Primary Intraocular Lens Implantation in Children
Rupal H. Trivedi
M. Edward Wilson
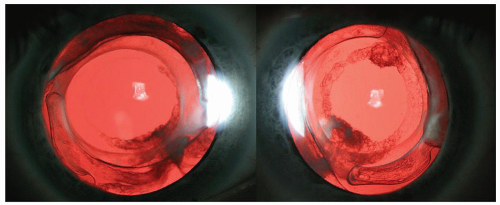
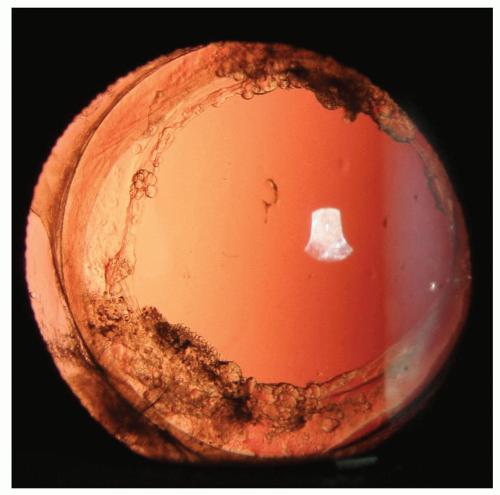
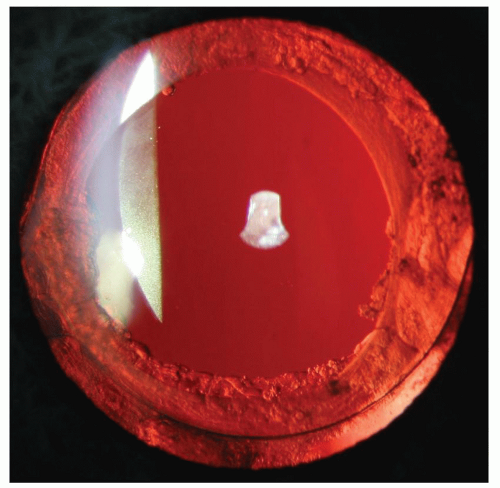
Primary intraocular lens (IOL) implantation has become the most common method used to correct aphakia in children beyond their first birthday (Figs. 25.1, 25.2, 25.3, 25.4). However, it is still considered an “off-label” (or “physician directed”) use by the U.S. Food and Drug Administration (FDA). It provides the benefit of at least a partial but uninterrupted optical correction, which is an important advantage to the visual development in amblyopia-prone eyes. Uncorrected pseudophakic vision is probably less amblyogenic than uncorrected aphakic vision. While there is certainly a benefit to IOL implantation by reducing the dependency on compliance with other external optical treatments (aphakic glasses and contact lenses), it was slow to catch on in children as compared with adults. This is because many early attempts at IOL implantation in children resulted in severe complications. Lack of awareness of the need for primary posterior capsulectomy and vitrectomy, poor IOL design, and the inherent propensity for an increased inflammatory response that occurs in a child’s eye after intraocular surgery resulted in this higher rate of postoperative complications. IOL implantation in children began to increase steadily only after 1990, even though its first reported use was in 1952 as a secondary IOL in a 12-year-old aphakic child.1 The use of mechanized vitrectomy instrumentation to perform a primary posterior capsulectomy and vitrectomy combined with implantation of better-quality IOLs resulted in fewer complications in children. This encouraged more and more surgeons to use IOLs for children and to gradually decrease the lower limit for age of implantation. Binkhorst and Hiles pioneered the use of IOLs in children in the 1970s and 1980s.2,3 Surgeons were initially hesitant to implant adult-size IOLs (even high-quality IOLs) in the pediatric age group until a number of studies began to show their safety and efficacy in children.4,5,6,7 Although IOL implantation in children was mostly investigational before the mid-1990s, since that time, its use has risen dramatically among pediatric cataract surgeons. In 1996 editorial, Wilson8 stated that IOL implantation had become the standard of care for uncomplicated cataract surgeries in children beyond infancy. The dramatic increase in acceptance of IOL implantation in children was noticeable when comparing our 1993 practice preferences survey data with that of our 2001 practice preferences survey. We showed a nearly fivefold increase in the number of respondents from the American Society of Cataract and Refractive Surgeons (ASCRS) and more than a 13-fold increase in the number of respondents from the American Association for Pediatric Ophthalmology and Strabismus (AAPOS) implanting IOLs in children ≤2 years.9
IOL IMPLANTATION IN INFANTS
As primary IOL implantation has become more broadly used, the age in which the procedure is acceptable and appropriate has steadily decreased. IOL implantation is common for children undergoing cataract surgery beyond infancy (Fig. 25.5). For bilateral cataract during infancy, aphakic glasses and/or contact lens use may be a reasonable option; however, for unilateral cataract, we were equipoised between whether or not to offer primary IOL implantation at the time of infantile cataract surgery. The Infant Aphakia Treatment Study (IATS) was a multicenter, randomized, controlled clinical trial comparing the outcomes of contact lens versus IOL correction for monocular aphakia during infancy. The 1-year results were published in 2010 and the 5-year results are being published in 2014.10 In the 1-year outcome study report, the authors advised that until longer-term follow-up data are available, caution should be exercised when performing IOL implantation in children aged 6 months or younger given the higher incidence of adverse events and the absence of an improved short-term visual outcome compared with contact lens use.10
Table 25.1 describes the arguments for and against primary IOL implantation in infantile cataract surgery. The important concerns about primary IOL implantation during infancy are the technical difficulties of implanting an IOL and selecting an IOL power, and the higher rate of visual axis opacification (VAO). Despite performing primary posterior capsulectomy and vitrectomy, the rate of
VAO is higher in pseudophakic infantile eyes as compared with aphakic infantile eyes.11,12 The IATS reported that at the 1-year visit, more patients in the IOL group had undergone one or more additional intraocular operations than did patients in the contact lens group (63% vs. 12%; P < 0.001). Most of these additional operations were performed to clear lens reproliferation and pupillary membranes from the visual axis.10 For IATS patients up to 12 months of age, cataract surgery coupled with IOL implantation and spectacle correction was 37.5% (approximately $4,000) more expensive than was cataract surgery coupled with contact lens correction.13
VAO is higher in pseudophakic infantile eyes as compared with aphakic infantile eyes.11,12 The IATS reported that at the 1-year visit, more patients in the IOL group had undergone one or more additional intraocular operations than did patients in the contact lens group (63% vs. 12%; P < 0.001). Most of these additional operations were performed to clear lens reproliferation and pupillary membranes from the visual axis.10 For IATS patients up to 12 months of age, cataract surgery coupled with IOL implantation and spectacle correction was 37.5% (approximately $4,000) more expensive than was cataract surgery coupled with contact lens correction.13
The main concerns of contact lens correction are poor compliance, high lens loss rate, high cost, and keratitis (Fig. 25.6). These challenges make contact lenses impractical in many children especially in most parts of the developing world. It is certainly possible for an eye with a unilateral infantile cataract to achieve a good visual outcome following contact lens correction. However, it has continued to be the exception rather than the rule when contact lens
losses are high. Both IOLs and aphakic contact lenses may support similar visual acuity after surgery for unilateral cataract in the presence of good compliance and a low loss of contact lenses. However, IOLs support better visual acuity in those situations when compliance with contact lens wear is moderate or poor or when contact lens replacements/refittings are a hardship because of cost or transportation difficulties.14
losses are high. Both IOLs and aphakic contact lenses may support similar visual acuity after surgery for unilateral cataract in the presence of good compliance and a low loss of contact lenses. However, IOLs support better visual acuity in those situations when compliance with contact lens wear is moderate or poor or when contact lens replacements/refittings are a hardship because of cost or transportation difficulties.14
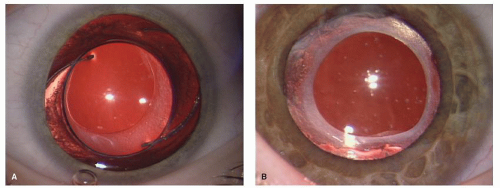 Figure 25.4. Postoperative follow-up showing a clear visual axis. A: Note haptic compression and peripheral capsular changes. B: Note well-centered IOL and anterior capsule opacification. |
Contact lens correction is the most commonly chosen option for aphakic correction in early infancy in our practice, especially in bilateral cataract patients. In unilateral cases, primary IOL implantation is more often chosen when compared to bilateral cases. This is especially true in families in which contact lens care is predicted to be difficult. In our state, Medicaid does not pay for contact lenses even when we write letters stating that the contact lenses are medically necessary. We prefer silicone SilSoft contact lenses; however, these lenses cost more than U.S. $150 each and are often lost or in need of frequent replacement. Many poor families will not be able to afford this expense. In these families, IOL implantation with glasses for residual hyperopia is given more consideration since it may be the only viable option when the cataract is unilateral. To its credit, Bausch & Lomb SilSoft Contact Lens Patient Assistance Program (http://www.bausch.com/Search%20Results?searchtext=Silsoft+Contact+Lens+Patient+Assistance+Program+) has worked well for us. Typically when patients lose a lens, they are told to call our central scheduling number during working hours, and then one of our pediatric ophthalmology clinic technicians return the call and determine if they have the means to purchase a replacement contact lens. If so, we send a script and inform them of the online ordering sites, such as Walgreens.com. If we determine that they cannot afford to replace the lens, we order one for them through the Bausch & Lomb Patient Assistance Program by filling out an online form. We explain to the family that if they qualify for the Bausch & Lomb program, they can receive up to one free SilSoft lens order (maximum two lenses per order) every 3 months but that a new form must be filled out for each new order. The free lenses are shipped to us, and we mail them to the family or insert them at the next office visit.
WHAT IOL TO IMPLANT?
Type of IOL
Since posterior capsule opacification (PCO) is one of the most frequent and severe complications in pediatric cataract surgery, an IOL that decreases the incidence of PCO is more often used in pediatric cataract surgery.15,16 The choice of an IOL material and type for children is a modified version of what has evolved for adults. A biocompatible material that could be inserted via a smaller incision and fit the smallest capsular bag without excessive stretching is preferred.17 Our 2001 survey of ASCRS and AAPOS members reported that 66.8% of ASCRS respondees and 71.7% of AAPOS respondees preferred hydrophobic acrylic IOLs when implanting lenses in children.9 A later survey of AAPOS members conducted in 2006 showed that for in-the-bag fixation, hydrophobic acrylic IOLs were preferred by 93.3% of the respondents.18 AcrySof® hydrophobic acrylic lenses were preferred by 90.2% of respondents. Among AcrySof® users, more physicians preferred the single-piece AcrySof® lens for bag fixation of an IOL. For ciliary sulcus fixation of an IOL, hydrophobic acrylic IOLs were preferred by 69.9% of the respondents, and the AcrySof® hydrophobic acrylic IOL was preferred by 65.3% of overall respondents.
Among those implanting AcrySof®, most preferred the three-piece AcrySof® IOL for sulcus fixation. There are several published case series detailing the use of hydrophobic acrylic IOLs in children.9,12,15,17,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36



Among those implanting AcrySof®, most preferred the three-piece AcrySof® IOL for sulcus fixation. There are several published case series detailing the use of hydrophobic acrylic IOLs in children.9,12,15,17,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree