HISTORY OF RADIAL AND ASTIGMATIC KERATOTOMY
During the 19th century, Snellen (1869) (
1), Schiötz (1885) (
2), Bates (1894) (
3), and Lans (1898) (
4) described methods to reduce astigmatism. In 1939, Sato (
5) described spontaneous breaks in Descemet’s membrane in keratoconus that caused flattening of the cornea and reduction of myopia. In 1953, Sato and colleagues (
6) suggested that by making radial incisions in the posterior as well as the anterior cornea, astigmatism and myopia could be treated. Sato’s surgical technique required entry into the anterior chamber at three to four different sites. Incisions were then made using a “free hand” technique through the endothelial surface, from the edge of a 6-mm central optical zone through 50% of the corneal thickness. Additional anterior incisions, placed in between the posterior ones, were then made at approximately the same depth. There is no indication that pachymetry was performed. Yamaguchi and associates (
7) have estimated that 40% to 50% of the endothelial surface was damaged at the time of surgery. Approximately 75% to 80% of the 200 patients who underwent Sato’s procedure developed visually significant corneal edema an average of 20 years after the operation.
In the early 1970s, in the former Soviet Union, Yenaliev (
8), Fyodorov, Agranorsky, and Durnev (
8,
9,
10,
11) modified Sato’s technique, performing anterior radial incisions in the peripheral cornea and sclera. In 1978, Bores, Myers, and Cowden (
12,
13) reported the outcomes of the first RK procedure in the United States, using Fyodorov’s techniques (
8,
10).
In 1980, the National Eye Institute funded the Prospective Evaluation of Radial Keratotomy (PERK) Study to assess the efficacy, safety, predictability, and stability of RK (
14). The PERK study used rigid, standardized, surgical protocols, data collection by independent observers, and a multicenter design. It was a collaborative effort among university-based and private ophthalmologists in nine clinical centers. The protocol did not allow corrections for astigmatism. The surgical plan was based on the amount of myopic error and no other preoperative factors such as age, sex, or intraocular pressure were addressed (
14,
15,
16).
The surgical protocol of the PERK Study required eight freehand centrifugal incisions (clear zone to limbus) made with the length of a 45-degree diamond blade set using ultrasonic pachymetry at 100% of the thinnest paracentral corneal measurement (
16). Preoperatively, optical zones were limited to 3, 3.5, or 4 mm, corresponding to low-, medium-, or high-myopia levels (range −2 to −8 D). Repeat surgery for enhancement (eight additional incisions were made between the initial eight) was carried out under specific guidelines (
15,
17).
The RK postoperative outcome in the PERK study showed a decrease in myopia in all patients: 88% of patients achieved uncorrected visual acuity of 20/40 or better; 90% of patients with myopia of 6 D or less achieved visual acuity of 20/40 or better. Reduction of best-corrected visual acuity (20/25) was noted in 0.8% of patients.
Throughout the decade following the initiation of the PERK study, numerous advances were introduced through the work of various surgeons (
Table 70-1) (
18,
19,
20,
21,
22,
23,
24,
25,
26). Two principal techniques for RK evolved: (a) American style (centrifugal), or backcutting, in which incisions are made from center to periphery; and (b) Russian style (centripetal), or frontcutting, in which incisions are made from the limbus to the edge of the desired optical zone. It has been shown that centrifugal incisions inherently yield a diminished range of corneal flattening, because incision depth for a given diamond setting is less reliable than that with a centripetal incision (
27,
28,
29).
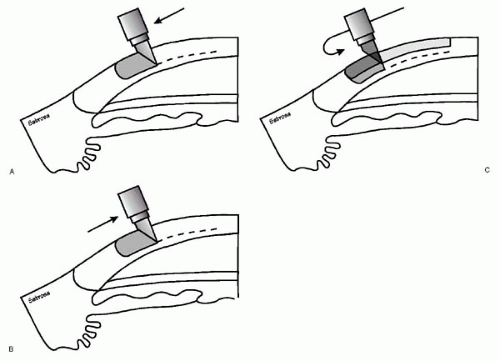
From these two approaches evolved the Genesis and Duotrack (or “combined”) techniques, which combined the safety of the centrifugal incision with the efficacy of the centripetal incision (
24,
30). In the combined technique, the centrifugal component provided the surgeon with a relatively shallow and linear safety groove. The centripetal component further deepened the incision groove and undercut the deep stroma adjacent to the optical zone, increasing the range of corneal flattening (
Fig. 70-1) (
30,
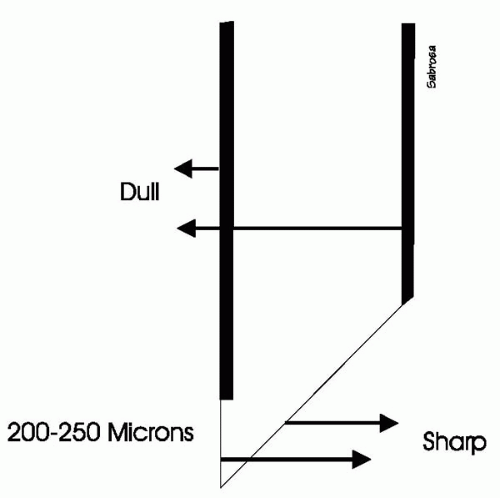
31). The diamond knife blade employed for the combined technique enabled the surgeon to begin the incision at the optical (clear) zone, extend out toward the limbus, and then reverse direction back toward the central optical zone without optical zone invasion. The angled edge on the back surface (centrifugal cutting component) is sharpened along the entire length, and the vertical edge of the front surface is ground sharp to a cutting edge for a distance of only 200 to 250
μm from the blade tip (
Fig. 70-2). The blunt upper portion of the vertical knife edge reduced the chance of unwanted invasion of the central optical zone when the blade tip is initially inserted into the cornea at the optical zone margin (
32). In a comparative study using donor eyes (
31), the combined (Genesis) technique demonstrated greater corneal flattening than the centrifugal (American) method of incision and reduced variability when compared with the centripetal (Russian) method.
As experience with RK increased, a tendency for shorter incisions developed (
26,
33,
34,
35,
36). In a cadaver eye study, Jester and associates (
34) found that incisions extending beyond the limbus reduced the efficacy of RK. Salz and colleagues (
35) found a small decrease in efficacy when using a shorter incision, but a significant effect was maintained. This is consistent with the results from Lindstrom’s (
26) modified technique for low to moderate myopes, known as
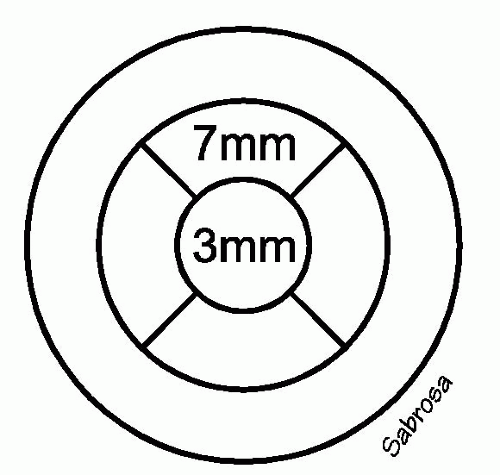
minimally invasive RK (“mini-RK”), which reduces the length of cornea incised. In a cadaver eye study, eight short incisions were performed from the 3-mm to the 7-mm optical zone (
Fig. 70-3), producing 92% of the efficacy of full-length incisions made to the 11-mm optical zone. Pinheiro and co-workers’ (
36) eye bank study also showed that reducing the incision length reduced the likelihood of corneal rupture as intraocular pressure is increased.
PATIENT EVALUATION
Approximately 25% of the adult population in the United States is myopic (
37,
38). It has been reported that the majority of candidates seeking keratorefractive surgery state their goal as good visual function without physical dependence on spectacles or contact lenses (
39,
40). Occasionally, patients may have medical (e.g., contact lens intolerance),
occupational, recreational, or cosmetic reasons for seeking surgery.
RK should be limited to patients with low to moderate myopia and an otherwise normal eye examination (
24,
41,
42). Higher degrees of myopia have variable responses to RK, and procedures such as photorefractive keratectomy and laser-
in-situ keratomileusis (LASIK) may yield better and more stable results. For extreme high myopes, clear lens extraction or phakic intraocular lens implantation may be more appropriate. In the case of the RK candidate, myopia, and astigmatism must be stable and nonprogressive (
43). Postoperative corneal transplant and cataract surgery patients with residual myopic astigmatism may benefit from incisional keratotomy after all sutures are completely removed and refractive stability documented.
Table 70-2 outlines the appropriate surgical procedures for the levels of severity of ametropia.
Patient History
A complete patient history should be taken, including a medical and ocular history, a family history, a list of medications, the refractive stability, as well as a relevant social and occupational history.
Scleritis: A history of scleritis disqualifies patients from all keratorefractive surgeries because of the potential for associated systemic disease, corneal melting, and perforation.
Delayed epithelial wound healing: Patients considered ineligible for RK because of delayed epithelial wound healing are those with a history of neurotrophic corneal ulcers, herpes zoster ophthalmicus, or nonhealing epithelial defects.
Corneal ectasias: Corneal ectasias such as keratoconus are absolute contraindications to incisional keratotomy (
44,
45,
46). Keratoconus is a progressive corneal ectasia that can cause wide variations and fluctuations in pre- and postoperative refractions (
46,
47,
48,
49). Refractive surgery may accelerate the progression of this disease. Other corneal ectasias include keratoglobus, Terrien’s, and pellucid marginal degeneration.
Cataracts: Cataracts are an absolute contraindication to RK surgery, as refractive shifts and loss of best-corrected visual acuity frequently occur as a result of progression. However, patients with stable, visually insignificant congenital lens opacities are reasonable candidates for keratorefractive surgery.
Retinal diseases: Retinal diseases such as macular degeneration, diabetic retinopathy or other vasculopathy, and progressive retinal degenerations are absolute contraindications, because of the potential for loss of low-contrast acuity, which may accelerate loss of best-corrected acuity in these patients.
Connective tissue disease: Connective tissue diseases, including rheumatoid arthritis and Sjögren’s syndrome, affect corneal wound healing and therefore are contraindications for RK. Patients with history of inflammatory bowel diseases (e.g., Crohn’s disease, ulcerative colitis, or Wegener’s granulomatosis) have the potential for corneal melting and are poor candidates for this surgery.
Immunosuppression: Patients with history of immunosuppression due to acquired immunodeficiency syndrome or chronic active hepatitis, as well as those who are pharmacologically immunosuppressed from systemic
corticosteroids or other cytotoxic agents are poor candidates for refractive surgery.
Pregnancy: Pregnancy is an absolute contraindication to RK because of the changes in corneal curvature and refraction that can occur during this time. Incisional keratotomy should be delayed until stability of refraction is documented after delivery. The effects of RK in nursing mothers have not been well documented, but in general it is advisable to defer surgery until lactation has ceased and a stable refractive state documented.
Relative Contraindications
Keratoconjunctivitis sicca: Keratoconjunctivitis sicca resulting from Sjögren’s syndrome, alkali burns, or ocular cicatricial pemphigoid is an absolute contraindication, but moderate to severe primary dry-eye syndromes resulting in surface abnormalities are considered relative contraindications to keratorefractive surgery. These patients should be treated with punctal occlusion and tear replacement before surgery to normalize the ocular surface. If a normal ocular surface cannot be achieved with such interventions, it is best to avoid surgery.
Herpes simplex keratitis: In general, refractive surgery in patients with a documented history of ocular herpes simplex keratitis should be approached with extreme caution. Patients without a history of stromal disease who have been free from herpes simplex keratitis for at least 1 year may be reasonable surgical candidates, particularly if corneal sensation is normal, but it should be considered that they may be at reserved risk for herpes simplex-related ocular morbidity if they undergo surgery. Oral acyclovir given in the perioperative period may also be beneficial in preventing recurrence of the disease (
50).
Blepharitis, ocular rosacea, and meibomitis: These conditions can also be relative contraindications to refractive surgery and need to be treated preoperatively with lid hygiene, and in some cases with oral tetracycline, doxycycline, or minocycline. Moreover, medical treatment of these disorders must be continued after surgery to minimize the chances of abnormal corneal wound healing. In the presence of corneal pannus, RK should be deferred until the underlying cause is controlled, because these eyes are at higher risk of developing vascularization within the incisions, resulting in subsequent refractive instability.
Glaucoma: A history of glaucoma is a relative contraindication to incisional keratotomy. The use of topical steroids in the postoperative period of incisional keratotomy may increase the intraocular pressure, and fluctuations in intraocular pressure may affect the refractive state of the eye as well.
Diabetes mellitus: Diabetes mellitus is a relative contraindication. This is due to concerns about delayed wound healing and abnormal immune responses, although there have been no specific complications reported in diabetic patients undergoing RK. Certainly a diabetic patient with documented ocular complications of diabetes is not a good candidate for refractive surgery.
Atopic disease: Atopic patients with severe lid abnormalities, cataracts, keratoconus, or severe eye rubbing are poor candidates for surgery. Eye rubbing can lead to an increased incidence of infection, a delay in wound healing, and postoperative refractive instability. Antihistamines and behavior modification may be beneficial in preventing and treating ocular itching and eye rubbing, respectively.
Family History
The family history should include documentation of corneal dystrophies, keratoconus, glaucoma, retinal detachment, retinal dystrophies, optic nerve abnormalities, diabetes mellitus, collagen vascular disease, early cardiovascular disease, and any other hereditary diseases.
Medications
A complete list of past and current systemic and ophthalmic medications should be obtained from the patient. This list can provide clues to the existence of diseases that may have been overlooked or forgotten by patients during the medical and ocular history.
Refractive Stability
Patients younger than 18 and those who have had a 0.5 D or greater change in sphere or cylinder per year over the preceding 2 years are not eligible for surgery. In general,
waiting until at least 21 years of age before attempting refractive surgery is preferable.
Contact Lens Wear Considerations
Candidates for keratorefractive surgery should discontinue soft contact lens wear 2 weeks before surgical evaluation. Rigid, gas-permeable lens wearers must discontinue lenses for a minimum of 3 weeks before surgical evaluation. Manifest and cycloplegic refractions, along with corneal topography, should be used to monitor and confirm stabilization of the corneal curvature of refraction before the surgery can be planned. The existence of corneal warping due to contact lens wear (usually rigid, gas permeable lenses) is a contraindication to keratorefractive surgery until the condition has stabilized. It may take months or years for some corneas to recover from warping due to contact lens wear (
51). If corneal topography or refraction is unstable at the time of evaluation, repeat testing after 2 to 3 weeks is usually performed.
Social and Occupational History
Patients of presbyopic age may benefit from refractive correction of monovision, whereas younger patients (35 to 40 years of age or younger) are usually not tolerant of this approach. Patients involved in contact sports clearly should not be considered good candidates for RK. When applicable, patients should be made aware that some airlines and branches of the military do not recognize refractive surgery as a valid means of visual correction.
Patient Expectations
Patients with unrealistic expectations for surgical outcomes, such as those who expect an improvement in best-corrected acuity or better vision than that achievable with corrective contact lenses, should be considered poor candidates for refractive surgery unless properly educated about realistic expectations of RK.
Patient Evaluation
A complete ophthalmologic examination is performed, including measurements of ocular dominance and motility, pupil size (in light and dim illumination), corneal sensitivity, and intraocular pressure. Examination procedures should include retinoscopy, manifest and cycloplegic refractions as well as external slit-lamp and dilated funduscopic examinations. Funduscopic examination should include posterior pole examination for the presence of myopic degeneration and examination of the periphery to check for presence of lattice degeneration or evidence of other myopic vitreoretinal abnormality.
Preoperative testing usually includes corneal topography and screening pachymetry. For corneal topography, computed videokeratography (CVK) can be used to detect regular and irregular astigmatism, corneal warping from contact lens wear, or compressive lid lesions, as well as evidence of keratoconus (
44,
45,
52,
53,
54,
55), or pellucid marginal degeneration. For astigmatic keratotomy (AK), topography helps to refine placement of arcuate or tangential incision or incisions, although it should be kept in mind that the correlation between refractive and topographic astigmatism is sometimes poor (
56).
Patient Education
It is crucial that the prospective patient demonstrate reasonable comprehension of the potential risks and benefits of the primary surgery and possible enhancement procedures as well as reasonable surgical and nonsurgical alternatives. It should be stressed that additional corrective optical aids (i.e., glasses or contact lenses) may still be necessary to improve vision postoperatively. Changes in corneal shape may, in some cases, make contact lens wear more difficult or impossible. Furthermore, it should be stressed that corneal surgery will not change the normal aging process of the crystalline lens, whereby most individuals at or near emmetropia require reading glasses by their mid-40s.
Preoperatively the patient must read and sign an informed consent document after discussing the planned procedure and the postoperative instructions with the keratorefractive surgeon. It is preferable to conduct the informed consent discussion at a visit separate from the day of surgery. This allows the patient time to digest the information received and ask further questions, if necessary.