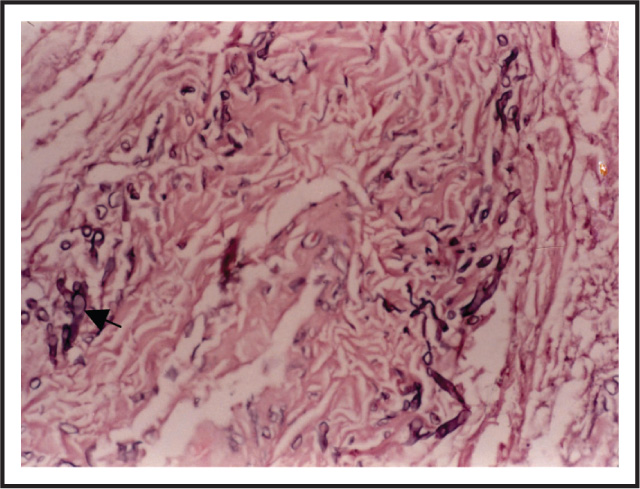
The confirmation of diagnosis is done by histopathology. Histology shows areas of necrosis, vasculitis, and thrombosis. In mucormycosis, abundant aseptate hyphae are seen within the vessel wall (Figure 4). Aspergillus appears as septate hyphae with acute branching. Special stains for fungus like Grocott-Gomori help in easy identification of fungal hyphae.
Treatment
As the disease is seen in immunocompromised individuals, the clinicians should have a very strong index of suspicion in all such patients with sinusitis so that the disease can be diagnosed at the earliest. The treatment should be initiated on strong clinical suspicion without even waiting for histopathological confirmation, as the progression of the disease is very rapid. The disease is treated with systemic, intravenous antifungal therapy. Liposomal amphotericin B is indicated in all patients with mucormycosis. Surgical clearance of the disease has to be radical with pre- and postoperative systemic antifungal therapy.
Granulomatous Invasive Fungal Sinusitis
Invasive granulomatous fungal sinusitis runs a chronic course. The patients are mostly immunocompetent. Chronic granulomatous is unique in its geographical distribution with most of the reports coming from Sudan7 and India.29 The disease more commonly involves ethmoid and medial wall of the orbit. Then it may extend to orbital apex and spread intracranially. Ocular symptoms may include diplopia and proptosis due to compression of extra-ocular muscles or by direct extension and tissue invasion.
On examination, the lesion in granulomatous fungal sinusitis is well-delineated, giving an appearance of encapsulation. The mass is usually firm to touch and sometimes has a consistency like cartilage. It is usually adherent to the underlying structures and requires sharp dissection for removal.
Histopathology
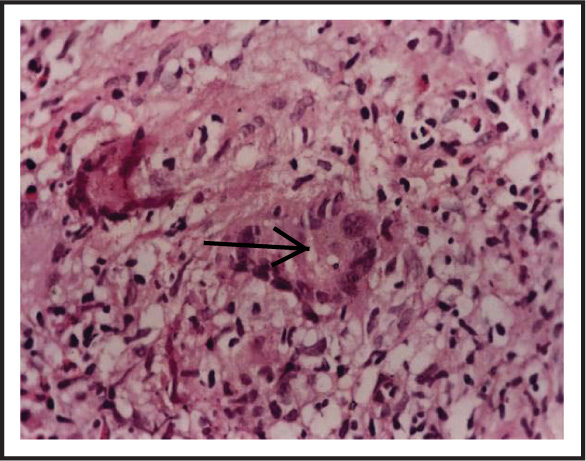
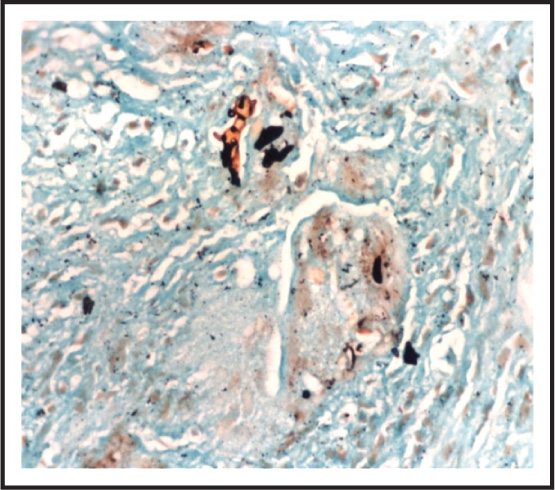
The diagnosis is based on histopathology, which shows chronic inflammatory exudate with multinucleated giant cell reaction to fungal hyphae. On routine staining with hematoxylin and eosin, fungal hyphae are seen as holes within the giant cells (Figure 5). The hyphae appear brown when stained with special fungal stains of Grocott-Gomori (Figure 6). Aspergillus flavus is implicated in most of the cases of chronic granulomatous invasive fungal sinusitis.
Radiology
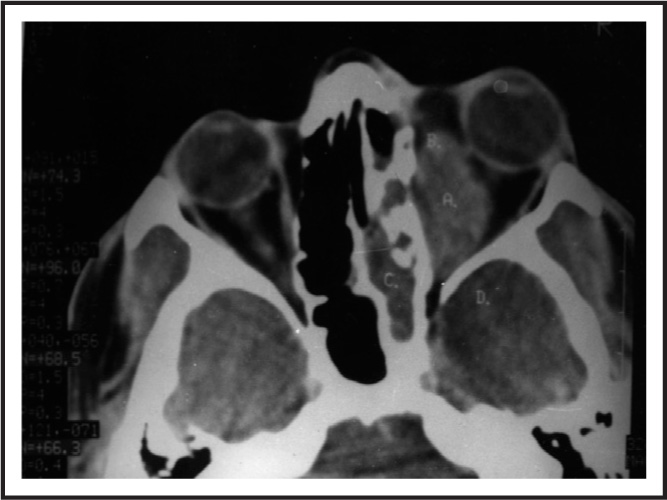
Computed tomography shows soft tissue mass of homogenous intensity within the involved sinus (Figure 7). Unilateral involvement of maxillary and ethmoid sinuses is the commonest with intra-orbital and/or intracranial extension. To see the intracranial extension, contrast-enhanced CT scan or MRI is helpful.
Treatment
There is a lack of consensus on the extent of surgery and duration of antifungal treatment. Management is by surgical clearance of the disease followed by antifungal therapy. The disease does not run a fulminant course, so radical surgery like orbital exentration can be reserved for patients not responding to antifungal therapy. Patients need a good endoscopic and radiologic follow-up after treatment to pick up residual or recurrent disease. The disease tends to recur if adequate postoperative antifungal therapy is not given (Figure 8). There are some reports of good response to long-term postoperative treatment with itraconazole.30
Chronic Invasive Fungal Sinusitis
Chronic invasive fungal sinusitis (CIFS) was described in 1997 by deShazo.31 CIFS is more commonly seen in patients with uncontrolled diabetes with or without metabolic acidosis, though it has also been reported in normal hosts as well. With early detection and control of diabetes, the disease runs an indolent course. It is characterized by tissue invasion, often resulting in bone destruction with extension of the disease to adjoining areas like pterygopalatine fossa, palate, orbit, or brain.32 Clinical differentiation from acute fulminant invasive can be done by a chronic course, absence of anesthetic nasal eschar, and the pattern of spread (direct as well as vascular route).
Histopathology
Histopathology shows fungal hyphae in the necrotic tissue with neutrophilic and eosinophilic inflammatory exudate. In some cases, vascular invasion is also seen.
Radiology
CT scans are essential as they have the capability of showing soft tissue details relative to the osseous walls and air spaces of the sinuses. This allows delineation of the extent of disease beyond the paranasal sinuses.33 Radiologic information is essential to know the extent of the disease and for the surgical planning as well as assessment of the therapy.