9
Principles of Macular Laser Surgery
Alexander J. Brucker  Tushar M. Ranchod
Tushar M. Ranchod
Lasers have diverse applications in the treatment of posterior segment disease. All of these applications rely on the common characteristics of laser light: monochromatism, coherence, and directionality (1). Laser is an acronym for Light Amplification by Stimulated Emission of Radiation, a name which succinctly describes the mechanism of action.
Light is produced by the release of photons in one of two ways. An unexcited atom may be stimulated to an excited state and then spontaneously release a photon as it decays to the lower energy level (spontaneous emission). In lasers, however, a single photon strikes an excited atom to stimulate the release of a second photon (stimulated emission). This stimulated emission results in two photons with uniform frequency and phase (coherence). A chain reaction of stimulated emission requires population inversion, in which the rate of excitation to a higher energy state exceeds the rate of decay to a lower energy state. The released energy (in the form of photons) is amplified by enclosing the system within mirrors. Light is reflected back and forth within the laser, and a partial reflector at one end of the instrument allows a fraction of the light to leave in a single direction (limited divergence). Figure 9-1 illustrates a simple laser.
WAVELENGTH SELECTION
The specific wavelength of light produced by a laser depends on the choice of lasing medium. Media used in ophthalmic lasers include solid-state materials (i.e., neodymium-Yag), gases (i.e., argon, krypton), organic dyes, combinations of reactive and inert gases (i.e., excimer), and semiconductors (i.e., diode) (2–4). Laser wavelength determines absorption by anatomic structures and pigments as well as scatter by media opacities.
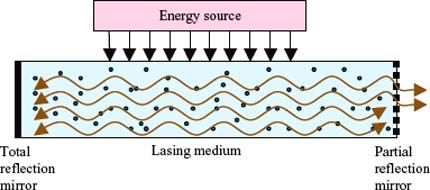
Figure 9-1. Illustration of a simple laser.
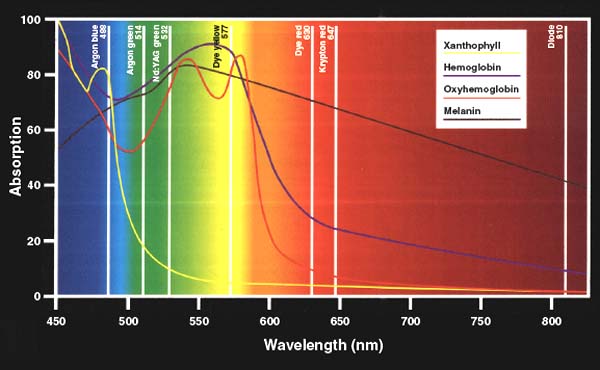
Choice of wavelength during macular laser surgery must account for retinal pigments and their absorptive characteristics with respect to therapeutic goals. Melanin, located in the retinal pigment epithelium (RPE) and choroidal melanocytes, has a broad spectrum of absorption and generally does not influence wavelength choice (5). By contrast, hemoglobin in arterial and venous blood, and xanthophylls in the inner and outer plexiform layers possess narrower spectra of absorption. In general, laser light is not well absorbed by pigments of a similar color wavelength (6). For example, the yellow pigment xanthophyll absorbs yellow laser light poorly while hemoglobin absorbs red laser light poorly but absorbs yellow wavelengths well. For this reason, yellow wavelengths are useful for focal macular treatment both to avoid uptake in the fovea, where xanthophyll is most concentrated, and to focus concentration on vascular lesions such as micro-aneurysms. Blue wavelengths are not widely used any longer due to absorption by xanthophylls causing undesired inner segment damage, as well as greater scatter than other visible wavelengths (5).
Longer wavelengths such as red tend to penetrate more deeply than shorter wavelengths such as green, and longer wavelengths are scattered less by media opacities such as cataract. Figure 9-2 illustrates the absorption properties of various ophthalmic lasers by retinal pigments.
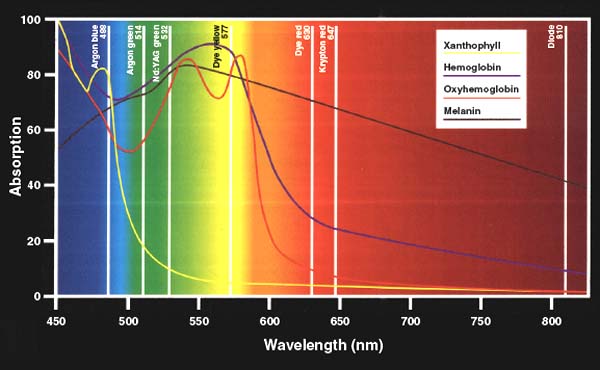
Figure 9-2. Illustration of the absorption properties of various ophthalmic lasers by retinal pigments. (From laser surgery of the posterior segment Bloom SM, Brucker AJ, 1997, 2nd ed, Lippincott Raven. Figure 1-3 Absorption characteristics of the major ocular pigments for the wavelengths current used for posterior segment photocoagulation, reprinted with permission)
TISSUE EFFECTS
The combination of wavelength and power determines a laser’s effect on tissue. These effects can be classified as photocoagulative, photodisruptive, photoablative, or photochemical. Photocoagulation results when tissue pigments absorb laser energy and tissue temperature rises enough to cause protein denaturation. Panretinal photocoagulation (PRP) with an argon laser is an example of photocoagulation. Photodisruption occurs when concentrated power delivery creates a shock wave that disrupts tissue bonds. The Nd:Yag laser’s photodisruptive properties allow for the creation of iridotomies and capsulotomies and can be used to disrupt the posterior hyaloid face, for example in cases of premacular hemorrhage (3, 7). Photoablation results when laser energy elevates the temperature of water to the point of vaporization. Excimer lasers use photoablation to reshape the cornea in procedures such as laser in situ keratomileusis, and excessive burns during retinal photocoagulation may result in photoablation of posterior segment tissues (8). Photochemical reactions, also known as photoactivation, occur when laser energy alters chemical bonds in order to activate a target compound (1). Photodynamic therapy with verteporfin is an example of photochemical activation, in which a 489 nm nonthermal diode laser is used to locally activate intravenously injected verteporfin within a treatment zone, thereby resulting in occlusion of a neovascular membrane (9).
DELIVERY MODALITIES
Laser treatments to the posterior segment can be delivered using a variety of modalities. A slit lamp-mounted laser may be used in combination with a variety of lenses, discussed later in this chapter. A laser fitted to an indirect ophthalmoscope allows treatment with less accuracy but more flexibility than a slit lamp-mounted laser; this setup is often useful for patients who cannot sit comfortably or safely in a chair, or when treatment must be delivered to the far periphery. Laser treatments may also be delivered intraoperatively using an endoscopic laser probe, thereby bypassing anterior segment media opacities (10, 11).
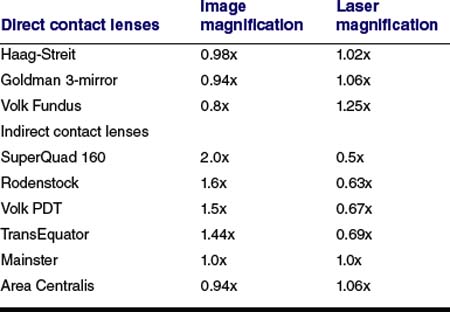
A surgeon may choose from a wide variety of lenses when delivering laser treatment to the posterior segment (12). A contact lens is generally used at the slit lamp, with the benefit of stabilizing the globe and ensuring an uninterrupted view during treatment. Contact lenses may provide direct views (virtual, upright image) or indirect views (real, inverted image) at a variety of magnifications (13). Lower image magnification is used for treatments over wide areas, such as panretinal photocoagulation, while higher image magnification is used for macular treatments. Laser spot size magnification is inversely related to angular image magnification, so that lenses which magnify the surgeon’s fundus view will proportionately minify the laser spot size (13). Table 9-1 provides a list of commonly used contact lenses along with their image and laser magnification characteristics.
TABLE 9-1 COMMON CONTACT LENSES WITH MAGNIFICATION CHARACTERISTICS
Noncontact lenses can be used at the slit lamp or with the indirect headset. Noncontact lenses are helpful at the slit lamp when corneal contact is undesirable, as in the case of a corneal erosion or wound. The condensing lenses used are generally the same as those used for clinical examination. As with contact lenses, laser spot size is minified as an inverse function of retinal image magnification. Image and laser spot magnification depend in part upon the diopteric power of the condensing lens, with lower power lenses providing greater image magnification and spot size minification. Treatment with the indirect headset introduces further complexity to spot size determination, since the degree of image and laser spot magnification varies with the surgeon’s working distance from both the condensing lens and patient (14
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


