Revision Rhinoplasty
Richard E. Davis
Cosmetic nasal surgery remains one of the most effective and long-lasting procedures in the cosmetic surgery arsenal. A successful rhinoplasty not only creates a more attractive nose, it diverts attention to the eyes, making for a more harmonious and thus a far more beautiful face. Yet, while cosmetic rhinoplasty ranks among the most commonly performed cosmetic operations, few if any surgeons ever fully master its numerous subtleties and peculiar nuances. Without question, the delicate and complex three-dimensional nature of nasal anatomy, the precise and unforgiving tolerances of the nasal airway, and the lofty expectations of the typical rhinoplasty consumer make cosmetic rhinoplasty an extremely challenging surgical procedure. Moreover, the profound psychological importance of the face makes rhinoplasty a tremendously high-stakes emotional endeavor in which even dramatic cosmetic improvements may sometimes fail to meet patient expectations. Nevertheless, despite the inherent technical challenges and emotional risks, the lure of a more attractive face is a powerful motivating force that is likely to ensure the popularity of cosmetic nasal surgery indefinitely.
Unfortunately, the growing popularity of cosmetic nasal surgery has also created a corresponding increase in the number of substandard rhinoplasty outcomes. While a failed rhinoplasty may occasionally result entirely from adverse tissue responses to a well-executed surgical procedure, failed surgeries are far more often the result of technical errors such as faulty cosmetic analysis, poor artistic judgment, overzealous tissue removal, and/or gross surgical ineptitude. And while primary (first-time) rhinoplasty is widely regarded as among the most challenging of all elective cosmetic procedures, treatment of a failed rhinoplasty, commonly known as revision (or secondary) rhinoplasty, is typically an order of magnitude more difficult. Unlike primary rhinoplasty in which the misshapen nose is devoid of surgical scarring, every revision rhinoplasty patient presents with previously operated tissues that have sustained varying degrees of skeletal disruption, subcutaneous fibrosis, circulatory impairment, and/or soft tissue contracture. Moreover, while the primary rhinoplasty patient is typically upbeat and excited about the prospect of a more attractive nose, the revision rhinoplasty patient is frequently burdened by apprehension, anxiety, and skepticism. Hence both the technical and psychological challenges of revision rhinoplasty are often formidable.
Without question, complex revision rhinoplasty ranks among the most technically demanding of all cosmetic surgeries and is best reserved for the revision rhinoplasty specialist. Indeed, even for the most gifted cosmetic surgeon, a near-singular devotion to nasal surgery is often necessary to develop proficiency in this extremely challenging surgical niche. And while the technical demands of revision rhinoplasty are considerable, exceptional technical skills alone are not sufficient for a successful practice. The truly effective revision surgeon must also possess a discerning, yet compassionate listening ear and a willingness to confront the myriad emotional issues that typically accompany a failed rhinoplasty. Often the patient’s emotional trauma is considerable and may even lead to depression, social isolation, and impaired functioning. And since the emotional consequences of a failed rhinoplasty are often so profound, the importance of revision rhinoplasty cannot be overstated. Without question, complex revision rhinoplasty is an emotionally charged and technically demanding procedure that requires expertise, sensitivity, and exceptional technical skill.
Fortunately, contemporary techniques in revision rhinoplasty are now more effective than ever before. And while perfect restoration of the devastated nose is seldom possible, a carefully conceived and well-executed surgical treatment plan is often rewarded with considerable cosmetic and functional improvement. However, devising an effective surgical treatment plan is itself a complex and difficult undertaking. The surgeon must first correctly
assess the cosmetic deformity and the corresponding tissue characteristics, and then formulate a surgical game plan that will reliably achieve the desired cosmetic goal, all while limiting risk, cost, and treatment time. Once the game plan is formulated, the surgeon must also justify the treatment rationale and disclose potential surgical risks to an often apprehensive and nervous patient. Care must be taken not to trivialize the surgical risks and generate a false sense of security; yet at the same time, equal care must be taken to avoid overemphasizing the surgical risks and needlessly alarming the already worried patient. Fortunately, for the majority of patients a single operation in competent hands results in a satisfactory, albeit slightly imperfect restoration of nasal function and beauty. For those seeking maximum improvement, staged reconstruction often yields superior overall results when tissues permit, but few patients have the inclination, time, or financial resources to undertake sequential revision surgery.
assess the cosmetic deformity and the corresponding tissue characteristics, and then formulate a surgical game plan that will reliably achieve the desired cosmetic goal, all while limiting risk, cost, and treatment time. Once the game plan is formulated, the surgeon must also justify the treatment rationale and disclose potential surgical risks to an often apprehensive and nervous patient. Care must be taken not to trivialize the surgical risks and generate a false sense of security; yet at the same time, equal care must be taken to avoid overemphasizing the surgical risks and needlessly alarming the already worried patient. Fortunately, for the majority of patients a single operation in competent hands results in a satisfactory, albeit slightly imperfect restoration of nasal function and beauty. For those seeking maximum improvement, staged reconstruction often yields superior overall results when tissues permit, but few patients have the inclination, time, or financial resources to undertake sequential revision surgery.
For the surgeon, successful restoration of the devastated nose is more than a technical triumph; it is an immensely rewarding endeavor in which the emotional benefits to the patient can be truly life changing. Indeed, few other elective cosmetic procedures can impact a patient so profoundly, and the heartfelt appreciation of these individuals is extremely gratifying.
POSTSURGICAL DEFORMITIES OF THE NOSE
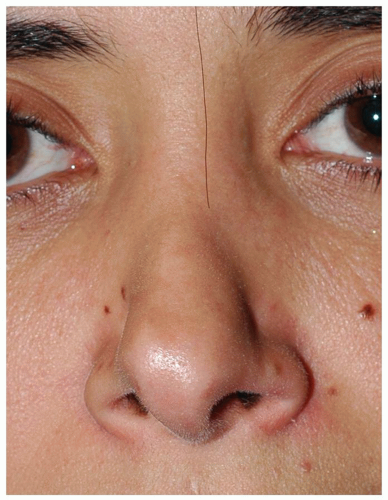
The severity of postsurgical nasal deformities varies widely, ranging from minor to irreversible. Patients presenting with gross overresection of the skeletal framework often constitute the greatest technical challenge, especially when coupled with fibrotic nasal skin, naturally weak nasal cartilage, and/or functional airway disturbances. And technical challenges are most severe when major anatomic deficiencies are coupled with genetically unfavorable wound-healing characteristics. Although some patients may present with only mild cosmetic or functional impairment, the complex revision rhinoplasty patient presents with moderate to severe cosmetic deformity, often complicated by concurrent nasal airway dysfunction. Sadly, a growing number of patients are presenting with profound cosmetic deformities following multiple misguided attempts at revision surgery. In many instances, tissue limitations, such as the cumulative effects of fibrosis, contracture, and vascular impairment, prevent successful surgical restoration of the nose, even in expert hands (Fig. 184.1). Although young healthy individuals can sometimes tolerate repeated nasal surgeries and still retain effective healing responses, revision rhinoplasty becomes progressively more difficult with each successive surgery, and all noses will eventually reach a point of surgical intolerance at some time. Determining whether or not a given nose can safely tolerate further surgery is a difficult and imprecise undertaking, and each patient must be approached cautiously in the context of potential surgical intolerance.
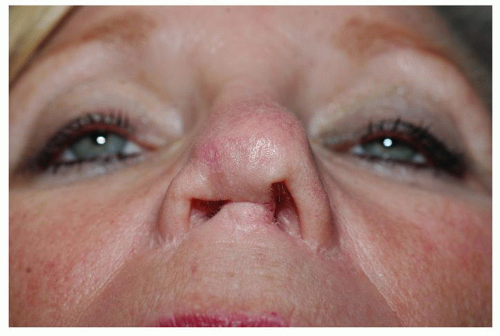 Figure 184.1 Severe nasal deformity presenting after multiple unsuccessful attempts at revision rhinoplasty. |
In deciding whether or not to pursue further surgery, a thorough physical examination of the nose is paramount. Direct physical examination is the only available means of assessing the anatomic, structural, and physiologic severity of a failed rhinoplasty, and without this critical assessment, the likelihood of a successful revision surgery is greatly diminished. Adverse physical findings such as a severely collapsed nasal framework, scarred and inelastic nasal skin, signs of borderline tissue perfusion, or dense cicatricial stenoses of the vestibular skin are the hallmarks of pending surgical intolerance, and these findings should prompt a sober reassessment of the need for further surgical treatment. In the worst-case scenario, numerous adverse physical findings combine to yield a strongly unfavorable risk-to-benefit ratio and a relative contraindication to further cosmetic surgery. On the other hand, debilitating functional impairment such as severe obstructive sleep apnea resulting from profound nasal airway obstruction may justify further intervention despite the increased surgical risk. Ironically, some seemingly intolerant noses will respond surprisingly well to a properly executed revision rhinoplasty, while some seemingly healthy noses will occasionally suffer significant wound-healing complications. Hence, the decision to reoperate is a dilemma for which there is no easy answer, and since no patient is ever fully immune from unforeseen complications, the prudent surgeon must balance the potential surgical risks against the emotional and physical burden of an untreated nasal deformity.
Although there are an infinite number of postsurgical nasal deformities that may arise following primary cosmetic rhinoplasty, cosmetic deformities can be loosely categorized as those of skeletal tissue excess and those of skeletal tissue deficiency. Postsurgical contour deformities of skeletal tissue excess are most often the result of incomplete or neglected treatment of congenital skeletal
overgrowth such as a persistent dorsal hump or a persistent hanging columella. In straightforward cases of skeletal tissue excess, the prognosis is often highly favorable since revision surgery simply entails completing the primary rhinoplasty—the so-called completion rhinoplasty (see Case One).
overgrowth such as a persistent dorsal hump or a persistent hanging columella. In straightforward cases of skeletal tissue excess, the prognosis is often highly favorable since revision surgery simply entails completing the primary rhinoplasty—the so-called completion rhinoplasty (see Case One).
Another common cause of skeletal tissue excess is the overzealous use of augmentation graft materials—the so-called overgrafted nose. Typically, surgical revision of the overgrafted nose is a difficult undertaking that requires reconfiguration of the nasal framework by removing, replacing, and/or modifying the existing structural elements to achieve an attractive, harmonious, and structurally sound skeletal framework. Treatment is particularly difficult when the existing nasal framework is twisted or asymmetric since extensive surgical “deconstruction”— and thus destabilization of the skeletal framework—is required. In contrast, revision of the overgrafted nose is comparatively straightforward when only superficial surface changes are required and extensive skeletal destabilization can be avoided.
Unlike postrhinoplasty deformities of skeletal tissue excess that are often the result of incomplete surgical treatment, postsurgical deformities of skeletal deficiency are commonly the result of aggressive overtreatment. In the so-called “overresected nose,” excessive lowering of the nasal bridge and/or overzealous excision of the nasal tip cartilage results in a profound and often progressive collapse of the nasal framework. The cosmetic impact of surgical overresection is an unattractive and stigmatic look that is derived from an amalgamation of various characteristic nasal deformities (Fig. 184.2A-C). Surgical overresection of the alar cartilages, particularly the lateral crura, frequently leads to pinching of the nasal tip, alar retraction, bossae, and/or supra-alar pinching, while overresection of the anterior septum may lead to overrotation or excessive deprojection of the tip unit (1, 2, 3). Moreover, overresection of the anterior septum will typically weaken skeletal tip support and exacerbate the adverse effects of alar cartilage overresection (1, 4). Finally, overresection of the nasal dorsum leads to a scooped dorsal profile, often accompanied by middle vault pinching, a widened and washed-out bony dorsum, and abnormal shadowing of the bony-cartilaginous junction—the so-called inverted-V deformity (3, 5) (Fig. 184.3). In addition to a conspicuous and unsightly nasal appearance, the overresected nose is also emblematic of bad rhinoplasty surgery—a highly undesirable stigma that adds to the patient’s emotional distress. Unfortunately the morbidity of surgical overresection is not limited to cosmetic sequelae as most overresected noses are also burdened by collapse of the internal and/or external nasal valves leading to symptomatic nasal airway obstruction (1, 2, 3). Overresection of the nasal framework is a devastating complication of cosmetic rhinoplasty that usually leads to severe nasal deformity and that likely represents the most common motivation for revision rhinoplasty.
In order to restore the overresected nose to create a sturdy, attractive, and fully functional appendage, revision rhinoplasty requires re-expansion of the undersized and collapsed skeletal framework—frequently against a scarred and inelastic soft tissue envelope. Unlike naturally elastic nasal skin that can stretch to accommodate full skeletal re-expansion, fibrotic and noncompliant skin may fail to permit cosmetically and functionally ideal enlargement of the nasal framework. Moreover, successful skeletal re-expansion requires a newly constructed framework of sufficient rigidity to distend the scarred and noncompliant nasal skin without invoking skeletal distortion, all while simultaneously avoiding cutaneous vascular insufficiency produced by excessive closing tension and subsequent disruption of nutrient blood flow. In patients with medical comorbidities such as cigarette smoking, diabetes, inflammatory disease, prior cocaine abuse, or any other form of preexisting vascular impairment, the risk of vascular insufficiency is greatly increased, and excessive skin tension must be carefully avoided even if the newly expanded framework must be reduced in size. Accordingly, a thorough history and physical examination is particularly important in this patient population to screen for risk factors or preexisting manifestations of impaired tissue perfusion. Although frank skin necrosis is exceedingly rare in revision rhinoplasty, vascular insufficiency may still result in wound dehiscence, incomplete revascularization of autografts, and/or frank wound infection—any of which may potentially jeopardize the surgical outcome and produce disastrous surgical consequences. Consequently, in the overly short and underprojected nose with stubbornly noncompliant nasal skin, avoidance of vascular compromise often precludes full skeletal re-expansion and this limitation is best identified and discussed prior to surgery. Moreover, even in the absence of skeletal re-expansion, tissue perfusion is disrupted to some degree in every rhinoplasty, and proactive measures to optimize tissue perfusion are essential. Meticulous soft tissue technique, judicious use of electrocautery, appropriate use of surgical dissection planes, avoidance of overly constrictive compression dressings, careful monitoring of capillary refill, and postoperative supportive measures all serve to collectively optimize soft tissue perfusion and reduce the risk of ischemic injury. Without question, the combined skeletal and soft tissues derangements associated with the overresected nose make it one of the most technically challenging and complication-prone of all postsurgical nasal deformities.
In reality, most severe surgical deformities are a combination of overresected skeletal tissues and untreated deformities of the original nose. Coexisting nasal airway dysfunction is common, and twisting and/or asymmetry of the damaged framework is also frequently present, both of which make revision rhinoplasty considerably more complicated. And while a severely disfigured nose presents
a formidable and sometimes insurmountable technical challenge, the presence of coexisting psychosocial issues can also greatly complicate the management of any rhinoplasty patient.
a formidable and sometimes insurmountable technical challenge, the presence of coexisting psychosocial issues can also greatly complicate the management of any rhinoplasty patient.
PATIENT EVALUATION AND TREATMENT PLANNING
Regardless of whether the surgical challenge is big or small, the ultimate objective of revision rhinoplasty is always the same—to create an attractive, sturdy, and fully functional nose that flatters the face and integrates naturally with the surrounding facial features. However, this task is not always easy or even medically feasible, and deciding when and how to operate is the first critical step in a successful revision rhinoplasty. Ironically, it is often the failure to properly evaluate the nose that leads to revision rhinoplasty in the first place, and the importance of the preoperative nasal history, physical examination, and cosmetic analysis cannot be overemphasized. Although the novice surgeon often focuses primarily upon the operative procedure, the accomplished surgeon will spend as much or more time on the evaluation, analysis, and treatment planning as on the operation itself. And because the end result of revision rhinoplasty depends as much upon tissue quality and healing responses as the actual operation, recognizing and planning for tissue inadequacies is frequently what differentiates a favorable outcome from a disappointing one.
For the revision rhinoplasty patient, the initial nasal assessment begins with a thorough rhinoplasty history detailing the number of prior surgeries, the recovery interval between surgeries, the specific intervention for each surgery, and the subsequent tissue responses. This information serves to characterize the type and degree of prior tissue alteration and the overall wound-healing tendencies. When combined with the results of a thorough nasal examination, the rhinoplasty history will reveal the approximate anatomic and physiologic health of the nose and its likely tolerance for additional surgery. From this baseline perspective, the surgeon must then analyze the cosmetic deformity, pinpoint the desired cosmetic and functional end point, and devise an effective surgical game plan that accounts for the existing anatomic and cosmetic inadequacies. A careful assessment of the existing structural support, airway patency, nasal contour, and tissue quality will enable the surgeon to customize the surgical game plan in order to compensate for anticipated tissue deficiencies and/or adverse wound-healing responses. From the psychological standpoint, perhaps the biggest challenge in revision rhinoplasty is establishing realistic cosmetic expectations that coincide with the anticipated surgical complexity and the associated risks and limitations therein. A careful assessment of the patient’s personality, underlying motives, and cosmetic objectives is also essential to reduce the likelihood of disappointment and/or confrontation stemming from unmet surgical expectations. Clearly, complex revision rhinoplasty is an intricate and complicated puzzle that can only be solved with a detailed and thorough preoperative evaluation.
PSYCHOLOGICAL ASPECTS OF REVISION RHINOPLASTY
From the moment of introduction, an evaluation of the patient’s emotional health and well-being should commence. To begin the consultation, the surgeon should review the patient’s social history, including the patient’s education, employment, marital status, living situation, and psychiatric history. This information will help to delineate the patient’s level of functioning and to define his or her emotional support network. As the consultation proceeds, the surgeon should also carefully explore the patient’s justification for seeking revision rhinoplasty and the patient’s concept of a satisfactory outcome. In most instances, healthy patient motives and realistic treatment expectations become increasingly evident as doctor/patient relationship develops. However, for patients with discrete emotional pathology, inappropriate motives and/or grandiose surgical expectations are often the first signs of underlying emotional illness. Unfortunately, many serious emotional disorders are not always readily
apparent, and emotionally disturbed patients are often adept at concealing their symptoms. Although the majority of secondary rhinoplasty patients are not suffering from discrete emotional illness, emotional overtones are common in both emotionally unbalanced and emotionally healthy revision patients, making it difficult to properly differentiate between these fundamentally different yet outwardly similar patient groups. And because discrete emotional disorders are often more difficult to identify in the revision rhinoplasty patient, the consulting surgeon should maintain a high index of suspicion in any patient who exhibits subtle signs or symptoms suggestive of emotional pathology. Although detecting emotional illness is sometimes challenging, the importance of early identification is paramount since surgical treatment is often contraindicated in patients with discrete psychological disorders; and failure to properly screen for emotional pathology may lead to potentially catastrophic treatment complications.
apparent, and emotionally disturbed patients are often adept at concealing their symptoms. Although the majority of secondary rhinoplasty patients are not suffering from discrete emotional illness, emotional overtones are common in both emotionally unbalanced and emotionally healthy revision patients, making it difficult to properly differentiate between these fundamentally different yet outwardly similar patient groups. And because discrete emotional disorders are often more difficult to identify in the revision rhinoplasty patient, the consulting surgeon should maintain a high index of suspicion in any patient who exhibits subtle signs or symptoms suggestive of emotional pathology. Although detecting emotional illness is sometimes challenging, the importance of early identification is paramount since surgical treatment is often contraindicated in patients with discrete psychological disorders; and failure to properly screen for emotional pathology may lead to potentially catastrophic treatment complications.
As stated above, psychological evaluation of the revision rhinoplasty patient is made more challenging by the normal, yet sometimes alarming emotional overtones that typically accompany a failed rhinoplasty. While these emotional overtones manifest differently among revision rhinoplasty patients according to a variety of factors, the typical primary rhinoplasty patient is generally far less complicated from an emotional standpoint. For surgeons unfamiliar with the emotional by-products of a failed rhinoplasty, behavior of the typical (well-adjusted) revision rhinoplasty patient may occasionally seem both inappropriate and disconcerting, particularly when compared to the happy-go-lucky primary rhinoplasty patient. Consequently, understanding and appreciating the unique emotional context of the revision rhinoplasty patient is fundamental to appropriate patient selection and successful patient management.
For the typical first-time (primary) rhinoplasty patient, the prospect of an attractive and unobtrusive nose is a longsought personal goal that is the motivating force behind surgical treatment. Characteristically, the first-time rhinoplasty patient is upbeat and excited about surgery, since it promises to beautify a nose that was often a source of insecurity, embarrassment, or social ridicule. Any fears or apprehensions generated by the anticipated discomfort or potential risks of surgery are often quickly dispelled by the prospect of an attractive new facial appearance. In fact, the typical primary rhinoplasty patient often approaches the surgery with carefree optimism, focused primarily upon the promise of a favorable cosmetic outcome.
In contrast, for the typical revision rhinoplasty patient, the bitter disappointment of a failed rhinoplasty gives rise to a far more pessimistic outlook dominated by apprehension, worry, and skepticism. For most revision patients, the emotional nightmare that prompted secondary rhinoplasty is not easily forgotten, and further treatment is seen through a much more ominous perspective. Frequently the prospective revision rhinoplasty patient is skeptical, indecisive, and hesitant to risk further facial deformity despite a favorable prognosis for a successful restoration. As a consequence, many patients awaiting revision surgery repeatedly second-guess their treatment decision and become increasingly more anxious as surgery approaches.
The apprehension and lack of confidence typical of the revision rhinoplasty patient is easy to understand. Rather than the attractive and natural-appearing nose that was anticipated, the revision rhinoplasty patient has been forced to contend with unexpected facial disfigurement and the array of unpleasant human emotions that naturally accompany an adverse life event. The realization that their surgeon may have been inexperienced and poorly trained, or even incompetent and deceitful, is often very difficult to accept, particularly if surgery was preceded by repeated assurances that a favorable outcome was a virtual certainty. Accordingly, confusion, bewilderment, embarrassment, resentment, anger, and mistrust often characterize the initial response to a failed cosmetic rhinoplasty. And for the emotionally frail and insecure individual who lacks strong coping skills, the psychological impact of a failed rhinoplasty is typically far more severe and disabling. Moreover, for patients with frank psychological disorders, a failed rhinoplasty may provoke considerable anger and resentment resulting in a wide range of maladaptive and aberrant behaviors. Hence the prospect of further surgery in the previously operated patient is a much different undertaking that must be approached in a far different manner.
Fortunately, most revision rhinoplasty patients are well-adjusted individuals who are reacting in a justifiable manner to an unanticipated facial deformity. And although even well-adjusted individuals must reconcile the negative human emotions that inevitably attend a failed rhinoplasty, once beyond the initial shock and disappointment of an adverse outcome, the well-balanced individual quickly rebounds and seeks appropriate restorative treatment. Eventually, anger and disappointment are channeled in a healthy and productive manner—ultimately leading to a rational plan of action and resolution of the problem.
In contrast, for those with poor coping skills, a failed rhinoplasty can become an emotionally devastating event heralded by withdrawal, self-pity, and depression. Extreme insecurity and social isolation are not uncommon in this patient population, and in severe cases may even lead to loss of employment, disruption of schooling, and/or failed interpersonal relationships. Despite their yearning for an attractive nose, the emotionally insecure patient often becomes paralyzed with apprehension and may wait years before finally deciding to undertake revision surgery. For others, the longing for a normal-looking nose is superseded by the fear of yet another failed outcome, and despite a favorable surgical prognosis, surgery is never undertaken.
Finally, a small number of revision rhinoplasty patients also suffer from underlying psychological illness. In addition to the already substantial technical challenges typical
of complex revision rhinoplasty, management is further complicated by active resistance to patient counseling, a lack of rational decision making, and disregard for surgical restrictions and care requirements. In some instances, psychological disturbances may even render the patient incapable of assessing their postrhinoplasty outcome with any degree of objectivity. Regardless of whether or not these patients have legitimate cosmetic abnormalities, their inability to acknowledge previously damaged nasal tissues, subsequent treatment limitations, inherent surgical risks, and/or actual surgical improvements makes them exceedingly poor surgical candidates irrespective of their surgical prognosis. Failure to identify such individuals and to defer surgical treatment can lead to anger, confrontation, hostility, and potentially even violence against the surgeon or the surgical staff; and such problems underscore the importance of careful patient screening during the initial evaluation.
of complex revision rhinoplasty, management is further complicated by active resistance to patient counseling, a lack of rational decision making, and disregard for surgical restrictions and care requirements. In some instances, psychological disturbances may even render the patient incapable of assessing their postrhinoplasty outcome with any degree of objectivity. Regardless of whether or not these patients have legitimate cosmetic abnormalities, their inability to acknowledge previously damaged nasal tissues, subsequent treatment limitations, inherent surgical risks, and/or actual surgical improvements makes them exceedingly poor surgical candidates irrespective of their surgical prognosis. Failure to identify such individuals and to defer surgical treatment can lead to anger, confrontation, hostility, and potentially even violence against the surgeon or the surgical staff; and such problems underscore the importance of careful patient screening during the initial evaluation.
Although most revision rhinoplasty patients are welladjusted individuals, for even the most self-assured and emotionally secure individual, the initial impact of a failed surgery is substantial and can be exacerbated by absent family support, severe disfigurement, insufficient financial resources, or limited access to appropriate medical care. Instead of enjoying the physical and emotional benefits of an attractive new nose, the failed rhinoplasty patient must contend with the prolonged public stigma of a “botched nose job,” and the prospect of a second more difficult, and frequently more expensive, revision surgery. Even individuals with robust coping mechanisms and a strong emotional support network will suffer some measure of angst in this scenario, and the revision rhinoplasty surgeon must make allowances for these difficult circumstances (6). At the very least, the revision rhinoplasty surgeon should regard all prospective revision patients, including those with healthy coping skills, as emotionally traumatized, potentially labile, and justifiably distraught individuals. Without question, the addition of powerful and unpredictable emotions superimposed upon a formidable technical challenge make revision rhinoplasty patients exceptionally difficult to treat (6, 7).
Perhaps one of the most difficult aspects of revision rhinoplasty is establishing a bond of trust with the apprehensive and cautious secondary rhinoplasty patient. Having previously placed their trust in a medical professional they assumed would beautify their nose, the typical revision rhinoplasty patient often finds it difficult to trust another surgeon, much less to then embark upon a more difficult and more hazardous secondary operation. Since many adverse rhinoplasty outcomes result from substandard surgical care, a cautious and skeptical approach to further surgery is clearly justified but may itself become an obstacle to the ultimate goal of nasal restoration. Furthermore, most revision rhinoplasty patients resort to the Internet for treatment advice where confusing and often erroneous recommendations are commonplace. The Internet also provides interactions with hundreds of other unhappy rhinoplasty patients serving to underscore the prevalence of adverse outcomes and to further raise the level of patient anxiety. Sadly, the Internet often portrays rhinoplasty surgeons as uncaring and profit-driven individuals who prey upon the unsuspecting. And while the unethical and incompetent practices of some cosmetic surgeons may lend credence to these cynical viewpoints, the emotionally traumatized and gullible revision rhinoplasty patient is particularly susceptible to such distortions and may erroneously regard these views as both authoritative and trustworthy. Consequently, the prospective revision rhinoplasty patient often initially regards the treatment recommendations of the revision rhinoplasty consultant with suspicion and mistrust. Even multiple consultations with seasoned revision rhinoplasty experts may fail to provide clarity and reassurance, particularly since legitimate differences in treatment philosophy often result in contradictory treatment recommendations. Hence, while the secondary rhinoplasty patient is often eager to treat the postsurgical deformity, they are often confused and uncertain about where to turn for help.
Upon the realization that further nasal surgery is inevitable, most revision rhinoplasty patients seek to become more knowledgeable as to the methods, risks, and options for revision nasal surgery. As a result, patients occasionally demonstrate a surprising familiarity with technical rhinoplasty jargon and tout a (cursory) understanding of secondary rhinoplasty techniques. Moreover, they will often challenge the technical aspects of a proposed treatment plan based upon a naive and sometimes distorted understanding of nasal surgery. At face value, these patients may seem overly controlling and manipulative—much like the individual with narcissistic personality disorder. However, upon closer scrutiny these individuals are usually nothing more than fearful victims who are desperately trying to avoid yet another devastating surgical outcome, and the revision rhinoplasty surgeon should not necessarily be intimidated by patients seeking validation of the proposed treatment plan.
Without question, a failed rhinoplasty has numerous medical, financial, and psychosocial implications for the patient. Moreover, the task of finding a trustworthy surgeon with appropriate skills and expertise can prove a daunting and frustrating task for the gun-shy patient, particularly when conflicting opinions and misinformation abound. Since many prospective patients harbor concerns about the integrity, professionalism, and surgical competence of the revision surgeon, a compassionate listening ear and a willingness to patiently justify all treatment recommendations is the first step in earning patient trust and confidence. Failure to effectively justify the proposed treatment plan or to provide a compelling rebuttal to various misguided treatment recommendations, no matter how painstaking or time-consuming, may ultimately foster mistrust and create an emotional barrier to successful revision surgery.
And although a trusting relationship takes considerable time and effort to cultivate, it is highly improbable that a revision rhinoplasty patient will progress to surgical treatment without it.
And although a trusting relationship takes considerable time and effort to cultivate, it is highly improbable that a revision rhinoplasty patient will progress to surgical treatment without it.
SOMATOFORM AND PERSONALITY DISORDERS
Despite the commonly held view that cosmetic nasal surgery is merely a superficial (nontherapeutic) alteration of outward appearance, significant psychological benefits have been confirmed in well-adjusted individuals following successful primary rhinoplasty (8, 9). Moreover, it is reasonable to conclude that similar therapeutic benefits are likely for the revision rhinoplasty patient since a successful outcome can fully eliminate the cause of emotional angst and provide analogous psychological benefits. However, roughly one-third of individuals seeking cosmetic nasal surgery also present with symptoms of mild to moderate psychiatric disease (8, 9). Included among this subset of patients are those with distinct and identifiable psychological disorders such as somatoform disorders or various forms of aberrant personality disorders. In both cases, these disorders may thwart successful treatment, and the treating surgeon must be familiar with the hallmark symptoms of each disease so that appropriate precautions and/or exclusions can be implemented.
Body dysmorphic disorder (BDD) is a somatoform disorder that occurs at a far greater frequency among patients who seek cosmetic surgery (9, 10, 11). Sometimes called “imagined ugliness syndrome,” BDD is a DSM-IV disorder (Diagnostic and Statistical Manual of Mental Disorder, Fourth Edition) that is defined as an irrational preoccupation with an imagined or trivial defect in appearance that results in significant emotional distress and/or impairment in daily functioning. Nearly all BDD sufferers engage in compulsive behaviors such as mirror checking or skin picking related to obsessive preoccupations with personal appearance, often spending hours each day engaged in these anxiety-producing activities (9, 10, 11). In severe forms, BDD may give rise to surgically addictive behaviors in a futile quest to eliminate imaginary flaws in body image. However, nonpsychiatric medical treatments such as cosmetic surgery seldom prove effective in eliminating symptoms of BDD (9, 12). The most common form of BDD is the delusional variant in which patients lack insight or awareness regarding their obsession; whereas patients with the nondelusional variant can recognize their obsession to a variable extent (11). In the delusional form, sufferers are completely convinced that they appear ugly and grossly abnormal. Frequently BDD occurs in tandem with other psychiatric disorders including major depression, obsessive-compulsive disorder, substance abuse disorder, eating disorders, and personality disorders (9). Impaired psychosocial functioning is common in BDD and in severe cases may result in prolonged school or work absences, or the inability to sustain interpersonal relationships (11). Clinical depression is a near-universal feature of BDD, and patients with severe BDD are at significantly increased risk for suicide (10, 11). Revision rhinoplasty surgeons are also likely to encounter BDD patients with far greater frequency as the nose is one of the most common areas of concern second only to the hair and skin (10). Interestingly, BDD sufferers also frequently “doctor shop” as they relentlessly seek a surgical cure to their psychiatric illness (9, 10). However, in contrast to well-balanced patients with mild but correctable complaints who will benefit from successful revision surgery, those with BDD may never achieve satisfaction regardless of the cosmetic outcome. Even exceptional cosmetic outcomes are unlikely to eliminate the patient’s dissatisfaction with their nasal contour and may even trigger new obsessions with other body parts (9, 10). Physical violence is also more common in distraught BDD patients and may be directed at cosmetic surgeons who fail to eliminate the perceived deformity (9, 10, 11, 12). Because many BDD sufferers are adept at evading the screening process, the diagnosis of BDD should be entertained in any patient who dwells excessively upon a minimal or barely perceptible cosmetic defect. In a recent survey of 265 aesthetics surgeons regarding BDD, 84% failed to recognize symptoms of BDD until after surgery (12). Because surgical success rates are exceedingly poor in patients suffering from BDD, particularly delusional BDD patients in whom appropriate insight is lacking, surgery is generally contraindicated (9, 11). Psychiatric evaluation and treatment is recommended for any individual in whom BDD is suspected, particularly since the delusional variant appears to respond to drug therapy with serotonin reuptake inhibitors (10, 11). Psychiatric clearance is also essential for any suspected BDD patient prior to cosmetic surgical treatment (10), but surgical success rates in patients with documented BDD are notoriously poor and there is a growing consensus that BDD should be regarded as a contraindication to cosmetic treatments (9, 11).
Personality disorders, defined as deeply ingrained, nonpsychotic, and maladaptive patterns of behaving and relating to others, are the most commonly encountered psychological disturbance in patients seeking cosmetic surgery (6, 13). Although certain personality disorders are easily recognized, others such as borderline personality disorder may be difficult to identify since patients may initially seem normal. The borderline personality disorder is characterized by a sense of loneliness and emptiness, unpredictable mood swings, fear of abandonment, and irritability (6). Patients with borderline personality disorder may be identified as slightly “off” due to excessive flattery and premature familiarity, juxtaposed against aggressive and suspicious questioning. Despite behavior that is initially flattering, sympathetic, or seductive, stressful events such as a failed rhinoplasty (or a perceived surgical failure) may trigger acute decompensation with overt maladaptive symptoms such as postoperative depression,
disordered self-image, and/or inappropriate demonstrations of anger, as individuals with borderline personality disorder look to others for cause, responsibility, and blame for their actions or circumstances (6, 13).
disordered self-image, and/or inappropriate demonstrations of anger, as individuals with borderline personality disorder look to others for cause, responsibility, and blame for their actions or circumstances (6, 13).
Another commonly encountered personality disorder, the narcissistic personality disorder, is characterized by excessive arrogance and a feeling of superiority to others, regardless of actual achievements (6). Patients with narcissistic personality feel entitled to special treatment from office staff and the surgeon due to an inflated sense of self-esteem. Narcissists require continual validation of their special status and react with indifference, contempt, or even hostility to those who fail to actively reinforce their self-perceived greatness. Often they wear conspicuous flashy clothing or makeup and behave in a way that is designed to attract attention. Consequently, the narcissistic personality is typically very easy to discern in consultation. They interrupt frequently, demonstrate resistance to active listening, and show disinterest in surgical recommendations as they typically possess a preconceived notion of what procedure is best for them. While the otherwise normal but self-centered or egotistical individual may make a suitable surgical candidate when they are able to acknowledge the limitations of surgical treatment, elective cosmetic surgery is generally contraindicated in the patient with frank narcissistic personality disorder (6). Moreover, failure to meet the unrealistic cosmetic expectations of the narcissistic patient may trigger a narcissistic rage that can be disturbing, frightening, and even physically violent.
When evaluating any prospective rhinoplasty patient, it is critically important for the revision rhinoplasty surgeon to look beyond the technical aspects of surgical treatment and to closely examine the psychological health of the individual as demonstrated through the developing surgeon-patient relationship. Virtually all revision rhinoplasty patients present with some measure of recent or current emotional upheaval in response to the adverse rhinoplasty outcome, making detection of emotional pathology far more difficult. However, for the emotionally healthy individual, the normal response to a stressful adverse life event does not ultimately inhibit effective management. In contrast, for patients with various emotional disorders, the absence of insight and/or objective thinking makes attaining a satisfied patient highly improbable, and treatment is usually best avoided altogether. Failure to recognize the differentiating signs and symptoms of these emotionally troubled patients may result in significant conflict between patient and surgeon even when the surgical care is appropriate and the surgical outcome is satisfactory. In extreme cases, maladaptive behaviors may lead to confrontation, hostility, and potentially even physical violence. And with the recent popularity of Internet communication, hostility may also manifest through online slander, character assassination, and/or fictitious accounts of surgical negligence, all protected by the cloak of Internet anonymity. Clearly, a failed rhinoplasty is an emotionally charged issue, and the revision surgeon must always be mindful of the significant emotional overlay associated with treatment expectations, particularly in the presence of underlying emotional pathology.
KEY PROGNOSTIC INDICATORS IN SECONDARY RHINOPLASTY
Proper physical evaluation of the revision rhinoplasty patient includes an assessment of several key determinants that strongly impact the surgical prognosis. The importance of these determinants to successful secondary rhinoplasty merits special emphasis during the nasal examination and each of these variables is briefly highlighted below.
In addition to evaluating the psychological well-being of the patient, the initial patient evaluation should focus upon the patient’s general medical health, particularly as it relates to anesthetic tolerance and surgical wound healing. Although robust general health, good exercise tolerance, and the absence of medical comorbidities are favorable indicators of physical vigor at any age, secondary nasal surgery becomes increasingly more difficult in later life. In contrast to adolescents and young adults who typically possess a dramatic and rapidly forgiving recuperative capacity, elective cosmetic nasal surgery is often far more prone to complications in middle age and beyond. While general physical vitality remains an important consideration in all patients, age alone is a major consideration in cosmetic nasal surgery, particularly in the previously operated nose. Hence, complex revision rhinoplasty should be approached with caution in the older patient since nasal healing responses often decline with age.
Another important prognostic indicator is the length of time since prior nasal surgery. Although surgically induced tissue trauma is to a large extent permanent and therefore cumulative, at least some degree of tissue injury is reversible if given adequate time for recovery. Consequently, multiple surgical procedures stacked at close intervals are highly detrimental since the nose has yet to recover from one injury before being subjected to another. In this scenario, even a young healthy patient with highly favorable recuperative powers may develop adverse wound-healing responses due to repeated uncompensated tissue trauma. Conversely, a healthy 35-year-old patient seeking revision of a failed teenage rhinoplasty has the advantage of a nearly two decade-long recovery in which all reversible injury has fully resolved. In this scenario, a well-executed revision rhinoplasty in a suitable candidate is usually followed by favorable wound-healing responses, sometimes comparable to a previously unoperated nose. Hence, noses that have been allowed a prolonged period of recovery are often far more tolerant of secondary surgery, whereas revision surgery in the face of acute swelling and inflammation may lead to increased complication rates from adverse healing responses.
Another critical factor that can dramatically impact the surgical prognosis is nasal skin quality. Without question, a smooth and healthy nasal complexion with intermediate skin thickness is best suited to cosmetic nasal surgery. In fact, a clear, smooth (nonsebaceous) complexion almost always indicates tolerant and “forgiving” nasal skin with minimal scarring tendencies and little preexisting cutaneous inflammation. On the other hand, thick oily nasal skin with large sebaceous units often responds poorly to surgical manipulation, reacting with excessive swelling, prolonged inflammation, and a tendency for heavy subcutaneous scarring. In the oversized nose, thick inelastic skin may fail to contract and properly conform to surgical reduction of the skeletal framework, whereas in the undersized nose, thick inelastic skin may limit cosmetically ideal skeletal re-expansion. Another important disadvantage of ultrathick nasal skin is the loss of surface definition created by excessive masking of the underlying skeletal framework. Because ultrathick nasal skin heavily obscures topographic features of the underlying nasal skeleton, the delicate surface undulations that characterize a well-defined and attractive nasal tip are lost. Moreover, a weak and underprojected nasal framework, whether acquired naturally or through surgical overresection, only serves to exacerbate the loss of desirable surface highlights. In contrast, for patients with extremely thin nasal skin, the atretic outer covering offers scant camouflage of underlying skeletal imperfections, and a flawless skeletal contour is required to prevent visible imperfections in the surface topography. Furthermore, both telangiectasias and dyschromias are easily provoked with repeated surgical dissection of thin nasal skin. In contrast to ultrathick or ultrathin nasal skin, intermediate skin thickness offers effective concealment of minor skeletal imperfections while still retaining a welldefined and attractive surface contour. In addition, healthy skin of intermediate thickness is usually associated with ample elasticity, prompt resolution of surgical edema with minimal subcutaneous scarring, and the capacity to rapidly conform to a surgically downsized nasal framework. When examining the previously operated nose, nasal skin quality is a crucial prognostic indicator that must be evaluated carefully. In fact, nasal skin quality is typically a far more reliable indicator of wound healing than is skin pigmentation, as virtually all skin tones will heal favorably when the complexion is smooth and clear. Consequently, failure to assess skin quality and to account for the intrinsic healing characteristics during surgical planning is a serious oversight in the evaluation process.
Another critical determinant of surgical success is intrinsic cartilage strength. Because the goal of any rhinoplasty is to create a permanent improvement in nasal contour via a nondeforming and durable skeletal framework, the biomechanical properties of the nasal cartilage are of critical importance to the long-term surgical outcome. Although cartilage strength is commonly regarded as unchanging throughout life, in reality cartilage stiffness commonly degrades over time. Age-related or disease-mediated losses in cartilage strength are inevitable in virtually every nose, and while noses blessed with naturally rigid cartilage may experience only negligible losses in structural support, in noses with naturally soft cartilage, age or disease-mediated deterioration may profoundly affect the shape and/or function of the nose over time. Moreover, even modest cartilage resection can exacerbate the age-related or diseasemediated deterioration of naturally weak nasal cartilage, producing a catastrophic effect upon long-term structural integrity. Vigorous soft tissue contraction—the so-called “shrink wrap” phenomenon—may compound the adverse impact of surgical intervention and age-related deterioration by distorting and collapsing the severely weakened nasal framework. Consequently, when evaluating the previously operated nose, baseline skeletal strength becomes a key indicator of both the existing structural support and the future susceptibility to structural failure. And since surgical restoration of the nose is only as good as the tissues used in the reconstruction, assessment of the baseline structural integrity and the strength of available graft materials are critical to the surgical prognosis and represent a crucial component of every new patient evaluation.
The final prognostic indicator is perhaps the most important single factor in the surgical prognosis—the body’s genetically predetermined response to tissue injury. While the majority of young healthy individuals enjoy a forgiving tissue response that facilitates rapid and favorable healing, a small subset of humans appear to have tissues that respond poorly to surgical manipulation regardless of the care and precision exercised during surgical treatment. Furthermore, this sinister tendency is nearly impossible to detect with certainty in any given patient. Unlike the aforementioned prognostic indicators that can be quantified during the new patient evaluation, unfavorable wound healing responses may occasionally present without any identifying signs or symptoms. And while the majority of unsuccessful rhinoplasties are probably the result of incorrect aesthetic analysis, poor artistic judgment, technical errors, or surgical incompetence, a small subset of adverse outcomes is unquestionably the result of genetically predetermined adverse would-healing tendencies. At their worst, unfavorable healing responses may lead to prolonged inflammation, excessive fibrosis of the soft tissue envelope, excessive or inadequate soft tissue contracture, vascular insufficiency, and/or diminished immune function. The cumulative effects of these antagonistic influences may completely negate all of the surgical modifications intended to enhance nasal contour and function. Moreover, adverse wound-healing responses often become more severe with each successive nasal surgery. Although physical signs such as thick inelastic nasal skin, hypertrophic scarring, or excessive subcutaneous fibrosis often foreshadow adverse wound-healing responses, hostile healing responses can also arise in seemingly favorable surgical candidates who are devoid of discrete clinical findings.
When combined with weak skeletal anatomy in the surgically damaged nose, adverse healing responses represent an insurmountable surgical challenge in which further surgery is best avoided. Because these patients are occasionally indistinguishable from those with normal healing responses, even the accomplished surgeon will occasionally experience an adverse surgical outcome despite performing a technically appropriate and well-executed surgical procedure. Consequently the prudent surgeon should forewarn all patients about the unlikely but potentially catastrophic development of adverse healing responses, and a favorable surgical outcome should never be guaranteed even in the seemingly ideal patient. Although physical signs and symptoms are often lacking, warning signs suggestive of adverse healing responses should be sought in every new patient evaluation.
When combined with weak skeletal anatomy in the surgically damaged nose, adverse healing responses represent an insurmountable surgical challenge in which further surgery is best avoided. Because these patients are occasionally indistinguishable from those with normal healing responses, even the accomplished surgeon will occasionally experience an adverse surgical outcome despite performing a technically appropriate and well-executed surgical procedure. Consequently the prudent surgeon should forewarn all patients about the unlikely but potentially catastrophic development of adverse healing responses, and a favorable surgical outcome should never be guaranteed even in the seemingly ideal patient. Although physical signs and symptoms are often lacking, warning signs suggestive of adverse healing responses should be sought in every new patient evaluation.
PHYSICAL ASSESSMENT OF THE NOSE
Perhaps the most commonly neglected, yet critically important component of the revision rhinoplasty assessment is physical examination of the nose. Because every secondary rhinoplasty patient presents with varying degrees of prior surgical scarring, skeletal disruption, vascular impairment, and/or structural instability; a proper revision rhinoplasty evaluation requires a thorough physical examination and cannot be conducted by photo review alone. Although photographic analysis of the nose is a critical component of the preoperative cosmetic assessment (5), high-resolution rhinoplasty photos fail to convey vital physical and biomechanical tissue properties like cartilage strength, tip support, sidewall rigidity, skin thickness, airway dimension, septal alignment, valve patency, or skin elasticity. In the aggregate, these tissues characteristics have a profound influence upon the method of surgical treatment and upon the probability of a successful surgical outcome. Failure to carefully examine the previously operated nose with a combination of inspection, palpation, and dynamic observation is a grave oversight that often precedes unsuccessful surgery. Hence, the present trend toward Internet consultations, while a reasonable first step in the evaluation process, should not be regarded as a suitable substitute for a proper one-on-one patient evaluation.
Surgical assessment of the nose prior to revision rhinoplasty requires a methodical physical examination designed to assess every physical characteristic that may influence the surgical outcome. The preoperative examination should be conducted in light of the patient’s cosmetic and functional objectives so that a realistic treatment plan can be devised that reflects the patient’s cosmetic goals and yet simultaneously recognizes and accounts for the anatomic obstacles to success. Although a proper surgical assessment cannot be performed from photographs alone, examination findings should be carefully correlated with standardized rhinoplasty photographs in order to obtain a complete and accurate cosmetic analysis. Indeed, a conventional aesthetic nasal analysis using standardized rhinoplasty photographs is an essential component of every good rhinoplasty evaluation (5). In addition to the cosmetic assessment, the preoperative nasal examination should also evaluate the structural integrity of the bony and cartilaginous skeletal framework; the thickness, elasticity, and perfusion of the inner and outer nasal lining; and the status of the entire nasal airway including the external and internal nasal valves, the nasal septum, and the nasal turbinates. In turn, this information will help to determine the associated surgical complexity, the surgical risk, and the surgical prognosis specific to each individual patient. Although this represents a time-consuming endeavor, without a comprehensive preoperative surgical evaluation the probability of a satisfactory final outcome is greatly diminished. Hence, the importance of the physical examination cannot be overemphasized.
Perhaps the most neglected aspect of the revision rhinoplasty evaluation is the functional assessment of the nose. Often the revision rhinoplasty patient is focused solely upon the cosmetic deformity and is reluctant to further complicate their management with complaints of functional impairment. However, nasal airway dysfunction is common in the revision rhinoplasty patient population and since untreated nasal airway dysfunction can lead to adverse health consequences, particular attention should be directed toward evaluating nasal airway patency. Typically, patients with nasal airway obstruction report daytime nasal congestion that becomes noticeably more severe at night. Subsequent nocturnal obstruction leads to associated symptoms of mouth breathing often accompanied by an overly dry throat, frequent awakenings from thirst or nasal obstruction, and disrupted sleep patterns with daytime fatigue. Ancillary symptoms such as rhinogenic headaches, decreased sense of smell, recurrent sinus infections, or Eustachian tube dysfunction may also be present. Symptoms of allergic rhinitis, when present, will also typically exacerbate the clinical symptoms of nasal airway dysfunction.
For a thorough cosmetic assessment, physical examination of the previously operated nose should include a careful inspection of both the external and internal nasal anatomy. In addition to the standard external cosmetic parameters of contour, alignment, symmetry, width, length, projection, and rotation, particular attention should also be paid to the physical and biomechanical characteristics of the outer nose, and palpation is an indispensible component of the physical examination. Only palpation will yield information regarding skin thickness, skin elasticity, cartilage strength, sidewall rigidity, tip support, and smoothness of the nasal dorsum. These characteristics are of considerable surgical significance as these physical properties weigh heavily upon the surgical prognosis.
Although important information is obtained through inspection and palpation of the outer nasal tissues, the external nasal attributes tell only part of the story.
Examination of the internal nasal passages is also critically important to the preoperative surgical assessment. Inspection of the nasal vestibule for the presence of cicatricial webs, valvular stenoses, prolapsed crural cartilage, recurvature of the lateral crura, or caudal septal deviations is vital to the complete preoperative assessment of the previously operated nose. In addition, observation of the nose for dynamic nasal valve collapse during normal inspiration is another important part of the physical examination. Findings of dynamic nasal valve collapse are often overlooked on speculum examination and indicate a pathologic weakness of the nasal sidewall—a more common finding in surgically overresected noses. Speculum or fiberoptic examination of the nasal cavum is also a key component of the revision rhinoplasty evaluation. Visual inspection of the nasal mucosa for excessive erythema, rhinorrhea, and edema— the triad of inflammatory findings consistent with allergic rhinitis—should not be overlooked since preoperative allergy treatment may help to reduce both intraoperative bleeding and postoperative mucosal edema. Findings of friable, dry, and heavily crusted mucosa should also be sought since these are tangible signs of decreased vascularity, such as that produced by chronic cocaine abuse, autoimmune vasculitis, or recent surgery. Similarly, visual inspection of the quadrangular cartilage for clinically significant airway obstruction and/or mucosal adhesions (synechiae) is essential since surgical treatment of these fixed anatomic deformities is required for satisfactory functional results. The presence of high (dorsal) deviations of the quadrangular septum should also be sought since a number of cosmetic and functional problems will develop if curvature of the dorsal septum is unrecognized and left untreated. Cotton-swab palpation of the quadrangular cartilage is also recommended to assess intrinsic cartilage strength and to detect potential areas of missing cartilage from previous septal surgery. Stout rigidity throughout the quadrangular septum indicates a reasonable likelihood that surplus septal cartilage is available for cartilage grafting. Septal perforations should also be sought on preoperative examination since large perforations may indicate poor vascularity and compromised structural support of the septal L-strut. While asymptomatic septal perforations do not necessarily require surgical treatment, smaller perforations are often easily eliminated during standard septal surgery and all preexisting anatomic abnormalities should be documented prior to surgical revision. Finally, visual assessment of the inferior and middle turbinates for hypertrophy and obstruction of the internal nasal airway is also necessary for proper functional assessment and treatment.
Examination of the internal nasal passages is also critically important to the preoperative surgical assessment. Inspection of the nasal vestibule for the presence of cicatricial webs, valvular stenoses, prolapsed crural cartilage, recurvature of the lateral crura, or caudal septal deviations is vital to the complete preoperative assessment of the previously operated nose. In addition, observation of the nose for dynamic nasal valve collapse during normal inspiration is another important part of the physical examination. Findings of dynamic nasal valve collapse are often overlooked on speculum examination and indicate a pathologic weakness of the nasal sidewall—a more common finding in surgically overresected noses. Speculum or fiberoptic examination of the nasal cavum is also a key component of the revision rhinoplasty evaluation. Visual inspection of the nasal mucosa for excessive erythema, rhinorrhea, and edema— the triad of inflammatory findings consistent with allergic rhinitis—should not be overlooked since preoperative allergy treatment may help to reduce both intraoperative bleeding and postoperative mucosal edema. Findings of friable, dry, and heavily crusted mucosa should also be sought since these are tangible signs of decreased vascularity, such as that produced by chronic cocaine abuse, autoimmune vasculitis, or recent surgery. Similarly, visual inspection of the quadrangular cartilage for clinically significant airway obstruction and/or mucosal adhesions (synechiae) is essential since surgical treatment of these fixed anatomic deformities is required for satisfactory functional results. The presence of high (dorsal) deviations of the quadrangular septum should also be sought since a number of cosmetic and functional problems will develop if curvature of the dorsal septum is unrecognized and left untreated. Cotton-swab palpation of the quadrangular cartilage is also recommended to assess intrinsic cartilage strength and to detect potential areas of missing cartilage from previous septal surgery. Stout rigidity throughout the quadrangular septum indicates a reasonable likelihood that surplus septal cartilage is available for cartilage grafting. Septal perforations should also be sought on preoperative examination since large perforations may indicate poor vascularity and compromised structural support of the septal L-strut. While asymptomatic septal perforations do not necessarily require surgical treatment, smaller perforations are often easily eliminated during standard septal surgery and all preexisting anatomic abnormalities should be documented prior to surgical revision. Finally, visual assessment of the inferior and middle turbinates for hypertrophy and obstruction of the internal nasal airway is also necessary for proper functional assessment and treatment.
While no two revision rhinoplasty cases share identical nasal anatomy, many revision rhinoplasty patients present with a stereotypical and stigmatic nasal contour resulting from overaggressive excisional rhinoplasty. In fact, the typical revision rhinoplasty patient presents with at least some functional and cosmetic consequences of inadequate structural support stemming from overzealous skeletal resection. Characteristic stigmatic findings include low dorsal height and ill-defined sidewall shadows, pinching of the middle nasal vault and/or nasal tip with corresponding obstruction of the nasal valve, retraction of the alar rims with notching of the alar margins, and asymmetries of the nasal tip due to unequal scarification and collapse of the alar cartilage remnants. Often these deformities are interspersed with untreated deformities of the original nose such as excessive columellar protrusion, overprojection of the nasal spine, derangements in tip projection, or residual segments of dorsal overprojection such as the pollybeak deformity. Although each patient presents with a unique set of cosmetic and functional abnormalities, the vast majority of complex revision rhinoplasty patients present with varying degrees of inadequate skeletal support with or without simultaneous skeletal malposition.
Without question, one of the most important causes of the unsatisfactory rhinoplasty outcome is poor central tip support. In general, noses with naturally weak and/or surgically weakened central tip support are far more prone to adverse rhinoplasty outcomes and to adverse manifestations of alar cartilage overresection. In contrast, patients with vigorous central tip support suffer fewer complications of alar cartilage overresection all other factors being equal (see Case Two). While central tip support is derived in part from direct contributions of the medial crura, as well as from secondary support mechanisms from the surrounding soft tissues, the cartilaginous nasal septum is arguably the most important component of central tip support in most noses. Moreover, in the tension-nose deformity, septal support may comprise the overwhelming majority of structural tip support (14). In a fresh cadaver study examining septal contributions to nasal tip support, Adams and coworkers observed a 3.3-mm average loss in tip projection following isolated (dorsal) septal reductions of 4 mm performed through the open rhinoplasty approach (4). Moreover, even greater losses in tip projection were observed following removal of the entire quadrangular septum. The authors concluded that the septum likely plays a far more significant role in nasal tip support than previously believed, and is likely equal in importance to the lower lateral cartilages and their soft tissue attachments in providing nasal tip support. Consequently, assessing tip support by evaluating the intensity of tip recoil, the strength and rigidity of the anterior septum, and rigidity of the lower lateral cartilages is an essential component of the preoperative nasal exam. By the same token, restoring inadequate central support is one of the most important goals of revision rhinoplasty.
PINPOINTING THE COSMETIC OBJECTIVE WITH COMPUTER IMAGING
Without question, a thorough and methodical physical examination is requisite for a favorable surgical outcome. However, assessing the preoperative anatomy is only half of the equation. The other critical element in the preoperative
assessment is the cosmetic objective—how the nose should appear as a consequence of revision surgery. The surgical prognosis will vary considerably according to the ease or difficulty of the cosmetic objective, and pinpointing the desired cosmetic outcome is an essential component of the preoperative assessment.
assessment is the cosmetic objective—how the nose should appear as a consequence of revision surgery. The surgical prognosis will vary considerably according to the ease or difficulty of the cosmetic objective, and pinpointing the desired cosmetic outcome is an essential component of the preoperative assessment.
The ultimate goal of any rhinoplasty, whether primary or secondary, is satisfying the cosmetic desires of the patient. Aside from the formidable technical challenges of revision rhinoplasty, one of the biggest obstacles to achieving a satisfactory cosmetic outcome is obtaining a clear and unambiguous definition of the desired cosmetic objective. Since there is no universal or “ideal” nasal contour that applies equally to all faces (15), pinpointing each patient’s specific cosmetic desires is a critical aspect of surgical planning. Increasingly, the typical revision rhinoplasty patient is a young adult with very strong cosmetic preferences. And while many patients have passionate opinions regarding nasal length, tip width, or dorsal contour, many patients also have difficulty effectively articulating their precise cosmetic goals. Moreover, most secondary rhinoplasty patients are seeking reassurance that their goals have been understood correctly, and few are willing to empower the surgeon merely to “do what you think is best.”
The advent of computer morphing software, commonly known as preoperative “computer imaging,” is a helpful new technology that can facilitate communication between the revision surgeon and the prospective revision rhinoplasty patient (5, 16). Using standardized, (high-resolution digital) rhinoplasty photographs, combined with computerized morphing software, computer imaging allows the skilled user to electronically edit (or “morph”) rhinoplasty photographs in order to visually depict cosmetic surgical enhancements of the nose. Cosmetic analysis of the nose is greatly enhanced using computer imaging since individual parameters such as projection, rotation, width, or length can be altered, either independently or collectively, to determine the aesthetic impact of surgery upon the overall facial appearance. By incorporating the patient’s cosmetic preferences into the editing process, lifelike simulations are created that enable the patient to “preview” various surgical changes, and ultimately to endorse the overall cosmetic objective. Because the process yields a concrete representation of the desired cosmetic outcome, a relatively unambiguous goal is established, and both the patient and surgeon are assured that the cosmetic objectives have been communicated effectively. Furthermore, the ability to electronically fade between edited images and the corresponding unedited image in real time greatly enhances the analytical power of computer imaging for surgeon and patient alike. For the patient, real-time transformation provides immediate intuitive understanding of the cosmetic deformity and greater reassurance regarding the proposed surgical correction. For the surgeon, the morphed image offers improved diagnostic insights and a mutually agreeable nasal contour from which an individualized treatment plan can be developed and quantified. Although the benefits of computer imaging are irrefutable, computer imaging is subject to potential abuse and/or misinterpretation. Consequently, care must be taken to avoid overoptimistic simulations and to advise all patients that computer-enhanced images represent a best-case scenario, not a guaranteed outcome (5, 16). Nevertheless, while exact recreation of the simulated image is virtually impossible, in skilled hands the final outcome often resembles, or even exceeds, the computer-generated simulation (17). Owing to the many benefits of this new technology, revision rhinoplasty patients now commonly request computer imaging as part of their preoperative surgical assessment.
FINALIZING THE TREATMENT PLAN
Once the cosmetic goal is determined, the final piece of the preoperative assessment is complete. The seasoned revision rhinoplasty surgeon will then carefully collate all of the available information including the patient’s general health, the baseline cosmetic deformity, the biophysical tissue characteristics, the patient’s cosmetic goals, the extent of functional impairment, the psychological status of the patient, and the likely healing tendencies, in order to devise an individualized surgical treatment plan and a corresponding surgical prognosis. As enumeration of the treatment plan becomes increasingly more explicit, the surgical approach (i.e., external vs. endonasal), the anesthetic options, and the choice of autologous graft materials must also be discussed and agreed upon. The surgeon must then decide if the patient’s expectations are realistic and if the treatment objectives are within reach at an acceptable level of surgical risk. The patient’s response to the stated surgical limitations and to the overall prognosis will help to determine if patient expectations are appropriate and sincere. Encouraging the patient to articulate and acknowledge the attendant surgical risks also helps to confirm that risk counseling was effective. Finally, the surgeon should ensure that the patient will comply with all surgical restrictions, care requirements, and follow-up appointments before assuming responsibility for surgical care.
Anesthetic Considerations
Once the decision is made to proceed with surgical treatment, preoperative preparations and restrictions are reviewed with the patient. All platelet inhibitors, including aspirin, nonsteroidal anti-inflammatory drugs, omega fish oils, high-dose vitamin E, and most herbal supplements should be discontinued at least 7 to 10 days prior to surgery to prevent drug-induced clotting disturbances. Tobacco users should be advised to discontinue all nicotine products immediately, and nasal allergies should be treated to reduce preoperative inflammation. A general medical evaluation is recommended for any patient with medical comorbidities or potential anesthetic contraindications.
While the optimal type of anesthesia remains a topic of considerable debate, the author emphatically prefers the use of general anesthesia for nasal surgery, and for revision rhinoplasty in particular. A carefully administered general anesthetic titrated to the age and body mass of the patient offers superior patient comfort, improved hemodynamic control, and optimal protection of the lower airway against the threat of aspiration. However, because secondary rhinoplasty cases are typically of a much longer duration than the average primary rhinoplasty, special precautions are required to prevent sequela of prolonged immobility during general anesthesia. All patients are placed in the semi-Fowler “beach chair” position with the feet and head elevated to facilitate peripheral venous return, and the legs are continuously massaged with sequential compression devices to minimize pooling of venous blood in the lower extremities and thereby reduce the risk of deep vein thrombosis. Pressure points on the heels and elbows are padded liberally, and the head is positioned above the heart to minimize venous back-pressure.
While the cost of general anesthesia is marginally greater, the technical advantages of general anesthesia are numerous. First, general anesthesia virtually eliminates intraoperative patient movement in response to painful stimuli. Because the depth of twilight anesthesia is limited by the need to maintain spontaneous ventilation, a partially conscious patient is often prone to unexpected movements and may even become restless, disoriented, or overtly combative. In contrast, endotracheal intubation safely permits a much deeper level of anesthesia that virtually eliminates intraoperative patient movement. Although judicious infiltration of the nose with 1% lidocaine containing epinephrine is still required for optimal hemostasis, distortion of the nose from large fluid volumes can be minimized since pain control is primarily achieved via the general anesthetic. In addition, blood pressure control is far less challenging in the absence of painful stimuli, and controlled hypotension can be used in healthy patients to improve visualization of the surgical field, to minimize extravasation of blood into the surrounding soft tissues, and to minimize operative blood loss. In contrast, patients under intravenous sedation may feel threatened as a result of anesthetic-induced disorientation and confusion. Blood pressure spikes, excessive bleeding, and defensive movements are common in this scenario and may complicate surgical management. While a skillfully administered intravenous anesthetic can often avoid these problems, susceptibility to apnea varies widely among individuals and general anesthesia eliminates this variable entirely. Finally, the presence of a cuffed endotracheal tube provides enhanced protection of the lower airway against the aspiration of blood which is an ever-present risk in upper airway surgery.
Perhaps the biggest perceived drawback to general anesthesia is the high incidence of postoperative nausea and vomiting (PONV). Moreover, PONV is more common following oral ingestion of blood, which is highly emetogenic and common following nasal surgery. In addition to being unpleasant, PONV may also lead to exacerbations in surgical site edema, ecchymosis, pain, and/or epistaxis, potentially prolonging recovery and intensifying the risk of subcutaneous fibrosis. However, a narcotic- free general anesthetic protocol can dramatically reduce the incidence of PONV (personal observation). After anesthetic induction with intravenous propofol (APP Pharmaceuticals LLC, Schaumburg, IL) and succinyl choline (PharMEDium Services LLC, Cleveland, MS), general anesthesia is maintained throughout the remainder of surgery on sevoflurane (Abbott Laboratories, North Chicago, IL) inhalational anesthetic. During periods of planned stimulation such as during lateral osteotomies, propofol is first administered by bolus to assist in blood pressure homeostasis and labetalol hydrochloride (Hospira Inc., Lake Forest, IL) or nicardipine hydrochloride (Sandoz Inc., Princeton, NJ) are used to supplement blood pressure and/or heart rate control. Dexamethasone sodium phosphate (APP Pharmaceuticals LLC, Schaumburg, IL) is used on induction for prophylaxis against PONV, and a single 4-mg dose of ondansetron (Baxter Healthcare Corporation, Deerfield, IL) is also used 30 minutes prior to extubation for additional PONV prophylaxis. The combined use of dexamethasone and ondansetron has been shown to be more effective at reducing severe PONV than ondansetron alone for both laparoscopic surgery and fentanyl-based patient-controlled analgesia (18, 19). Moreover, by using the narcotic-free general anesthetic protocol described above, postoperative emesis is rare even when oral narcotics are used for postoperative pain control, and most patients are alert and oriented within 10 to 15 minutes of extubation. When used in combination with controlledhypotensive anesthesia, the protocol also has a favorable impact upon postoperative swelling and ecchymosis since the intraoperative tissue extravasation of blood is greatly minimized. Patients typically perceive their surgery as lasting only a few minutes and few have recall of the operating room experience.
SURGICAL RECONSTRUCTION OF THE PREVIOUSLY OPERATED NOSE
Optimal Timing of Revision Rhinoplasty
The optimal timing of secondary rhinoplasty (and the traditional requirement to postpone surgery for 1 year) is a topic of ongoing debate. For virtually any complex secondary rhinoplasty patient, the emotional burden of a prolonged recovery is considerable, and rapid intervention would be far preferable from an emotional standpoint. However, early revision surgery in the face of acute postsurgical inflammation and edema is significantly more complication prone, and is generally best reserved for legitimate medical emergencies. Furthermore, even when the acute
postsurgical changes have resolved, the surgically disrupted capillary and lymphatic microcirculation remains compromised, and complex revision surgery is generally best postponed until soft tissue swelling—the outward manifestation of microcirculatory impairment—has fully resolved. Although waiting a full year before correcting an unsightly postsurgical deformity can result in considerable emotional distress, a healthy microcirculation is essential to any complex secondary rhinoplasty, and the traditional recommendation to postpone revision surgery for 1 year is generally appropriate since significant microcirculatory impairment is often present in the first year after surgery. Moreover, in cases where the nose remains unacceptably large but otherwise shapely, allowing ample time for swelling and edema to resolve may obviate the need for revision surgery altogether since an acceptable cosmetic result often emerges within 12 months. And because surgical swelling is usually far more severe in patients with thick, sebaceous nasal skin, revision rhinoplasty in the ultrathick-skinned patient solely for the purpose of achieving minor size reductions is generally contraindicated for at least 18 to 24 months. Longer healing times are also necessary for patients with significant acne, allergic rhinitis, or other forms of chronic inflammation unless the inflammatory stimulus can be adequately controlled. While prolonged recovery is generally recommended for the thick-skinned or inflammationprone patient, prolonged lymphedema may also give rise to permanent subcutaneous fibrosis, thereby tainting an otherwise satisfactory cosmetic outcome. Consequently, in patients with prolonged swelling, the judicious use of lowdose triamcinolone acetate injections is often necessary to prevent permanent iatrogenic thickening of the nasal skin (20). Although triamcinolone injections can potentially cause significant adverse side effects such as telangiectasias, dermal thinning, and even cartilage absorption, when carefully titrated, low-dose triamcinolone can greatly enhance the cosmetic outcome and obviate the need for revision surgery in the thick-skinned nose.
postsurgical changes have resolved, the surgically disrupted capillary and lymphatic microcirculation remains compromised, and complex revision surgery is generally best postponed until soft tissue swelling—the outward manifestation of microcirculatory impairment—has fully resolved. Although waiting a full year before correcting an unsightly postsurgical deformity can result in considerable emotional distress, a healthy microcirculation is essential to any complex secondary rhinoplasty, and the traditional recommendation to postpone revision surgery for 1 year is generally appropriate since significant microcirculatory impairment is often present in the first year after surgery. Moreover, in cases where the nose remains unacceptably large but otherwise shapely, allowing ample time for swelling and edema to resolve may obviate the need for revision surgery altogether since an acceptable cosmetic result often emerges within 12 months. And because surgical swelling is usually far more severe in patients with thick, sebaceous nasal skin, revision rhinoplasty in the ultrathick-skinned patient solely for the purpose of achieving minor size reductions is generally contraindicated for at least 18 to 24 months. Longer healing times are also necessary for patients with significant acne, allergic rhinitis, or other forms of chronic inflammation unless the inflammatory stimulus can be adequately controlled. While prolonged recovery is generally recommended for the thick-skinned or inflammationprone patient, prolonged lymphedema may also give rise to permanent subcutaneous fibrosis, thereby tainting an otherwise satisfactory cosmetic outcome. Consequently, in patients with prolonged swelling, the judicious use of lowdose triamcinolone acetate injections is often necessary to prevent permanent iatrogenic thickening of the nasal skin (20). Although triamcinolone injections can potentially cause significant adverse side effects such as telangiectasias, dermal thinning, and even cartilage absorption, when carefully titrated, low-dose triamcinolone can greatly enhance the cosmetic outcome and obviate the need for revision surgery in the thick-skinned nose.
Although secondary surgery prior to complete healing is suboptimal, revision surgery within the first year may be preferable in a few rare circumstances. Unlike the otherwise shapely but still-swollen nose for which conservative treatment is appropriate, the overresected or twisted nose that has little hope of spontaneous improvement is sometimes best revised before progressive soft tissue contracture leads to permanent nasal collapse. In these challenging cases, nasal distortion is likely to gradually worsen in the months and years after rhinoplasty due to progressive “shrink wrap” contracture of both the inner and outer epithelial linings. Severely weakened and destabilized skeletal elements subjected to the persistent forces of soft tissue contracture often deform easily, resulting in severe buckling, pinching, retraction, and asymmetry of the cartilaginous framework. And while nonemergent reoperation during the acute phase of postoperative inflammation and edema is generally ill-advised, once the acute changes have passed and the microcirculation has recovered to a reasonable extent, early revision is reasonable—even if a full year has not elapsed—in order to prevent irreversible shrinkage of the nasal skin or mucosa. However, because early revision surgery risks unfavorable wound-healing responses and vascular insufficiency, early reoperation is best reserved for young and healthy individuals with forgiving skin and robust healing tendencies, and not for older patients or those with multiple medical comorbidities. Although the emotionally distressed patient is often seeking early revision, early intervention places additional physiologic stress upon the already damaged nasal tissues, and only the threat of permanent nasal contracture can justify the additional surgical risk. Hence, the decision to intervene early should not be taken lightly, and emotional distress alone is not justification for early surgical revision.
Another scenario in which early revision surgery is preferable is the comparatively minor anatomic deformity presenting in the patient with rapidly healing nasal skin. For the young patient with comparatively thin nasal skin and a smooth healthy complexion, surgical inflammation and swelling often resolve in far less than 12 months. In such patients, persistent skeletal deformities such as a small residual hump may be surgically corrected before the 1-year mark since further delay will not benefit surgical management.
In this scenario, expeditious intervention is reasonable since the emotional impact of a flawed outcome can be remedied sooner at negligible increased risk to the patient. In summary, the 1-year rule is an approximate guideline that is appropriate for some patients and inappropriate for others. And like most aspects of cosmetic nasal surgery, treatment decisions should be made according to the individual physical and psychological needs of the patient, and not according to broad generalizations. For the slowhealing nose, patience is often rewarded with a satisfactory cosmetic outcome in the absence of revision surgery. And while the emotionally distraught patient often pushes for early surgical intervention, sometimes accompanied by anger or hostility, appropriate treatment must not be compromised in the name of expediency. In contrast, early intervention is occasionally justified in the contractureprone patient who exhibits signs of rapid and severe nasal contracture. However, while early intervention may come as welcome news to these challenging patients, such highrisk cases seldom lead to storybook outcomes and a thorough, candid, and well-documented informed consent is mandatory.
AUGMENTATION GRAFTING OF THE OVERRESECTED NOSE
Perhaps the most common presentation in secondary rhinoplasty is severe structural compromise resulting from overresection of the nasal framework. For most patients, the immediate postoperative deformity is characterized by a partially collapsed and noticeably less attractive nose.
However, the initial deformity often eventually gives way to progressive (delayed) contour deformity as postoperative soft tissue contracture and fibrosis further deform the surgically weakened nasal framework. And while the degree of deformity often correlates to the extent of cartilage resection, noses with soft, pliable nasal cartilage are particularly vulnerable to skeletal overexcision since naturally weak cartilage is already near the threshold for skeletal collapse. Indeed, in the susceptible patient with exceedingly soft cartilage, even modest cartilage excision can lead to severe nasal deformities. Moreover, even when the initial rhinoplasty outcome fails to exceed the threshold for skeletal collapse, age or disease-related deterioration in cartilage strength may eventually lead to failure of the surgically weakened framework and subsequent nasal deformity. Because the severity of soft tissue contracture also varies widely among individuals, those with naturally strong contractile forces—often associated with relatively thin nasal skin—are also at increased risk for delayed skeletal deformities, even when they possess comparatively strong nasal cartilage. Likewise, surgical disruption of vital secondary tip support mechanisms will also predispose to iatrogenic deformity unless secondary support mechanisms are adequately reconstituted or compensated at the time of primary rhinoplasty (4). Noses with preexisting skeletal deviations are also potentially more susceptible to overaggressive excisional techniques since aggressive surgical destabilization may exacerbate underlying imperfections of the nasal cartilage, particularly deviation of the dorsal septum. And while a large nasal tip is often equated with strong nasal cartilage, in reality, wide or bulbous alar cartilages are often exceptionally soft, making them highly susceptible to surgical overresection. Without question, durable and dependable skeletal support is fundamental to a stable and reproducible rhinoplasty outcome, and surgical techniques that imperil long-term structural support are far more susceptible to the powerful and persistent forces of wound healing.
However, the initial deformity often eventually gives way to progressive (delayed) contour deformity as postoperative soft tissue contracture and fibrosis further deform the surgically weakened nasal framework. And while the degree of deformity often correlates to the extent of cartilage resection, noses with soft, pliable nasal cartilage are particularly vulnerable to skeletal overexcision since naturally weak cartilage is already near the threshold for skeletal collapse. Indeed, in the susceptible patient with exceedingly soft cartilage, even modest cartilage excision can lead to severe nasal deformities. Moreover, even when the initial rhinoplasty outcome fails to exceed the threshold for skeletal collapse, age or disease-related deterioration in cartilage strength may eventually lead to failure of the surgically weakened framework and subsequent nasal deformity. Because the severity of soft tissue contracture also varies widely among individuals, those with naturally strong contractile forces—often associated with relatively thin nasal skin—are also at increased risk for delayed skeletal deformities, even when they possess comparatively strong nasal cartilage. Likewise, surgical disruption of vital secondary tip support mechanisms will also predispose to iatrogenic deformity unless secondary support mechanisms are adequately reconstituted or compensated at the time of primary rhinoplasty (4). Noses with preexisting skeletal deviations are also potentially more susceptible to overaggressive excisional techniques since aggressive surgical destabilization may exacerbate underlying imperfections of the nasal cartilage, particularly deviation of the dorsal septum. And while a large nasal tip is often equated with strong nasal cartilage, in reality, wide or bulbous alar cartilages are often exceptionally soft, making them highly susceptible to surgical overresection. Without question, durable and dependable skeletal support is fundamental to a stable and reproducible rhinoplasty outcome, and surgical techniques that imperil long-term structural support are far more susceptible to the powerful and persistent forces of wound healing.
Until recently, “excisional” rhinoplasty techniques have been the workhorse of cosmetic nasal surgery. Traditional methods for reduction of the wide nasal tip and/or rotation of the ptotic tip have relied upon aggressive resection of the lateral crura—the so-called cephalic trim technique. Often the cephalic trim is combined with resection of the anterior septal angle, presumably to achieve still greater tip rotation. Sadly, these techniques are more often destructive, rather than constructive, as surgical reduction in skeletal support frequently exceeds the threshold for long-term structural stability. Although excisional techniques may yield acceptable surgical outcomes in select circumstances, the practice of excising vital skeletal tissues to refine the nasal contour is a risky and unpredictable undertaking, and a disproportionate number of adverse rhinoplasty outcomes are probably the result of overaggressive cartilage excision. Indeed, aggressive destabilization of the nasal framework can severely degrade and weaken skeletal support eventually resulting in stigmatic and unsightly deformities of the nasal contour. In fact, even seemingly trivial reductions in structural support can lead to skeletal collapse in the highly predisposed patient. Yet the strong association between excisional techniques and nasal contour deformities has done little to discourage the use of excisional methods as many practitioners still perform and teach only aggressive excisional techniques. Moreover, since both the severity of soft tissue contracture and the threshold for cartilage collapse cannot be reliably determined in advance, and since arbitrary limits for cartilage excision may fail to account for age-related reductions in cartilage strength, the long-term outcome of excisional rhinoplasty is at best haphazard and unpredictable. Fortunately, an improved understanding of nasal tip dynamics and a growing recognition of the harmful effects of overzealous cartilage removal is prompting a gradual shift away from excision-based techniques and toward the adoption of safer and more reliable surgical alternatives. As a result, the unpredictable and somewhat risky practice of aggressive cartilage excision is slowly being supplanted by techniques that conserve nasal cartilage and reliably enhance tip contour with far less risk of skeletal degradation.
OPTIONS FOR SKELETAL TISSUE REPLACEMENT
In the overwhelming majority of revision rhinoplasty cases skeletal support has been severely compromised and damaged or missing skeletal tissues must be surgically reconstituted in order to restore satisfactory nasal contour and function. As a consequence, the skillful and adept use of autologous tissue grafts has become the mainstay of revision rhinoplasty. In addition to a familiarity with the biophysical properties and limitations of various graft materials, successful tissue grafting demands a working knowledge of the proper harvest, fabrication, and fixation of each graft material. Although accomplished rhinoplasty surgeons may use specific graft materials differently, the fundamental tenets of graft harvest and application must be followed regardless of the material selected or the specific method of application.
Despite the potential risk of infection, resorption, warping, migration, and other complications associated with autologous graft materials, autografts remain the gold standard in secondary rhinoplasty owing to their long-term safety and reliability. However, synthetic implant materials, while controversial, are growing in popularity as an alternative to autologous tissue grafts. In primary augmentation rhinoplasty, porous synthetic polymers, most notably expanded-polytetrafluoroethylene (Gore-Tex, W.L. Gore & Associates Inc., Flagstaff, AZ) and high-density porous polyethylene (Medpor, Porex Surgical Inc., Newnan, GA) have been used successfully for dorsal augmentation with comparatively few initial complications, particularly in comparison to traditional nonporous (silicone) implants (21, 22, 23, 24). More recently, the use of porous polyethylene has expanded to include placement in the lower third of the
nose for both functional and cosmetic purposes (25



nose for both functional and cosmetic purposes (25
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree