Atopic Conjunctivitis
Neal P. Barney
Atopy refers to hypersensitivities in persons with a hereditary background of allergic diseases as first described by Cocoa and Cooke (1). The major, most commonly recognized atopic conditions include eczema (atopic dermatitis), asthma, hay fever, and allergic rhinitis. Atopic conditions affect 10% to 20% of the population. Atopic ocular disease includes seasonal allergic conjunctivitis (SAC), perennial allergic conjunctivitis (PAC), vernal keratoconjunctivitis (VKC), atopic keratoconjunctivitis (AKC), and giant papillary conjunctivitis (GPC). VKC and AKC may cause significant complications and lead to loss of vision. Type I hypersensitivity reaction of the ocular surface is the putative mechanism in SAC and PAC but is not the only pathophysiologic mechanism in VKC and AKC.
ALLERGIC CONJUNCTIVITIS: SEASONAL/PERENNIAL
Allergic conjunctivitis (AC) is a bilateral, self-limiting, allergic conjunctival inflammation. It occurs in sensitized individuals (no gender difference) and is initiated by allergen binding to immunoglobulin E (IgE) antibody on resident mucosal mast cells. Its importance is related more to its frequency than to its severity. The two forms of AC are defined by whether the inflammation occurs seasonally (spring, fall, SAC) or perennially (year-round, PAC). The inflammatory symptoms are similar for both entities; seasonal allergic conjunctivitis (“hay fever conjunctivitis”) is more common. SAC accounts for the majority of cases of AC and is related to atmospheric pollens (e.g., grass, trees, ragweed) that appear during specific seasons. Perennial allergic conjunctivitis is often related to animal dander, dust mites, or other allergens that are present in the environment year-round. Both SAC and PAC must be differentiated from the sight-threatening allergic diseases of the eye, AKC and VKC.
Demographics
Prevalence estimates for allergic conjunctivitis are difficult because allergies in general tend to be considerably underreported. A survey conducted by the American College of Allergy, Asthma, and Immunology (ACAAI) found that 35% of families interviewed experience allergies. Of these, at least 50% report associated eye symptoms. Most reports agree that allergic conjunctivitis affects up to 20% of the population, i.e., 60 million individuals in the United States (2). Importantly, 60% of all allergic rhinitis sufferers have associated allergic conjunctivitis. The distribution of SAC depends largely on the climate. For example, in the United States grass pollen—induced SAC generally occurs in the Gulf Coast and southwestern areas of the country from March to October, and from May to August in most of the rest of the country. Conversely, ragweed pollen—induced SAC occurs in most of the country during August through October, but in the southernmost states it can begin as early as July and stretch out through November. Tree pollens can become a problem as early as January in the south, and March in the north.
Symptoms
The dominant symptom reported in allergic conjunctivitis is ocular itching. Itching can range from mild to severe. Other symptoms include tearing (watery discharge), redness, swelling, burning, a sensation of fullness in the eyes or eyelids, an urge to rub the eyes, sensitivity to light, and occasionally blurred vision. As stated previously, allergic conjunctivitis is often associated with symptoms of allergic rhinitis.
Signs
Mild conjunctival hyperemia and chemosis are typical signs seen in patients with SAC. Hyperemia is the result of vascular dilatation; chemosis occurs because of altered permeability of postcapillary venules (Fig. 19-1). “Allergic shiners” (periorbital darkening), due to a transient increase of periorbital pigmentation resulting from the decreased venous return in the skin and subcutaneous tissue, are also common.
Pathophysiology
It has been understood for some time that antigen cross-linking of IgE antibody bound to the high-affinity IgE
receptor (FcεRI) on mast cells induces release of both preformed (granule associated, e.g., histamine and tryptase) and newly synthesized mediators (e.g., arachidonic acid metabolites), which have diverse and overlapping biologic effects. Both tissue staining and tear film data have implicated the mast cell and IgE-mediated release of its mediators in the pathophysiology of the ocular allergic inflammatory response. Additionally, a number of clinical studies examining topical antihistamine, mast cell stabilizing, and dual-acting drugs have demonstrated relief of allergic conjunctivitis symptoms (see Treatment, below).
receptor (FcεRI) on mast cells induces release of both preformed (granule associated, e.g., histamine and tryptase) and newly synthesized mediators (e.g., arachidonic acid metabolites), which have diverse and overlapping biologic effects. Both tissue staining and tear film data have implicated the mast cell and IgE-mediated release of its mediators in the pathophysiology of the ocular allergic inflammatory response. Additionally, a number of clinical studies examining topical antihistamine, mast cell stabilizing, and dual-acting drugs have demonstrated relief of allergic conjunctivitis symptoms (see Treatment, below).
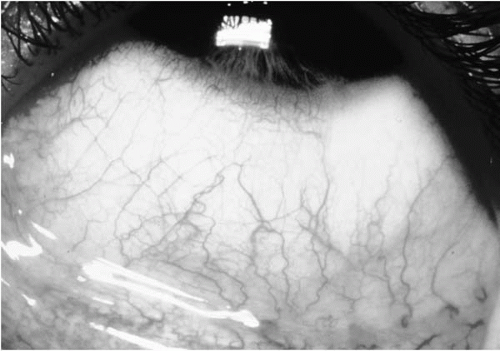 FIGURE 19-1. Seasonal allergic conjunctivitis showing chemosis and hyperemia.(see color image) |
Synthesis of inflammatory mediators varies according to the phenotype and tissue location of the mast cell. Granule-associated neutral proteases (tryptase and chymase) unique to mast cells are generally accepted as the most appropriate phenotypic markers to categorize human mast cells into subsets. Mast cells on this basis have been divided into MCT (tryptase) and MCTC (tryptase/chymase) phenotypes. The phenotype of normal human conjunctival mast cells has been well-documented using immunostaining of conjunctival biopsy specimens. Mast cells are rarely present in the normal human conjunctival epithelium, but when they are found, they appear to be limited to the MCT phenotype. Mast cells (MCT phenotype) and eosinophils are found to be increased in the conjunctival epithelium of individuals with SAC and PAC. In the substantia propria of the normal human conjunctiva, 95% are of the MCTC phenotype (3, 4, 5). The total number of mast cells (MCTC phenotype) is also increased in the substantia propria of individuals with AC (3).
Clinical evidence for mast cell activation is found in SAC and PAC. Tear film analysis of patients consistently reveals the presence of IgE antibody, histamine (6), and tryptase (7). There are granule associated, preformed (histamine, tryptase, bradykinin) and arachidonic acid derived, newly formed (leukotrienes, prostaglandins) mediators present in patients with ocular allergy. Preformed mediators are released immediately upon allergen exposure, whereas roughly 8 to 24 hours are required for release of newly formed mediators. These mediators are known to have overlapping biologic effects that contribute to the characteristic ocular itching, redness, and watery discharge associated with allergic eye disease. Histamine is involved in the regulation of vascular permeability, smooth muscle contraction, mucus secretion, inflammatory cell migration, cellular activation, and modulation of T-cell function (8). Arachidonic acid metabolites and tryptase originating from mast cells also have been shown to be specifically involved in the regulation of many of these same processes. Mast cells also synthesize cytokines and chemokines. Less well documented and defined are the effects of these mediators in the ocular allergic inflammatory process. Cytokines stored in mast cells are likely the first signals initiating infiltration of inflammatory white blood cells, such as eosinophils. Once these cells arrive, they gain access to the conjunctival surface by moving through the already dilated capillaries.
Immunohistochemical staining of human conjunctival tissue biopsies shows that inflammatory cytokines interleukin-4 (IL-4), IL-5, IL-6, and tumor necrosis factor-α (TNF-α) are localized to mast cells in normal and allergic conjunctivitis (9). These cytokines are consistent with a T-helper-2 (Th2) cytokine profile. Inflammatory cytokines (e.g., TNF-α) have also been measured in human tears (10, 11, 12, 13). Although it is difficult in vivo to determine the cellular source of cytokines in tears, recent studies comparing allergic to nonallergic subjects indicate that cytokine levels may be important indicators of ocular allergy (14). It has been demonstrated that tears from allergic donors (when compared to nonallergic donors) contained significantly less of the antiinflammatory cytokine, IL-10, and a trend toward decreased levels of the Th1 cytokine, interferon-γ (IFN-γ)-(14). Finally, IgE-mediated release of histamine and cytokines from mast cells can also initiate secondary effects on conjunctival epithelial cells. The activation and participation of epithelial cells in allergic inflammation is an active field of research. Human conjunctival epithelial cells express H1 receptors coupled to phosphatidylinositol turnover and calcium mobilization (15). Cytokines released from mast cells upregulate intercellular adhesion molecule 1 (ICAM-1) expression on conjunctival epithelial cells (16). This has become a hallmark of allergic inflammation. ICAM-1 appears to play a critical role in the migration of inflammatory cells, and is rapidly expressed following ocular allergen provocation.
Diagnosis
An individual suspected of having allergic conjunctivitis should have a thorough ocular, medical, and medication history. This will help greatly in differentiating AC from other ocular processes. This history should establish whether the process is acute, subacute, chronic, or recurrent. It should
further delineate whether the symptoms and signs are unilateral or bilateral, and whether they are associated with any specific environmental or work-related exposure. Ocular symptoms such as tearing, irritation, stinging, and burning are nonspecific. A history of significant ocular itching and a personal or family history of hay fever, allergic rhinitis, asthma, or atopic dermatitis are suggestive of ocular allergy. Viral and bacterial infections of the eye may mimic allergic conjunctivitis. Because AC is secondary to environmental allergens as opposed to transmission by eye-hand contact (infectious etiology), SAC and PAC usually present with bilateral symptoms. Patients complain of watery discharge or increased tearing. Redness is mild and chemosis may be present. Symptoms are often greater than signs. Vision, pupil shape, ocular movement, light reactivity, and the red retinal reflex remain normal in allergic conjunctivitis. Dry eye (secondary to a decrease of the aqueous portion of the tear film) gives symptoms suggestive of foreign body in the eye and may result in conjunctival redness. Similar symptoms are possible from anticholinergic side effects of systemic medications. Typically, itch is not reported with dry eye. Medication history should include questions concerning the patient’s use of over-the-counter topical ocular medications, cosmetics, contact lenses, and systemic medications. Any of these can produce acute or chronic conjunctivitis. This inquiry should include direct questions and should not rely on the patient to volunteer information. Many individuals do not appreciate the potential for nonprescription topical ocular medications to cause eye symptoms or partially treat AC.
further delineate whether the symptoms and signs are unilateral or bilateral, and whether they are associated with any specific environmental or work-related exposure. Ocular symptoms such as tearing, irritation, stinging, and burning are nonspecific. A history of significant ocular itching and a personal or family history of hay fever, allergic rhinitis, asthma, or atopic dermatitis are suggestive of ocular allergy. Viral and bacterial infections of the eye may mimic allergic conjunctivitis. Because AC is secondary to environmental allergens as opposed to transmission by eye-hand contact (infectious etiology), SAC and PAC usually present with bilateral symptoms. Patients complain of watery discharge or increased tearing. Redness is mild and chemosis may be present. Symptoms are often greater than signs. Vision, pupil shape, ocular movement, light reactivity, and the red retinal reflex remain normal in allergic conjunctivitis. Dry eye (secondary to a decrease of the aqueous portion of the tear film) gives symptoms suggestive of foreign body in the eye and may result in conjunctival redness. Similar symptoms are possible from anticholinergic side effects of systemic medications. Typically, itch is not reported with dry eye. Medication history should include questions concerning the patient’s use of over-the-counter topical ocular medications, cosmetics, contact lenses, and systemic medications. Any of these can produce acute or chronic conjunctivitis. This inquiry should include direct questions and should not rely on the patient to volunteer information. Many individuals do not appreciate the potential for nonprescription topical ocular medications to cause eye symptoms or partially treat AC.
Treatment
Allergic conjunctivitis can be debilitating to some degree and may cause some individuals affected to seek any type of help for relief of symptoms. The itching and tearing may be unbearable and sleepless nights frequent. Ocular allergic conjunctivitis symptoms may be worse than the nasal symptoms in those suffering from rhinoconjunctivitis. Furthermore, treatment of the nasal symptoms with topical nasal steroids may help the rhinitis, but not be effective for relieving ocular symptoms.
Management of allergic conjunctivitis, therefore, is primarily aimed at alleviating symptoms. Establishing the cause is the first step in treating allergic conjunctivitis. The best treatment is avoidance of the specific allergen, which, unfortunately, is sometimes not possible. But evaluation by an allergist, determination of sensitivities, and education about allergen avoidance through the use of filtering systems, barriers (bedding), special cleaning products, and vacuum sweepers can be of enormous help to the allergic patient. Avoidance of scratching or rubbing, application of cool compresses, artificial tears, and refrigeration of topical ocular medications are practical interventions to alleviate discomfort. Although oral antihistamines may help to relieve eye discomfort, this may also decrease tear production, causing more ocular symptoms.
The treatment of choice for mild to moderate AC is a dual-acting topical ocular medication (mast cell stabilizer and antihistamine effect: azelastine, ketotifen, or olopatadine). The mast cell stabilizing component of these drugs benefits patients most if treatment is started before the height of symptom onset. Patients usually note rapid onset of relief of itch upon drop instillation, as most dual-action medications have high H1 receptor affinity. Drug dosing varies from two to four times per day and efficacy is judged best by symptom relief.
In severe disease, combination therapy may be recommended. This therapy may include topical medications [antihistamines, mast cell stabilizers, nonsteroidal antiinflammatory drug (NSAIDs), or combinations], and oral antihistamines. NSAIDs inhibit cyclooxygenase, resulting in decreased formation of prostaglandins and thromboxanes, but not leukotrienes. Therefore, these compounds are useful in controlling itching and some inflammation, but not the infiltration of inflammatory cells. In extreme cases, use of a topical steroid four times a day should be considered. All patients receiving topical steroids should have their intraocular pressure measured frequently. Immunotherapy performed by an allergist may be beneficial in decreasing the severity of future ocular allergy symptoms.
VERNAL KERATOCONJUNCTIVITIS
Definition
VKC is a chronic, bilateral conjunctival inflammatory condition found in individuals predisposed by their atopic background. An excellent review of the history and description of this disease was published by Buckley (17) in 1988. Beigelman’s (18) 1950 monograph, Vernal Conjunctivitis, continues to be the most exhaustive compilation of information on this disease and is unmatched in current times. The list of easily recognized names in ophthalmology to have published on this entity is formidable: Arlt (19), Desmarres (20), von Graefe (21), Axenfeld (22), Trantas (23), and Herbert (24).
Demographics
In 2000, Bonini et al. (25) reviewed a series of 195 patients with VKC as the only allergic manifestation in 58.5% of patients. The onset of VKC generally occurs before age 10, it lasts 2 to 10 years, and it usually resolves during late puberty. Only 11% of patients were older than 20 years of age in the Bonini series (25). Males predominate in the younger ages, but the male-female distribution is nearly equal in the older patients. Young males in dry, hot climates are those primarily affected. The Mediterranean area and West Africa are areas of the greatest numbers of patients. It is relatively unusual in
most of North America and Western Europe. There is a significant history of other atopic manifestations such as eczema or asthma in 40% to 75% of patients with VKC (25). A family history of atopy is found in 40% to 60% of patients (25). Seasonal exacerbation, as the name implies, is common, but patients may have symptoms year-round.
most of North America and Western Europe. There is a significant history of other atopic manifestations such as eczema or asthma in 40% to 75% of patients with VKC (25). A family history of atopy is found in 40% to 60% of patients (25). Seasonal exacerbation, as the name implies, is common, but patients may have symptoms year-round.
Symptoms
Severe itching and photophobia are the main symptoms. Associated foreign-body sensation, ptosis, thick mucous discharge, and blepharospasm also occur.
Signs
The signs are confined mostly to the conjunctiva and cornea; the skin of the lids and lid margin are relatively uninvolved compared to AKC. The conjunctiva develops a papillary response, principally of the limbus or upper tarsus. The tarsal papillae are discrete, greater than 1 mm in diameter, have flattened tops that may stain with fluorescein, and occur more frequently in European and North American patients (17). Thick, ropy mucus tends to be associated with the tarsal papilla (Fig. 19-2). These are the classic “cobblestone papillae.”
Limbal papillae tend to be gelatinous and confluent, and they occur more commonly in African and West Indian patients (17) (Fig. 19-3). Horner-Trantas dots, which are collections of epithelial cells and eosinophils, may be found at any meridian around the limbus (22). These changes may lead to superficial corneal neovascularization. The forniceal conjunctiva usually does not show foreshortening or symblepharon formation.
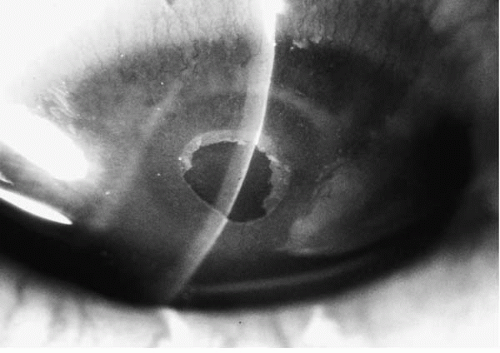
The corneal findings may be sight threatening. Buckley (17) describes in detail the sequence of occurrence of corneal pathogenesis. Mediators from the inflamed tarsal conjunctiva cause a punctate epithelial keratitis. Coalescence of these areas leads to frank epithelial erosion, leaving Bowman’s membrane intact. If, at this point, inadequate or no treatment is rendered, a plaque containing fibrin and mucus deposits over the epithelial defect (26). Epithelial healing is then impaired, and new vessel growth is encouraged. This so-called shield ulcer (Fig. 19-4) usually has its lower border in the upper half of the visual axis. With resolution, the ulcerated area leaves a subepithelial ringlike scar. The peripheral cornea may show a waxing and waning, superficial stromal, and gray-white deposition termed pseudogerontoxon. Iritis is not reported to occur in VKC.
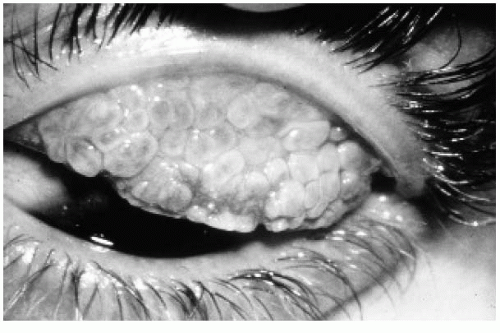 FIGURE 19-2. Flat-topped giant papillae of vernal keratoconjunctivitis (VKC).(see color image) |
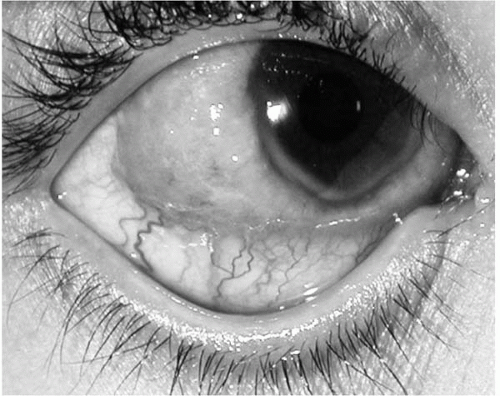 FIGURE 19-3. Limbal vernal lesion.(see color image) |
Pathophysiology
Biopsy of a tarsal conjunctival papilla in VKC reveals distinct findings. The epithelium contains large numbers of mast cells and eosinophils, neither of which are found in normal individuals (27,28). Human mast cells may be categorized based on the presence of neutral proteases (29). The epithelium of VKC patients contains mast cells predominantly of the type containing the neutral proteases tryptase and chymase (2). Basophils are found in the epithelium, which may indicate one form of a delayed type hypersensitivity reaction is occurring. Leonardi et al. (28) demonstrated eosinophils,
neutrophils, and mononuclear cells in the hyperplastic epithelium. Brush cytology of the conjunctival epithelium from patients with VKC showed more eosinophils and neutrophils in patients with corneal erosion or ulcer than in those without (30). Goblet cell density is not found to be elevated in the conjunctival epithelium of VKC (31). Eosinophil major basic protein is deposited diffusely throughout the conjunctiva of VKC patients, including the epithelium (32).
neutrophils, and mononuclear cells in the hyperplastic epithelium. Brush cytology of the conjunctival epithelium from patients with VKC showed more eosinophils and neutrophils in patients with corneal erosion or ulcer than in those without (30). Goblet cell density is not found to be elevated in the conjunctival epithelium of VKC (31). Eosinophil major basic protein is deposited diffusely throughout the conjunctiva of VKC patients, including the epithelium (32).
TABLE 19-1. COMPARISON OF VERNAL KERATOCONJUNCTIVITIS (VKC) AND ATOPIC KERATOCONJUNCTIVITIS (AKC) | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
The substantia propria contains elevated numbers of mast cells compared to normal individuals (27,28). The predominant mast cell subtype found contains tryptase and chymase (2). Forty-six percent of the mast cells in the substantia propria contain basic fibroblast growth factor (bFGF) (33). This may serve as a source of fibroblast growth and production of collagens. Eosinophil major basic protein granules are found close to mast cells in VKC (32). As in the epithelium, the substantia propria contains increased numbers of eosinophils and basophils compared to normal tissue (27). A unique profile of lymphocytes is found. T-cell clones can be isolated from biopsy specimens of VKC tarsal conjunctiva. These CD4 T-cell clones show helper function for IgE synthesis in vitro and produce IL-4 (34). Calder et al. (35), in separate work, found IL-5 expressed in T-cell lines from vernal biopsy specimen. Cognate interaction with T cells and the presence of IL-4 are needed for B-cell production of IgE (34). This would support the suggestion that IgE is produced locally. The substantia propria also has an increased amount of collagen. Fibroblasts from the tarsal conjunctival biopsy of VKC patients can be induced to proliferate by histamine and epithelium-derived growth factor (28). Cyclosporin A, which can be used effectively in VKC, has been shown in vitro to reduce collagen production and induce apoptosis of conjunctival fibroblasts from VKC patients (36).
The corneal epithelium of VKC patients expresses ICAM-1, an important cell adhesion molecule (37). Eosinophil peroxidase in contact with human corneal epithelial cells causes disruption of cell adhesion (38). Eosinophil major basic protein (EMBP) and cationic protein (ECP) are proinflammatory, and EMBP has been shown to be cytotoxic to corneal epithelium. In vitro, both of these damage the monolayers of human corneal epithelial cells but not the stratified corneal epithelial cells in culture (39).
Specific IgE and IgG have been isolated from the tears of VKC patients (40,41). Histamine (6) and tryptase (7) are elevated in the tears of VKC patients. The serum of VKC patients has been found to contain decreased levels of histaminase and increased levels of nerve growth factor (42,43). Finally, VKC is reported to occur in patients with the hyperimmunoglobulin E syndrome (44).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree