Refraction in Infants and Children
Michael X. Repka
THE MANAGEMENT OF refractive error is the most common problem faced by the ophthalmologist examining pediatric patients. Children present with symptoms of blurred vision, inability to read, sitting too close to the television, squinting, or poor performance in school. They may have been referred by a primary care provider or after a failed school screening examination. In addition to subnormal vision, children may complain of ocular fatigue, inability to study, letter reversal while reading and writing, and reading difficulty. Many will have normal eye and ocular motility examinations. For many only reassurance is necessary, while others will have a refractive problem.
DETERMINATION OF VISUAL ACUITY AND REFRACTIVE ERROR
Accurate measurement of refractive error is an essential component of the pediatric eye examination. Refractive error change during childhood mandates frequent rechecks. For instance, an aphakic infant may require monthly examinations, whereas yearly checks are sufficient for most myopic teenagers. Refraction of a child cannot be rushed and should rely on objective techniques rather than on the subjective techniques used in adult practice. The examination is generally carried out with the parents present. It is best for young children to sit on a parent’s lap. Older children may prefer to sit alone, as long as a parent or other familiar person is present. The room should not be completely darkened, as this may provoke anxiety (Fig. 5.1).
Visual acuity was considered to be essentially absent at birth, only 6 decades ago (1) Optokinetic nystagmus (OKN) measurements in the late 1950s showed this belief to be erroneous (2). Visual-evoked potential (VEP) acuities have been found to range from 20/200 to 20/100 at birth and to reach 20/20 by 1 year of age. Preferential looking techniques have demonstrated acuities of approximately 1 cycle per degree at birth (20/400), rapidly improving to adult levels of 30 cycles per degree by 30 months (3). Linear letter acuity is normally 20/40 by age 3 and 20/30 by age 4 or 5 years (3). By 7 years of age, most children have achieved 20/20 line acuity.
Acuity in the Preverbal Child
Measurement of visual acuity is normally performed in the course of determining the refractive error. In most children less than 2.5 years of age, preverbal methods must be used (4). Clinical methods for infants involve an estimate of fixation and following behavior (Fig. 5.2). A penlight is never used as a target since it lacks the edge contours necessary for accurate detection. Instead, the test target should incorporate high-contrast edges, e.g., stripes or a checkerboard. Perhaps the best target for an infant is the examiner’s face. An infant normally displays a visual preference for the human face. For the child of 6 months and older, an interesting toy should be used. Monocular fixation normally can be demonstrated at term and certainly should be present by the end of the first month of life. Following behavior refers to a qualitative assessment of the competence the infant demonstrates in following a moving target. The smoothness and amplitude of pursuit rapidly improves during the first 6 months of life. Careful observation for the presence of a fine nystagmus should be part of each examination. Some practitioners prefer to describe the quality of the fixation behavior with the terms “central,” “steady,” and “maintained.” Maintained fixation implies that the patient will maintain fixation with the same eye after a blink. No matter how fixation is described, the examiner also assesses the binocular fixation pattern to determine if there is an eye preference. A difference suggests a problem in the less preferred eye. One scheme is listed in Table 5.1, adapted from Zipf (4), in which categories A and B are considered normal, while C and D suggest amblyopia. However, there is considerable overlap between these grades, and the test appears to consistently overdiagnose amblyopia (5,6).
In an attempt to improve upon fixation preference testing with an objective, quantitative method of assessing visual function, techniques utilizing grating targets of varying spatial frequency (stripe width) have evolved. Such methods rely on detection of resolution acuity, a more sophisticated measure of visual performance than mere detection of a target as used for fixation assessment. There are three methods currently used for determining resolution acuity. They rely on preferential looking techniques, eliciting and detecting OKN, or recording a VEP.
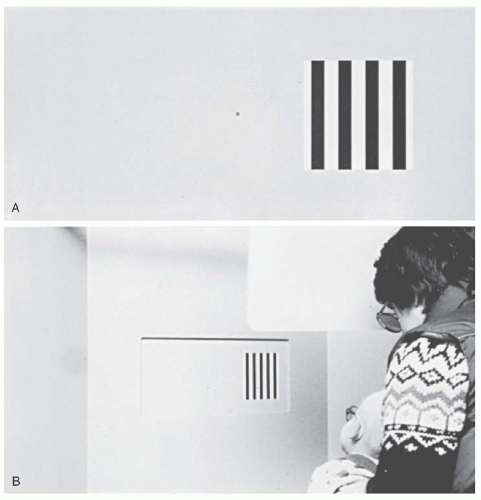
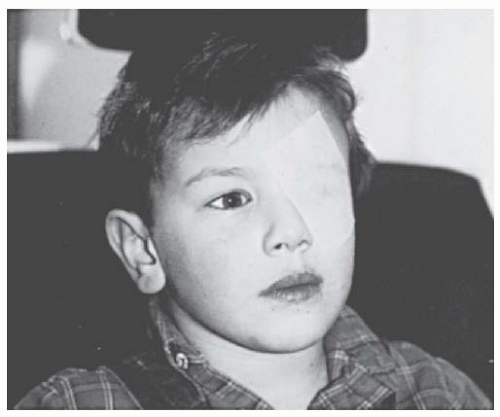 FIGURE 5.1. Examination of the preschooler. The patient is seated comfortably in a partially darkened room. The left eye is occluded with paper tape. |
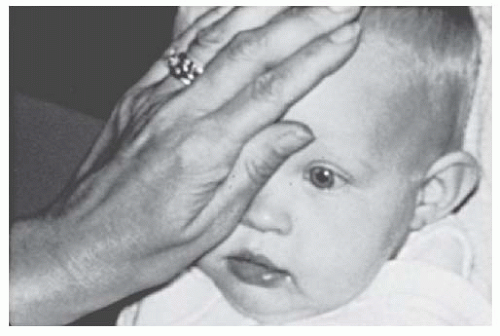 FIGURE 5.2. Fixation preference. The examiner is testing the monocular fixation pattern of an infant by using an attractive toy. |
The most widely used test is preferential looking. Forced-choice preferential looking (3), operant preferential looking (7), and current variations of the acuity card procedure have been developed to provide a simple, efficient method of assessing visual acuity in infants, young children, and nonverbal patients (Fig. 5.3) (8,9). Each of these methods assumes that the child prefers to look at an area of higher visual interest, the striped grating, rather than a neutral gray field. By determining the smallest width grating on which the patient will fixate, resolution acuity can be determined. Normative data for these tests can be used to translate these spatial resolution values to approximate Snellen acuity (8,10). There are wide ranges in normal, especially among the youngest children.
Preferential looking methods require time and specially trained personnel. These methods are not suitable as screening tools. The acuity card testing required 36 minutes for testing of the monocular and binocular acuity of one patient (9). The acuity card procedure seems most useful for monitoring amblyopia therapy in children with severe unilateral abnormalities (e.g., monocular aphakia).
Table 5.1 GRADING SCHEME FOR FIXATION PREFERENCE TESTINGa | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||
Visual acuities in infants have also been measured with VEP recordings or eliciting OKN in response to stripes of various widths. These two methods are handicapped by the complicated apparatus necessary for their performance. The OKN method is additionally handicapped by its reliance on a normal ocular motor system for end-point determination. The usefulness of VEP is diminished by its reliance on a dedicated technician. An additional concern with VEP is that acuities determined by it are better than those determined by behavioral methods because VEP bypasses neural processing to determine a response end point. All three resolution methods for assessing visual acuity (forced-choice preferential looking, VEP, and OKN) are further hampered by their overestimation of visual acuity even among normal individuals (10). Unfortunately, this is the exact infant for whom the development of this type of test is most important.
Between 1 and 3 years of age, visual acuity remains difficult to measure. Behavioral techniques are too time consuming to maintain an active toddler’s interest, although limited success has been reported with the acuity card procedure (9). Other tests for this age range are reviewed by Simons (11)
and McDonald (12). Most clinicians have found these to be insufficiently reliable, and they continue to rely on assessment of fixation behavior until the child is 3 years old.
and McDonald (12). Most clinicians have found these to be insufficiently reliable, and they continue to rely on assessment of fixation behavior until the child is 3 years old.
Acuity in the Older Child
After the age of 2.5 years, children will increasingly be able to read a chart to determine their visual acuity. These tests measure recognition acuity: the ability to differentiate one stimulus from a group of similar stimuli.
The particular test used, as well as the method of presentation, should be the most complex to which the patient can respond consistently. Comparison of visual acuities from visit to visit must take into account the specific test performed as well as the child’s reliability during each examination.
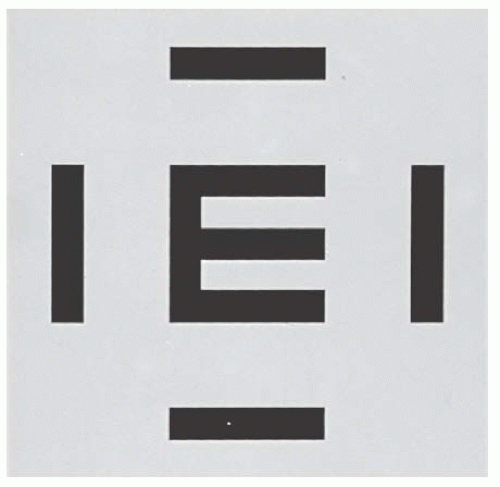
For any test of children’s vision, the method of optotype presentation may affect the measured acuity. Give adequate time and remove as much distraction from the exam room as possible. The testing distance should be 3 m rather than 6 m because of better testability. Presentation of a line of characters or surrounded single optotypes (Fig. 5.4) is preferable. These two methods produce similar results (13). Single letter
presentation eliminates contour interactions around the test optotype, which results in improvement in the measured visual acuity in both normal and amblyopic eyes (11). This effect is clinically termed “the crowding phenomenon.” The effect is greater in amblyopic eyes; thus, a patient with amblyopia may not be detected when tested with single optotypes.
presentation eliminates contour interactions around the test optotype, which results in improvement in the measured visual acuity in both normal and amblyopic eyes (11). This effect is clinically termed “the crowding phenomenon.” The effect is greater in amblyopic eyes; thus, a patient with amblyopia may not be detected when tested with single optotypes.
The test most commonly used for the youngest children involves picture optotypes (Fig. 5.5A), as they are more easily tested in young children. However, these tests even with surround bars are less sensitive to intereye acuity disparity than letter optotypes, and thus may not detect all cases of decreased vision. Hyvarinen invented a set of symbols (house, square, apple, circle) modeled on the Landolt C (Fig. 5.5B) (14).
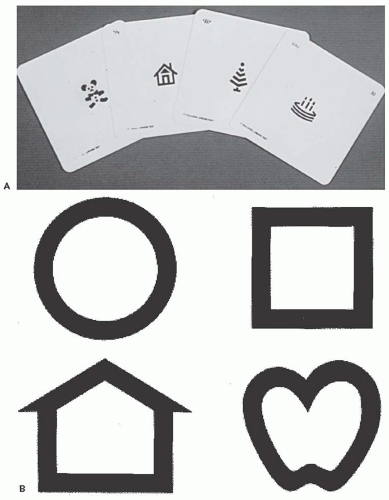 FIGURE 5.5. Picture optotypes. A: Traditional Allen pictures. These picture optotypes are not preferred. B: Lea symbols. |
Single surrounded HOTV tests are of great utility in the 30 to 54-month age group. The patient matches the letter being displayed to one on a handheld card. Consequently, recognition but not literacy is required for this letter optotype test. The method of presenting the HOTV stimuli has been formalized in a protocol developed for the Amblyopia Treatment Studies (15). An automated version of the Amblyopia Treatment Study HOTV test is being used in many centers to provide consistent visual acuity determinations (Fig. 5.6) (16). The Lea symbols in a chart format have been compared to the automated HOTV test among children 3 to 3.5 years of age (17). Equally high proportions were successfully tested. However, children tested 2.5 lines better with the HOTV test, most likely because the
multiline Lea chart was used. In clinical practice, the Lea symbols have fared much better when tested in a single crowded optotype format (18).
multiline Lea chart was used. In clinical practice, the Lea symbols have fared much better when tested in a single crowded optotype format (18).
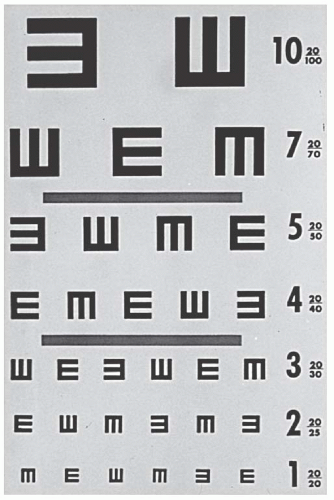
After 4 years of age, the single surrounded HOTV, letters, or tumbling-E test is used (Fig. 5.7). The E test was first devised by Snellen and while widely accepted as a standard, it is not recommended because it tends to be confusing for young children.
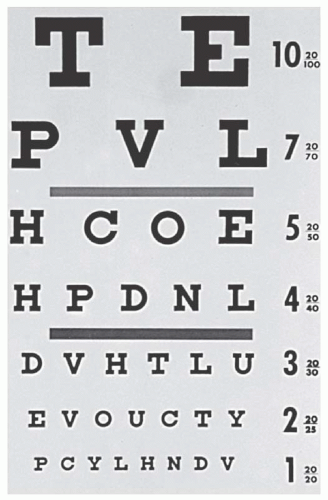
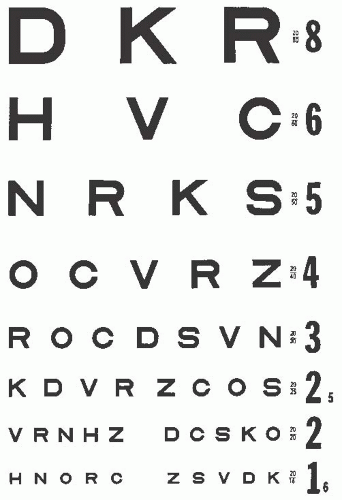
The most commonly used letter visual acuity test is one of the modifications of the Snellen chart (Fig. 5.8). The Snellen chart is not ideal as it employs letters of different legibility at the same visual angle and a scale that changes with unequal steps. A better letter test was designed by Sloan consisting of ten letters of approximately equal legibility (Fig. 5.9) (19). These letters have been used in the Early Treatment of Diabetic Retinopathy Study acuity test (20).
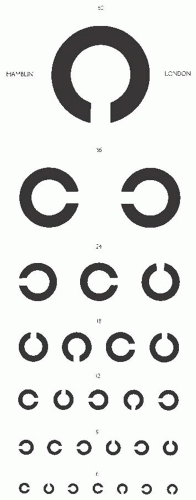
A standard optotype test of visual acuity is the Landolt C (Fig. 5.10). The subject identifies the orientation of the opening in the letter. This test, to date has met with limited clinical acceptance and is not useful in young children.
TECHNIQUE OF REFRACTION
Refraction of children is difficult because of their apprehension and brief attention spans. Consequently, the refraction must be both rapid and accurate. Despite the development of objective automatic refracting instruments, objective retinoscopy remains the best method of determining a child’s refraction. Retinoscopy is usually performed without sedation or a lid speculum, although conscious sedation or even general anesthesia may be required to perform accurate retinoscopy for some children.
Retinoscopy
The techniques of estimating refractive error taught by Copeland are used infrequently today. Most practitioners prefer neutralization methods using loose lenses in infants and young children, and trial frames or a phoropter in older children and teenagers. Retinoscopy is best performed with cycloplegia. When no cycloplegic agent is used, the retinoscopic refraction is termed “manifest” or dry. For such a refraction to be accurate, the patient’s accommodation must be controlled, usually by having them view a distant, nonaccommodative target such as a target light. Optotypes are unsuitable targets since the accommodative mechanism will respond to retinal blur, constantly adjusting the level of accommodation in an attempt to focus the image.
It is useful to attempt a manifest refraction of school-age children and teenagers before dilation if there is evidence of undiagnosed hypermetropia. If a large hyperopic error is confirmed during the cycloplegic refraction, the examiner will know about how much hyperopic correction the patient will tolerate and prescribe accordingly. This may eliminate the need for the patient to return for a post-cycloplegic manifest refraction.
Cycloplegic Refraction
The cycloplegic refraction is an integral part of the examination of each pediatric patient. In addition to determining
refractive error, the instillation of the cycloplegic agent allows a thorough retinal exam. Selection of the cycloplegic agent depends on the age of the patient as well as the pigmentation of the iris. Cycloplegia in children more than 4 months of age is obtained by placing one drop of proparacaine HCl 0.5% in the inferior fornix of each eye, followed by one drop of cyclopentolate 1%. The use of a topical anesthetic before instillation of the cycloplegic drug enhances the cycloplegic effect. This is due to either reduction of reflex tearing and lid squeezing or alteration of the corneal epithelial barrier (21). The refraction is performed 35 to 40 minutes later. For preterm infants, a weaker cycloplegic agent is recommended such as a combination of 0.2% cyclopentolate and 1% phenylephrine. For term to 4-month-old infants, 0.5% cyclopentolate is satisfactory, although phenylephrine is also needed with darker irides. Use of the weaker agents reduces the systemic side effects, especially vomiting. In the case of smaller babies in the neonatal intensive care unit, care should be taken to examine them shortly before a feeding when the stomach is empty.
refractive error, the instillation of the cycloplegic agent allows a thorough retinal exam. Selection of the cycloplegic agent depends on the age of the patient as well as the pigmentation of the iris. Cycloplegia in children more than 4 months of age is obtained by placing one drop of proparacaine HCl 0.5% in the inferior fornix of each eye, followed by one drop of cyclopentolate 1%. The use of a topical anesthetic before instillation of the cycloplegic drug enhances the cycloplegic effect. This is due to either reduction of reflex tearing and lid squeezing or alteration of the corneal epithelial barrier (21). The refraction is performed 35 to 40 minutes later. For preterm infants, a weaker cycloplegic agent is recommended such as a combination of 0.2% cyclopentolate and 1% phenylephrine. For term to 4-month-old infants, 0.5% cyclopentolate is satisfactory, although phenylephrine is also needed with darker irides. Use of the weaker agents reduces the systemic side effects, especially vomiting. In the case of smaller babies in the neonatal intensive care unit, care should be taken to examine them shortly before a feeding when the stomach is empty.
Many examiners consider atropine the most complete cycloplegic agent for children, especially for those with accommodative forms of esotropia. In a series of 120 patients with accommodative esotropia, Rosenbaum and coworkers found an average of 0.34 diopter more hyperopia with atropine 1% administered over 3 days compared with two drops of 1% cyclopentolate (22). They also noted that the difference between the cyclopentolate and atropine cycloplegic refractions tended to be greater for esotropic patients with hypermetropia greater than 2.00 diopters. Nonetheless, most practitioners continue to reserve atropine for those patients who fail to be adequately cyclopleged, despite two or three doses of cyclopentolate. Because of the potential for under correction with cyclopentolate, any patient who inadequately responds to a hyperopic correction or whose refractive esotropia decompensates should undergo a repeat cycloplegic refraction. It is common to find additional hyperopia at the second refraction.
If the examiner elects to use atropine, care should be taken. Atropine is administered by the parent or guardian usually as 1% ointment or solution twice daily for 3 days before the retinoscopic evaluation. It is important to instruct the parent not to instill the ointment the day of the evaluation, as the ointment vehicle will make retinoscopy nearly impossible. The parents should be instructed to store atropine, especially the solution, well away from children. Each drop of 1% solution contains 0.5 mg of atropine.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree