Purpose
To assess the efficacy of intravitreal 0.5 mg ranibizumab for the treatment of center-involving macular edema secondary to branch retinal vein occlusion (BRVO) over 1 year compared with standard-of-care grid laser.
Design
A prospective randomized controlled clinical trial.
Methods
A total of 36 patients with vision loss in 1 eye attributable to macular edema following BRVO were recruited from 5 institutions. Patients were randomized 1:1 to a treatment group that received 6 monthly injections of 0.5 mg ranibizumab and thereafter monthly as needed based on best-corrected visual acuity (BCVA) and central foveal thickness (CFT) assessments on optical coherence tomography scans, or a standard-of-care group that received monthly sham injections for the 1-year duration of the study. Grid laser was administered at 13 and 25 weeks in both groups if criteria for laser treatment were met. Main outcome measures included mean change in BCVA in Early Treatment Diabetic Retinopathy Study (ETDRS) letter scores from baseline to month 12. Secondary outcomes included anatomic outcomes and the percentage of patients requiring grid laser in both groups.
Results
Mean BCVA change from baseline was significantly greater in the treatment compared with the standard-of-care group at 12 months (12.5 ETDRS letters vs -1.6 ETDRS letters, P = .032). The mean CFT was significantly reduced in the treatment compared with standard-of-care group (361.7 μm vs 175.6 μm, P = .025). At 13 and 25 weeks, more patients in the standard-of-care group (68.4%, 50.0%) received grid laser than in the treatment group (6.7%, 8.3%). No new ocular or systemic adverse events were observed.
Conclusions
Compared with standard grid laser, intravitreal ranibizumab provided significant and sustained benefits in visual acuity gain and anatomic improvement in eyes with macular edema secondary to BRVO.
Retinal vein occlusion, the second most common cause of retinal vascular blindness after diabetic retinopathy, affects approximately 16 million people worldwide. It affects approximately 1% of individuals below 60 years, with increases in prevalence to 5% in those over 80 years.
Branch retinal vein occlusion (BRVO) accounts for 80% of all vein occlusions. Without treatment, it can lead to a sustained loss of vision, with a reported final mean visual acuity of 20/70 with 23% of patients having a visual acuity ≤20/200. The cause for the vision loss in BRVO is predominantly attributable to macular edema. Since the publication of the Branch Vein Occlusion Study (BVOS) 25 years ago, grid laser photocoagulation has been the standard of care for BRVO-associated macular edema. In this study, treatment of macular edema following BRVO with grid laser resulted in ≥2 lines of visual acuity (VA) improvement in 65% of eyes compared with 37% of untreated eyes at the 3-year primary endpoint. In the last 5 years, several new treatments for macular edema secondary to BRVO have been evaluated in randomized clinical trials. This included intravitreal triamcinolone injections, intravitreal dexamethasone implants, and inhibitors of vascular endothelial growth factor (VEGF) agents. Of these, anti-VEGF agents have been the most promising. In the Ranibizumab for the Treatment of Macular Edema following Branch Retinal Vein Occlusion (BRAVO) study, rapid and sustained visual improvement was seen in the first 6 months in patients who received monthly 0.3 mg and 0.5 mg ranibizumab compared with sham injections. At the 6-month primary endpoint of the study, the mean gain from baseline best-corrected visual acuity (BCVA) letter score was 16.6 and 18.3 Early Treatment Diabetic Retinopathy Study (ETDRS) letters in the 0.3 and 0.5 mg ranibizumab cohorts, respectively, compared with 7.3 letters in the sham group. After the initial 6 months, treatment with ranibizumab was given on an as-needed basis in all patient groups in the second 6-month observation period. The results from months 6-12 of the study showed maintenance of the visual gain that was achieved in the ranibizumab groups at the 1-year endpoint. An improvement in BCVA, although to a lesser extent, was also seen in the sham group. However, BRAVO was limited by a study duration of only 6 months and did not directly compare the effectiveness of intravitreal ranibizumab against grid laser, the current standard of care at that time. This may be relevant as a previous trial, the Standard Care versus Corticosteroid for Retinal Vein Occlusion study (SCORE), failed to show any superiority of intravitreal triamcinolone injections over grid laser for treating macular edema secondary to BRVO. This led the authors to recommend that grid laser should be the benchmark against which other treatments are compared in clinical trials investigating treatment for vision loss attributable to macular edema following BRVO.
In this randomized controlled clinical trial, we evaluated the efficacy and safety of monthly 0.5 mg intravitreal ranibizumab compared to standard-of-care conventional grid laser over a 1-year period in patients with vision loss attributable to perfused macular edema following BRVO.
Methods
Study Design
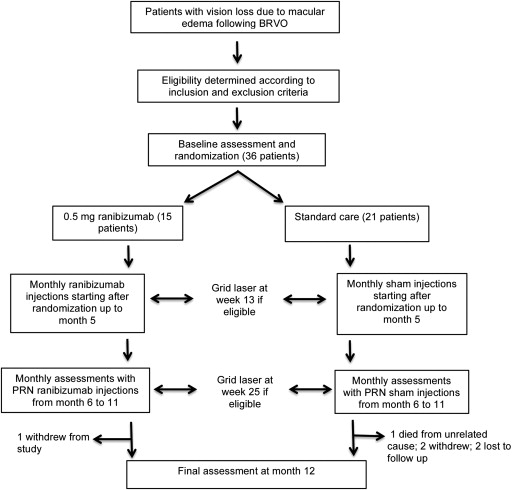
We conducted a 12-month, masked, randomized, placebo-controlled study across 5 centers designed to evaluate the efficacy and safety of monthly intravitreal injections of 0.5 mg ranibizumab vs standard of care with conventional laser grid in patients with vision loss attributable to perfused macular edema following BRVO ( Figure 1 ). Patients were assessed and eligibility determined by the investigating physicians at the individual study sites according to a predistributed study manual. Recruited patients underwent baseline assessment for best-corrected visual acuity (BCVA) and retinal edema prior to randomization. Patients were then randomized 1:1 into 1 of 2 study groups: those treated with intravitreal injections of 0.5 mg ranibizumab for 6 months and thereafter with monthly injections as needed, in combination with standard of care; and those treated with standard of care only. Standard of care consisted of observation with laser grid treatment being allowed at 13 and 25 weeks into the study period according to the BVOS protocol. Sector or pan-retinal laser for neovascularization of either the retina or iris was allowed at the investigating physician’s discretion. The study adhered to the tenets of the Declaration of Helsinki and was performed according to the principles of Good Clinical Practice (Chapter 2 of the International Conference on Harmonization Harmonized Tripartite Guideline for Good Clinical Practice) and national regulations about clinical studies. The study protocol was approved by institutional review board and health research ethics committee at each study site (Sir Charles Gairdner Hospital Human Research Ethics Committee for the Lions Eye Institute, Perth; Royal Victorian Eye and Ear Hospital Human Research Ethics Committee for the Royal Victorian Eye and Ear Hospital, Melbourne; South Eastern Sydney and Illawarra Area Health Service Human Research Ethics for Save Sight Institute, Sydney; Tasmania Health and Medical Human Research Ethics Committee for Hobart Eye Surgeons, Tasmania; and Royal Australian and New Zealand College of Ophthalmologists Human Research Ethics Committee for Central Sydney Eye Surgeons, Sydney). All patients provided written informed consent prior to participation in the study. The trial was registered at Australian New Zealand Clinical Trials Registry, ANZCTR (registration number ACTRN12607000262404).
Study Population
Between August 2007 and September 2011, 36 treatment-naïve patients meeting the inclusion and exclusion criteria and presenting with unilateral visual loss of 6 weeks to 9 months duration secondary to perfused macular edema from BRVO were recruited into the study. Patients were recruited from retina clinics of the Lions Eye Institute Perth, Royal Victorian Eye and Ear Hospital Melbourne, Save Sight Institute Sydney, Central Sydney Eye Surgeons and Hobart Eye Surgeons, Tasmania. The inclusion and exclusion criteria are summarized in Table 1 . These patients comprised the intention-to-treat population, in whom the last-observation-carried-forward method was used for missing data for all efficacy parameters.
| Key Inclusion Criteria | Key Exclusion Criteria |
|---|---|
Patients presenting with vision loss attributable to macular edema following BRVO a with the following characteristics:
|
|
a BRVO is defined as the clinical evidence of retinal hemorrhages and telangiectasia in 1 quadrant or less of the retina accompanied by dilation and tortuosity of the affected venous system.
Randomization
Enrolled patients were randomly assigned with equal probability to receive either intravitreal ranibizumab injections or standard of care using sequentially numbered, sealed opaque envelopes containing the treatment assignment issued centrally by the trial coordinator at the Lions Eye Institute to each study site. The treatment assignments were compiled using a list of computer-generated pseudo-random numbers of variable block size. Patients were randomized for treatment in 1 eye only. Patients, evaluating physicians, certified visual acuity examiners, and staff who performed optical coherence tomography (OCT) and fluorescein angiography were masked to the treatment allocation.
Follow-up Visits and Assessments
Baseline assessment was performed 14 days prior to randomization and the administration of the sham or study intravitreal injection. This consisted of a full ophthalmic examination including BCVA measurement, tonometry, gonioscopy, dilated fundus examination, OCT assessment of the macula, fluorescein angiography, and color fundus photographs. Patients also provided a full medical and drug history and underwent a physical examination. Follow-up visits took place every month after the baseline assessment and first injection for the 12-month duration of the study. At each follow-up visit, BCVA was measured and patients were given a complete ophthalmic examination with OCT assessment of the central foveal thickness (CFT). From months 1-5 after the first injection, patients received injections of either ranibizumab or sham at each follow-up visit. From months 6-11, patients received an injection only if the prespecified anatomic and functional criteria for re-treatment were met. All patients received a telephone call 3 days after the intravitreal injection to assess for any ocular or systemic side effects. At weeks 13 and 25, grid laser treatment was administered to residual areas of edema if predetermined criteria (described in the Laser Grid Photocoagulation section) were met. At month 12, fluorescein angiography and color fundus photographs were taken in addition to the regular follow-up assessments. The BCVA was measured using a 4-meter ETDRS backlit lighthouse chart by a trained vision examiner. OCT was obtained using Stratus OCT (Carl Zeiss Meditec, Inc, Dublin, California, USA), available at the various study centers. The Fast Macular Thickness acquisition protocol was used to perform the scans and to determine the average thickness of the central 1-mm subfield of the macula. All adverse events, whether volunteered by the patient or detected by other means, were recorded and followed as appropriate. Patients experiencing serious adverse events attributed to possible anti-VEGF effects were required to discontinue the study. Any serious adverse event occurring after informed consent was obtained and, until 4 weeks after the patient stopped study participation, was recorded and followed up.
Intravitreal Injections
Patients assigned to the ranibizumab group received intravitreal injections of 0.5 mg ranibizumab under sterile conditions in a minor procedures room as outpatients. Eyes assigned to the standard-of-care group were prepared in the same way but received sham injections performed with a needleless hub of an empty syringe pushed firmly against the eye to simulate an injection. The intravitreal injection procedures were performed according to the Royal Australian and New Zealand College guidelines for intraocular injections ( http://www.ranzco.edu/images/documents/policies/Guidelines_for_Performing_Intravitreal_Therapy1.pdf ). Patients received their assigned treatment within 14 days following baseline assessment and at each monthly follow-up visit thereafter, for a total of 6 injections. From months 6-12, patients were given an injection of their randomized treatment if 1 or more of the following criteria were met: a loss of ≥5 letters from month 5 visit; an increase of ≥150 μm in the mean central subfield thickness on OCT from month 5 visit or at the investigating physician’s discretion.
Laser Grid Photocoagulation
Patients were assessed for macular laser grid treatment according to the precedent BVOS protocol at week 13 and week 25 of the study by the masked investigating physician. Treatment with standard grid laser was given at these 2 time points if the following criteria were met: Snellen visual acuity of ≤20/40, persistence of macular edema with mean central subfield thickness of ≥250 μm, BCVA gain of <5 letters compared to baseline visual acuity. Patients who did not meet the specified criteria received sham laser in the form of 500 μm, 50 mW spots applied to the far peripheral retina.
Outcome Measures
The primary efficacy outcome measure was the mean change from baseline BCVA letter score between the ranibizumab group and standard-of-care group at 12 months. The secondary outcome measures included the mean change from baseline BCVA over time, percentage of patients who gained or lost ≥15 letters from baseline BCVA, mean change from baseline CFT at 12 months and over time, and the percentage of patients with CFT ≤250 μm at 12 months. Other efficacy outcome measures included the percentage of patients who achieved Snellen equivalent BCVA ≥20/40 (70 letters) and Snellen equivalent BCVA ≤20/200 (35 letters) at 12 months, the percentage of patients with residual macular edema (CFT ≥250 μm) at 12 months, and the percentage of patients requiring grid laser treatment at 13 weeks and 25 weeks. Safety outcomes recorded the incidence and severity of ocular and systemic adverse events and any serious adverse events.
Statistical Analysis
Assuming a 10% improvement rate for the standard-of-care group, we calculated the sample size required to detect a 45% difference between the ranibizumab group and standard-of-care group in the proportion of eyes that showed visual acuity gain of greater than 10 letters at 1 year. A sample size of 19 patients in each arm was estimated to give an 80% power of detecting this difference as significant at the 2-sided 5% level if all eyes were from different subjects. Adjusting for a drop-out rate of 10%, we planned to recruit 21 eyes per group.
Statistical analysis was performed with commercial software (SPSS, ver.20; SPSS Inc, Chicago, Illinois, USA). Descriptive statistics were used to summarize patient demographics and baseline ocular characteristics. Independent t test was used for comparison of means and χ 2 or Fisher exact test was used for comparison of proportions between groups. All statistical tests were 2-sided while 1-tailed test (increased power) was also presented for hypothesis with prior assumption of effect in 1 direction. Cochran-Armitage test for linear trend was used to test for a linear trend in distribution of outcome (ordinal categories of letters gained or loss at 12th month) across treatment types. P value < .05 was considered as statistically significant.
Results
Baseline Characteristics and Patient Demographics
Thirty-six eyes of 36 patients were assigned randomly to receive intravitreal injections of 0.5 mg ranibizumab (n = 15) or standard-of-care treatment (n = 21) at 4 centers. Demographic and baseline characteristics were well matched between the 2 groups and are listed in Table 2 . No statistically significant differences were found between the groups for any of the characteristics measured. The flow of patients through the study is shown in Figure 1 . The average age of patients was 68 years (range 41–87 years), and 53% (19 of 36 patients) were female. There was a predominance of white patients in the study group (92% [33 of 36 patients]). The mean time from diagnosis of BRVO to the baseline examination was 16.3 weeks (median 14, range 4-39 weeks). The majority (56% [20 of 36 patients]) of patients were diagnosed ≤3 months prior to inclusion into the study. The mean study eye BCVA at baseline was 44.2 ETDRS letters (range 27–75 letters); approximate Snellen equivalent 20/125. The average CFT at baseline as measured by OCT was 559.4 μm (range 263–1419 μm). The average disc area of capillary nonperfusion seen on fluorescein angiography in the study eye was 3 disc areas (range 0–10).
| Parameter | Baseline | ||
|---|---|---|---|
| Standard of Care (n = 21) | Ranibizumab (n = 15) | All (n = 36) | |
| Age (y ± SD) a | 66.7 ± 10.7 | 69.6 ± 11.6 | 67.9 ± 11.0 |
| Sex, n (%) | |||
| Male | 9 (42.9) | 8 (53.3) | 17 (47.2) |
| Female | 12 (57.1) | 7 (46.7) | 19 (52.8) |
| Race, n (%) | |||
| White | 19 (90.5) | 14 (93.3) | 33 (91.7) |
| Asian | 2 (9.5) | 0 | 2 (5.6) |
| Aboriginal | 0 | 1 (6.7) | 1 (2.8) |
| Study eye characteristics: Time (wk) from diagnosis to inclusion | |||
| Mean ± SD a | 15.1 ± 8.8 | 17.9 ± 11.3 | 16.3 ± 9.9 |
| Median | 14 | 13 | 14 |
| BCVA (ETDRS letters ± SD) a | 46.2 ± 15.1 | 39.5 ± 21.2 | 44.2 ± 17.8 |
| Area of capillary nonperfusion on FFA (DA ± SD) a | 3.2 ± 3.3 | 3.0 ± 2.1 | 3.1 ± 2.8 |
| CFT (μm ± SD) a | 519.2 ± 183.7 | 615.6 ± 270.1 | 559.4 ± 225.4 |
| IOP (mm Hg ± SD) a | 14.1 ± 2.7 | 15.7 ± 2.9 | 14.8 ± 2.8 |
| Phakic eye, n (%) a | 17 (81.0%) | 13 (86.7) | 30 (83.3) |
a P value was nonsignificant between treatment and control groups for all parameters.
The completion rates through to 12 months in the study were 93.3% (14 of 15 patients) and 76.2% (16 of 21 patients) for the ranibizumab group and standard-of-care group, respectively. The 12-month outcome measure data were missing in a total of 6 patients. One patient from the ranibizumab group withdrew after being diagnosed with metastatic pancreatic carcinoma during the course of the study. Five patients did not complete the study in the standard-of-care group; among these, 2 patients were lost to follow-up, 2 patients decided to discontinue their participation, and 1 patient died of an unrelated cause. The last properly performed observation was carried forward for these missing values.
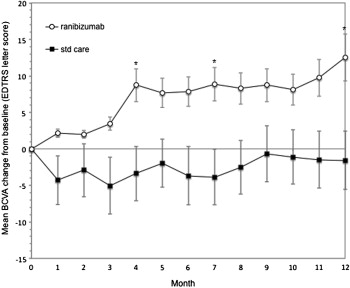
Primary Outcome Measure and Change From Baseline Best-Corrected Visual Acuity
The primary efficacy endpoint was mean change from baseline BCVA at 12 months. At 12 months, there was an improvement of visual acuity compared with baseline in the ranibizumab group by a mean of 12.5 letters (95% CI 2.8, 22.3) letters, while in the standard-of-care group there was a mean loss of 1.6 letters (95% CI -9.3, 6.2), a difference that was statistically significant ( P = .032); ( Table 3 , Figure 2 ). The improvement in BCVA in the ranibizumab group was seen at 1 month following injection and increased steadily at all subsequent monthly assessments up to the 12-month endpoint. In the standard-of-care group, a decrease in BCVA was seen at each time point from baseline, with a maximum loss of 5 letters at 3 months and fewer letters lost in the subsequent months. The difference in BCVA between the 2 groups was statistically significant at 12 months ( P = .032; Figure 2 ). Analysis by subgroup showed that statistically significant differences in the mean BCVA change between the 2 treatment groups were maintained in patients with poorer baseline vision, those with a longer duration of BRVO, and patients with thicker CFT at baseline ( Table 4 ). In both the ranibizumab and standard-of-care groups, the mean BCVA gain at 12 months was greater in patients with worse baseline BCVA and in patients who were diagnosed with BRVO for a longer duration of 12 weeks or more prior to inclusion into the study. Among patients who received ranibizumab, the mean improvement in BCVA at 12 months was greater in those who had CFT ≥450 μm at baseline. This was in contrast to the standard-of-care group, where patients with CFT with ≥450 μm did worse than those with CFT <450 μm at baseline.
| Parameter | Grid Laser (n = 21) | Ranibizumab (n = 15) | P Value |
|---|---|---|---|
| Change from baseline BCVA at 12 months in ETDRS letter score: | |||
| Mean ± SD | −1.6 ± 18.2 | 12.5 ± 19.3 | |
| 95% CI for mean | (−9.3, 6.2) | (2.8, 22.3) | |
| Difference in means (ranibizumab vs laser) | 14.1 | .032 | |
| 95% CI for difference | (1.09, 27.1) | ||
| Distribution of BCVA change at 12 months, n (%) | .116 a | ||
| Gain of ≥15 letters b | 4 (19.0) | 8 (53.0) | |
| Gain of 10-14 letters | 3 (14.3) | 1 (6.7) | |
| Gain of 5-9 letters | 0 (0.0) | 1 (6.7) | |
| No change, ± 4 letters | 6 (28.6) | 2 (13.3) | |
| Loss of 5-9 letters | 2 (9.5) | 0 (0.0) | |
| Loss of 10-14 letters | 0 (0) | 2 (13.3) | |
| Loss of ≥15 letters c | 6 (28.6) | 1 (6.7) | |
| Snellen equivalent BCVA ≥ 20/40, n (%) | 6 (28.6) | 9 (60.0) | .090 d |
| Snellen equivalent BCVA ≤ 20/200, n (%) | 1 (4.8) | 0 (0.0) | .999 d |
a P trend from Cochran-Armitage test for linear trend.
b P from 1-sided Fisher exact test of greater proportion of subjects with ≥15 letters gained in ranibizumab than in grid laser group = .037; P from 2-sided Fisher exact test = .071.
c P from 2-sided Fisher exact test of greater proportion of subjects with ≥15 letters lost in grid laser than in ranibizumab group = .200.
| Subgroup | Mean BCVA Change (95% CI) | Gained ≥15 Letters, n (%) | ||
|---|---|---|---|---|
| Grid Laser | Ranibizumab | Grid Laser | Ranibizumab | |
| Baseline BCVA (ETDRS letters) | ||||
| <55 | 7.4 (−4.5 to 19.2) | 27.9 (19.9 to 35.8) a | 1 (20.0) | 6 (85.7) |
| ≥55 | −4.4 (−13.6 to 4.9) | −0.9 (−10.8 to 9.0) | 4 (25.0) | 2 (25.0) |
| Time from diagnosis to inclusion (wk) | ||||
| <12 | −2.4 (−17.3 to 12.6) | 10.2 (−8.2 to 28.5) | 3 (37.5) | 3 (50.0) |
| ≥12 | 8.9 (−0.2 to 18.0) | 14.11 (2.49 to 25.7) a | 2 (15.4) | 5 (55.6) |
| Baseline CFT, μm | ||||
| <450 | 2.7 (−11.6 to 17.0) | 7.0 (−8.5 to 22.5) | 3 (42.9) | 2 (50.0) |
| ≥450 | −3.7 (−13.1 to 5.7) | 14.6 (2.3 to 26.8) a | 2 (14.3) | 6 (54.5) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


