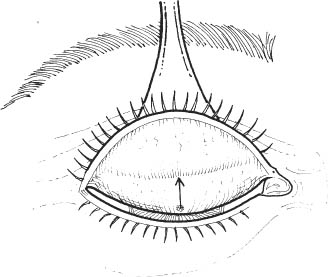
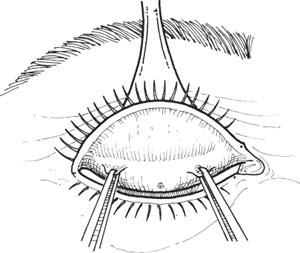
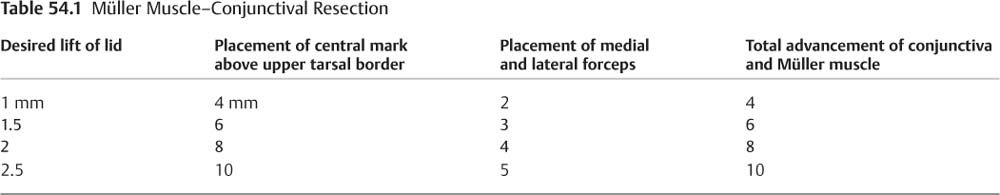
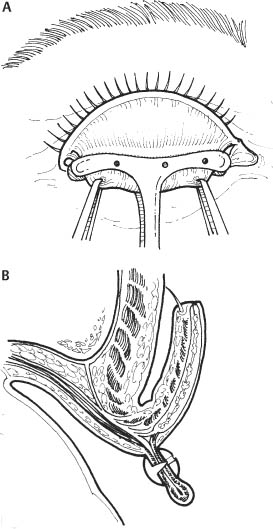
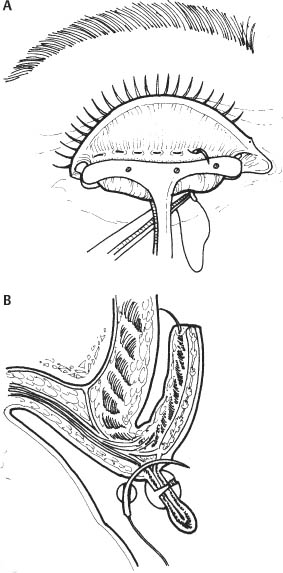
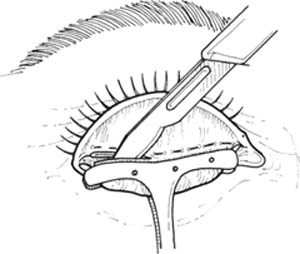
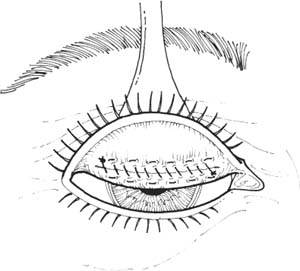
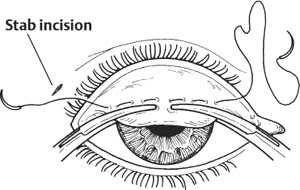
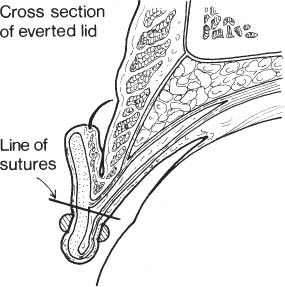
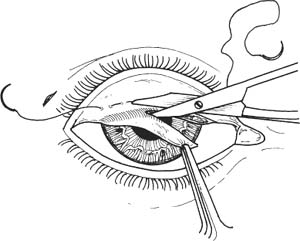
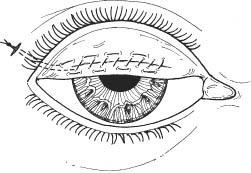
54 Numerous approaches to ptosis surgery have been described. The optimal procedure is determined by the etiology, severity, and characteristics of the ptotic eyelids and the personal preference of the surgeon. Ptosis may be broadly classified: Treatment based on the specific etiology will give the best results. Obtain a complete history to appropriately classify ptosis. The type and severity of ptosis will dictate the appropriate surgical management. Perform a complete lid and eye examination to determine a detailed operative plan. Evaluation of levator function and magnitude of ptosis are the most important determinants of the type of surgery to be performed. 1. Evaluate lid position and levator function. a. Measure palpebral fissure width. b. Ascertain amount of ptosis by measuring the margin to pupillary reflex distance (MRD) (the distance from the upper eyelid margin to the pupillary light reflex). i. Mild ptosis: 1–2 mm of lid droop (MRD = 2–3 mm) ii. Moderate ptosis: 3 mm of lid droop (MRD = 1 mm) iii. Severe ptosis: 4 mm or more (lid margin at or below visual axis) c. Measure levator function. i. Good: More than 8 mm. ii. Fair: 5–7 mm. iii. Poor: 4 mm or less. d. Note lid position on downgaze. i. Congenital ptosis is associated with lid lag. ii. In acquired ptosis, lid remains ptotic on downgaze. e. Compare lid symmetry. 2. Measure position of lid crease. a. A high lid crease suggests disinsertion or dehiscence of the levator aponeurosis. 3. Check corneal sensation, Bell phenomenon, and Schirmer test to evaluate potential impact of any postoperative lagophthalmos. 4. Perform an external examination with eversion of the upper eyelids to look for eyelid or orbital masses. a. Pseudoptosis is a consideration (from enophthalmos of involved eye, or proptosis of contralateral eye. 5. Perform neuromuscular examination. a. Examine pupils to rule out Horner syndrome or third nerve palsy. b. Check extraocular muscle function to rule out third nerve palsy or lack of Bell phenomenon. c. Rule out hypotropia as cause of pseudoptosis. d. Rule out myasthenia gravis. 6. Perform a visual field examination to document any field cut secondary to ptosis. 7. Take straight-on photographs to document presurgical presence of ptosis. The posterior Müller muscle–conjunctival resection procedure is useful for mild ptosis (less than 3.0 mm lid droop) with good levator function (8 mm or more). It gives excellent symmetry and contour when performed bilaterally. See Chapter 3. 1. Discontinue aspirin and nonsteroidal anti-inflammatory agents for 10 days before surgery. Discontinue warfarin 2–3 days preoperatively, if medically possible. 2. Query patient about bleeding tendencies. A useful screening question is asking if the patient had unusual bleeding after dental extraction. Obtain hematological evaluation if bleeding tendency is suspected. 1. Apply topical anesthetic. 2. Anesthesia: Local infiltrative anesthetic or general anesthetic in children and uncooperative patient. a. Inject 2.5 ml of 2% lidocaine without epinephrine in the frontal nerve distribution and pretarsal area b. Avoid epinephrine since it stimulates the Müller muscle and may influence results of surgery. 3. Prep and drape in the usual sterile manner. a. Keep both eyes exposed for comparison of two eyes during procedure. Figure 54.1 4. Evert eyelid over Desmarres retractor and mark conjunctiva with gentle cautery (monopolar or bipolar) 8.0 mm (for 2 mm of lift) above upper tarsal border centrally above the pupil (Fig. 54.1). See step 5 for table of magnitude of resection. 5. Mark 4 mm above the tarsal border in the medial and lateral eyelid, approximately 15 mm apart centered on the pupil (Table 54.1). Figure 54.2 6. Apply locking Castroviejo forceps (6-0 mm long silk traction sutures may be substituted) to medial and lateral marks (Fig. 54.2). 7. Remove Desmarres retractor. Figure 54.3 8. With the assistant tenting up tissues within the locking Castroviejo forceps, apply the ptosis clamp with the top of the clamp to the previously placed mark 8 mm above tarsal border (Fig. 54.3). a. Clamp includes 8 mm of conjunctiva and adherent Müller muscle. b. Clamp advances the levator aponeurosis internally. 9. Sew 6-0 plain suture lateral to medial across eyelid in horizontal fashion approximately 1 mm below clamp (Fig. 54.4). Figure 54.4 Figure 54.5 10. Use scalpel (e.g. #15 Bard-Parker blade) to excise tissue within clamp (Fig. 54.5). a. Angle scalpel toward metal clamp to prevent cutting of suture. Figure 54.6 11. Sew medial to lateral in simple running fashion (Fig. 54.6). a. Expect fine oozing from tissues (absence of epinephrine). Have assistant wipe ahead of surgeon with cotton applicators. 12. Tie two ends of suture together. 13. Apply antibiotic ointment to eye. 14. Apply iced compresses. 1. Apply ice packs to decrease swelling. 2. Apply antibiotic ointment 4 times daily to eye for lubrication. 1. Lid swelling and ecchymosis 2. Corneal abrasion secondary to suture irritation 3. Lid hemorrhage 4. Over- and undercorrections 5. Lid asymmetry 6. Poor lid contour 7. Malpositioned or indistinct lid crease 8. Exposure keratopathy secondary to lagophthalmos Like the posterior Müller muscle–conjunctival resection procedure, the Fasanella-Servat procedure is useful for mild cases of ptosis (2 mm or less) with good levator function (8 mm or more). It is the most technically straightforward of the ptosis procedures performed. Because the tarsal plate is vertically shortened, there is increased risk of central “peaking” of the eyelid compared to the Müller muscle–conjunctival resection procedure. Additionally, the vertical shortening of the tarsal plate that results from this procedure may make additional ptosis surgeries more difficult. See Chapter 3. 1. If possible, discontinue aspirin and nonsteroidal anti-inflammatory agents for 10 days before surgery. Discontinue warfarin 2–3 days preoperatively, if medically possible. 2. Query patient about bleeding tendencies. A useful screening question is asking if the patient had unusual bleeding after dental extraction. Obtain hematological evaluation if bleeding tendency is suspected. 1. Apply topical anesthetic. 2. Anesthesia: Local infiltrative anesthetic or general anesthetic in children and uncooperative patient. 3. Prep and drape. a. Keep both eyes exposed for comparison of two eyes during procedure. 4. Place scleral shell to protect globe (not shown in illustrations). Figure 54.7 5. Use scalpel (e.g., #11 Bard-Parker blade) to make small stab incision through skin at lateral border of lid crease (Fig. 54.7). Figure 54.8 6. Evert upper lid (Figs. 54.7 and 54.8). 7. Clamp two small curved hemostats across upper tarsal border encompassing superior tarsus, the inferior edge of the Müller muscle, and overlying conjunctiva. a. Place 2–3 mm from superior edge of tarsus. b. Ensure that the clamps are positioned so the width of engaged tarsus is constant along the entire length of the clamps. This avoids resecting too much tarsus centrally. c. Ensure that neither skin nor levator aponeurosis has been imbricated by the clamp. 8. Run one end of a double-armed 6-0 plain gut suture in mattress fashion, approximately 1 mm above the hemostats. a. Place full thickness through all tissues (inferior conjunctiva-tarsus Müller muscle–superior conjunctiva). b. Start medially and take approximately 4–6 bites, proceeding laterally. 9. Remove hemostats (Fig. 54.9). Figure 54.9 10. Cut through crush marks with Stevens scissors. a. Only upper tarsus, inferior portion of the Müller muscle, and conjunctiva should be removed. No more than one half of tarsus should be resected. b. Do not cut through levator aponeurosis and skin. Figure 54.10 11. Using the medial free arm of the suture placed in step 8 as a running suture, rejoin superior tarsal edge and inferior border of the Müller muscle while approximating the cut conjunctival edges (Fig. 54.10). 12. Carry both arms of the suture through the preplaced skin stab incision, tie the ends, and bury the knot beneath skin. 13. The skin incision usually does not need suturing. 14. Remove scleral shell. 15. Apply antibiotic ointment to eye. 16. Apply chilled compress. 1. Apply ice packs to decrease swelling. 2. Apply antibiotic ointment 4 times daily for corneal lubrication. 1. Lid swelling and ecchymosis 2. Corneal abrasion secondary to suture irritation 3. Asymmetry of lids 4. Poor lid contour Levator aponeurotic advancement or repair is useful in cases of uncomplicated congenital or acquired ptosis of any magnitude with 5 or more mm of levator function. With poorer levator function, a levator resection or frontalis suspension should be considered.
Ptosis Repair
 Introduction
Introduction
 Neurogenic (e.g., third nerve palsy, Horner syndrome)
Neurogenic (e.g., third nerve palsy, Horner syndrome)
 Myogenic (e.g., most congenital ptosis, chronic progressive ophthalmoplegia)
Myogenic (e.g., most congenital ptosis, chronic progressive ophthalmoplegia)
 Aponeurotic (involutional due to levator aponeurotic thinning, stretching, dehiscence, and disinsertion)
Aponeurotic (involutional due to levator aponeurotic thinning, stretching, dehiscence, and disinsertion)
 Mechanical (e.g., eyelid masses)
Mechanical (e.g., eyelid masses)
 “Pseudo”-ptosis (e.g., enophthalmos, phthisis bulbi, contralateral eyelid retraction).
“Pseudo”-ptosis (e.g., enophthalmos, phthisis bulbi, contralateral eyelid retraction).
Preoperative Procedure
 Müller Muscle–Conjunctival Resection
Müller Muscle–Conjunctival Resection
Indications
 Mild ptosis (less than 3.0 mm lid droopy) with good levator function (10 mm or greater).
Mild ptosis (less than 3.0 mm lid droopy) with good levator function (10 mm or greater).
 Significant reversal of ptosis with administration of 2.5% phenylephrine hydrochloride in superior conjunctival fornix.
Significant reversal of ptosis with administration of 2.5% phenylephrine hydrochloride in superior conjunctival fornix.
Preoperative Procedure
Instrumentation
 Scalpel (e.g., #15 Bard-Parker blade)
Scalpel (e.g., #15 Bard-Parker blade)
 Putterman ptosis clamp (Karl-Ilg)
Putterman ptosis clamp (Karl-Ilg)
 Sutures (6-0 plain gut)
Sutures (6-0 plain gut)
 Needle holder
Needle holder
 Toothed forceps
Toothed forceps
 Locking toothed forceps
Locking toothed forceps
Operative Procedure
Postoperative Procedure
Complications
 Fasanella-Servat Procedure
Fasanella-Servat Procedure
Indications
 Mild congenital ptosis (less than 2 mm lid droop), with good levator function (8 mm or more)
Mild congenital ptosis (less than 2 mm lid droop), with good levator function (8 mm or more)
 Select cases of mild acquired involutional ptosis
Select cases of mild acquired involutional ptosis
 Mild ptosis associated with Horner syndrome
Mild ptosis associated with Horner syndrome
Preoperative Procedure
Instrumentation
 Tissue marking pen
Tissue marking pen
 Scleral shell
Scleral shell
 Scalpel
Scalpel
 Small curved hemostats
Small curved hemostats
 Sutures (double-armed 6-0 plain gut)
Sutures (double-armed 6-0 plain gut)
 Needle holder
Needle holder
 Stevens scissors
Stevens scissors
 Toothed forceps
Toothed forceps
Operative Procedure
Postoperative Procedure
Complications
 Ptosis Repair by External Levator Aponeurosis Advancement
Ptosis Repair by External Levator Aponeurosis Advancement
Indications
 Acquired (involutional, traumatic) ptosis secondary to thinning, stretching, dehiscence, or disinsertion of the levator aponeurosis
Acquired (involutional, traumatic) ptosis secondary to thinning, stretching, dehiscence, or disinsertion of the levator aponeurosis
 Select cases of congenital ptosis with good levator function
Select cases of congenital ptosis with good levator function
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree