Postsurgical Contact Lens Fitting
Michael DePaolis
Joseph Shovlin
Julie Ott DeKinder
Christine Sindt
One of the most challenging and rewarding aspects of contact lens practice involves the postsurgical fit. In each case, the clinician is faced with a complex ocular surface, one in which both structure and function have been altered. As the patient’s contact lens needs are more therapeutic than cosmetic, and as there are few definitive prescribing guidelines, clinicians must be cautious, creative, and conservative. Although the fitting process can be an arduous one, patient gratification is often well worth it.
In this chapter, we will address the most common reasons for postoperative contact lens fitting, including penetrating keratoplasty (PK), radial keratotomy (RK), photorefractive keratectomy (PRK), laser-assisted in situ keratomileusis (LASIK), laser epithelial keratomileusis (LASEK), intrastromal ring segments (Intacs), and ocular trauma. For each application, we will discuss the rationale for perioperative and postoperative contact lens use. We will also review the topographic and physiologic challenges and the recommended fitting philosophies given these limitations. Finally, additional surgical options, should the patient prove to be contact lens intolerant, will be briefly discussed.
▪ PENETRATING KERATOPLASTY
Full-thickness PK remains the surgical procedure of choice for many corneal conditions. In 2006, 33,962 PKs were performed in the United States, which was an increase from the 31,952 preformed the previous year.1 PKs are performed regularly for a variety of reasons, including keratoconus, Fuch corneal dystrophy, pseudophakic bullous keratopathy, and herpes simplex stromal leukoma. A 20-year retrospective study determined that the most common indication for PK was aphakic/pseudophakic bullous keratopathy, followed by keratoconus and corneal scars.2 Through the development of improved tissue typing and harvesting, microsurgical techniques, and postsurgical immunomodulating therapeutics, PK has become a very safe and efficacious procedure. Unfortunately, as we are introducing a different donor cornea to the recipient bed, component ametropia often results, which can be quite varied from the fellow eye, with resultant anisometropia. Furthermore, as graft-host junction wound healing occurs in a radially variable fashion, irregular astigmatism often prevails. Given these scenarios, an otherwise successful surgical endeavor can be obscured by a poor outcome with traditional spectacle correction.
Contact Lens Rationale
Over time, several methods have been tried to treat postkeratoplasty irregular astigmatism. These include wedge resections, relaxing incisions,3 customized laser ablation,4 laser in situ keratomileusis,5 and photorefractive keratectomy.6 In consideration of the latter three surgical procedures, LASIK has become the surgical method of choice, but it, like the other two, is
still plagued with unintentional complications such as undercorrection or overcorrection, haze, and possible rejection of the graft,7 leaving contact lenses as the most logical solution. A retrospective chart review of patients who had LASIK following PK showed 3-month followup results of 20/60 or better in all eyes; however, only one eye was reported to have achieved 20/20 vision. The success rate was significant in myopic eyes, but not in hyperopic eyes.8 Corneal contact lenses in general, and rigid gas permeable (GP) lenses in particular, are well recognized for their ability to compensate for anisometropia and irregular astigmatism. In the case of unilateral PK, the patient may prefer an ipsilateral contact lens in which the prescription is balanced with the contralateral spectacle-wearing eye. In the case of bilateral PK, particularly when significant astigmatism is involved, the patient may prefer a bilateral contact lens correction. In addition to their role in long-term ametropia management, contact lenses are often used after PK for bandage purposes. In certain PK procedures, the graft is slow to reepithelialize, often requiring more than the traditional 1-week period of time. For these individuals, a bandage contact lens often provides protection to the sliding epithelium. The most prudent approach involves a hydrophilic bandage lens worn on an extended wear basis until epithelial closure occurs. As this is often a critical time from a graft rejection and infectious keratitis perspective, patients must receive concomitant topical antibiotic and steroid therapeusis. Additionally, the patient must be closely monitored on a 24- to 48-hour basis. Another reason for a hydrophilic bandage lens during the perioperative period involves the use of interrupted sutures in which the knots are not buried. Many surgeons attempt to modulate postsurgical astigmatism through the use of a continuous suture in conjunction with 6 to 12 interrupted sutures. While the continuous suture may remain in place for 12 months or longer, interrupted sutures are often removed as early as 8 weeks after surgery. Until their removal, however, the interrupted sutures can cause a significant foreign body sensation as well as papillary conjunctivitis. In these cases, a hydrophilic bandage lens can significantly reduce suture awareness and progression of papillary conjunctivitis. The bandage lens is often left in place for up to a week at a time, and ultimately discontinued when the interrupted sutures are removed. In both of these applications, disposable lenses have demonstrated good clinical efficacy.9 Disposable lenses offer significant benefits over more time-honored conventional hydrophilic bandage lenses. Moreover, disposable silicone hydrogel lenses offer the greatest benefits. Silicone hydrogel disposable lenses lend greater oxygen transmissibility than disposable hydrophilic lenses and have become the modality of choice in PK patients. The primary advantage of a disposable bandage lens is that of preventing the immunogenic, toxic, and mechanical sequelae of a spoiled contact lens. As the perioperative PK eye is often inflamed and requires numerous topical agents, bandage lens spoilage is quite common. When using a disposable bandage lens, the patient has the opportunity of discarding the lens on a weekly basis. Another advantage of disposable bandage lenses involves ease of replacement. During the perioperative phase, PK patients can inadvertently dislodge the bandage lens with their eye drops or while sleeping, and frequent replacement of a conventional lens can be quite cost prohibitive relative to a disposable lens. Silicone hydrogel disposable contact lenses have obvious advantages over hydrophilic disposable lenses as extended wear bandages. Hydrophilic disposable contact lenses, when worn as extended wear bandages, must be monitored for relative corneal hypoxia because of their relative low oxygen permeability (Dk) value. Limiting corneal hypoxia is especially important during the perioperative phase when contact lensrelated edema can either mimic or exacerbate graft rejection. Disposable lenses have essentially rendered conventional lenses obsolete; the one exception may be when extreme curvature changes are necessary or when a very large lens (15-20 mm) is necessary (i.e., for healing an associated leaking bleb). Custom hydrogel and, more recently, custom silicone hydrogel lenses offer good comfort, reproducibility, and quality for the management of challenging irregular cornea patients.
still plagued with unintentional complications such as undercorrection or overcorrection, haze, and possible rejection of the graft,7 leaving contact lenses as the most logical solution. A retrospective chart review of patients who had LASIK following PK showed 3-month followup results of 20/60 or better in all eyes; however, only one eye was reported to have achieved 20/20 vision. The success rate was significant in myopic eyes, but not in hyperopic eyes.8 Corneal contact lenses in general, and rigid gas permeable (GP) lenses in particular, are well recognized for their ability to compensate for anisometropia and irregular astigmatism. In the case of unilateral PK, the patient may prefer an ipsilateral contact lens in which the prescription is balanced with the contralateral spectacle-wearing eye. In the case of bilateral PK, particularly when significant astigmatism is involved, the patient may prefer a bilateral contact lens correction. In addition to their role in long-term ametropia management, contact lenses are often used after PK for bandage purposes. In certain PK procedures, the graft is slow to reepithelialize, often requiring more than the traditional 1-week period of time. For these individuals, a bandage contact lens often provides protection to the sliding epithelium. The most prudent approach involves a hydrophilic bandage lens worn on an extended wear basis until epithelial closure occurs. As this is often a critical time from a graft rejection and infectious keratitis perspective, patients must receive concomitant topical antibiotic and steroid therapeusis. Additionally, the patient must be closely monitored on a 24- to 48-hour basis. Another reason for a hydrophilic bandage lens during the perioperative period involves the use of interrupted sutures in which the knots are not buried. Many surgeons attempt to modulate postsurgical astigmatism through the use of a continuous suture in conjunction with 6 to 12 interrupted sutures. While the continuous suture may remain in place for 12 months or longer, interrupted sutures are often removed as early as 8 weeks after surgery. Until their removal, however, the interrupted sutures can cause a significant foreign body sensation as well as papillary conjunctivitis. In these cases, a hydrophilic bandage lens can significantly reduce suture awareness and progression of papillary conjunctivitis. The bandage lens is often left in place for up to a week at a time, and ultimately discontinued when the interrupted sutures are removed. In both of these applications, disposable lenses have demonstrated good clinical efficacy.9 Disposable lenses offer significant benefits over more time-honored conventional hydrophilic bandage lenses. Moreover, disposable silicone hydrogel lenses offer the greatest benefits. Silicone hydrogel disposable lenses lend greater oxygen transmissibility than disposable hydrophilic lenses and have become the modality of choice in PK patients. The primary advantage of a disposable bandage lens is that of preventing the immunogenic, toxic, and mechanical sequelae of a spoiled contact lens. As the perioperative PK eye is often inflamed and requires numerous topical agents, bandage lens spoilage is quite common. When using a disposable bandage lens, the patient has the opportunity of discarding the lens on a weekly basis. Another advantage of disposable bandage lenses involves ease of replacement. During the perioperative phase, PK patients can inadvertently dislodge the bandage lens with their eye drops or while sleeping, and frequent replacement of a conventional lens can be quite cost prohibitive relative to a disposable lens. Silicone hydrogel disposable contact lenses have obvious advantages over hydrophilic disposable lenses as extended wear bandages. Hydrophilic disposable contact lenses, when worn as extended wear bandages, must be monitored for relative corneal hypoxia because of their relative low oxygen permeability (Dk) value. Limiting corneal hypoxia is especially important during the perioperative phase when contact lensrelated edema can either mimic or exacerbate graft rejection. Disposable lenses have essentially rendered conventional lenses obsolete; the one exception may be when extreme curvature changes are necessary or when a very large lens (15-20 mm) is necessary (i.e., for healing an associated leaking bleb). Custom hydrogel and, more recently, custom silicone hydrogel lenses offer good comfort, reproducibility, and quality for the management of challenging irregular cornea patients.
Special Considerations
As is true of any surgically altered cornea, the PK patient presents with a variety of special considerations and relative contraindications to contact lens wear. These alterations can affect both structure and function. Structural changes most often involve topographic alterations, whereas functional changes pertain to adverse physiologic sequelae.
The topographic alterations associated with PK can be profound. First and foremost is the fact that a donor cornea, often of significantly different curvature, is placed in the recipient bed. The actual apposition between host and recipient often alters the cornea’s natural asphericity. The overall resulting curvature is further influenced by surgical technique and wound healing. Most PK surgeons attempt to trephinate a recipient bed, which is slightly smaller than the donor button. In doing so, the surgeon is able to ensure good wound coaptation (i.e., alignment and adhesion of the wound), maintain adequate anterior chamber depth, avoid peripheral anterior synechiae, and reduce the risk of postoperative glaucoma. However, if the recipient bed is too small or the donor button too large, a “proud” or very steep topography results. In the opposite scenario, one in which the donor button is too small for the recipient bed, the patient may encounter poor wound coaptation, a shallow chamber with peripheral synechiae, and increased risk of glaucoma. As a result of the donor cornea being drawn across the recipient bed, the topography is often “plateaued” or oblate. Either an excessively steep or flat cornea can be further complicated by graft “tilt.” It is extremely important to qualitatively assess topographic morphology as this often influences the initial lens design selection.
In addition to the topographic morphologic changes associated with penetrating keratoplasty, the contact lens clinician must also manage a significant amount of astigmatism. It is not uncommon for the post-PK patient to manifest 5 D or more of astigmatism.10 Although varying suturing technique and removal strategies can assist in reducing the probability of increased amounts of astigmatism, the surgeon is still at the mercy of individual wound healing. Furthermore, the astigmatism is often complicated by an irregular presentation. In fact, it is prudent to view the post-PK steep corneal meridian as two hemi-meridians that are not always orthogonal to the flat meridian.
The physiologic alterations associated with PK are numerous. Although many improvements have been made in tissue harvesting, transportation, and transplantation, the endothelium is still prone to cell loss. Given the fact that a viable endothelium is necessary to avoid graft rejection and expiration, it is especially important that the contact lens does not exacerbate polymegethism. Although the donor epithelium is entirely replaced by recipient epithelium within the first month, it is imperative that this tissue is protected throughout the graft’s life. Poorly fit contact lenses that result in chronic epithelial edema, superficial punctate keratitis, or corneal abrasion can ultimately precipitate epithelial graft rejection.11 Microcystic edema may be present, however, which is entirely independent of contact lens wear. Contraindications to fitting contact lenses include epithelial defects, inflammation, corneal edema, and loose sutures.7 Additionally, many PK patients manifest some degree of corneal neovascularization that may be because of the preexisting corneal condition or a result of a volatile postoperative course. Regardless of its cause, corneal neovascularization must be held in check when prescribing contact lenses. A poorly fit contact lens can result in inflammation and progression of corneal neovascularization. Another aspect of PK surgery is the total hypoesthesia that ensues. Although some reinnervation occurs after PK, it rarely does so completely. As a result, the PK patient experiences decreased corneal sensitivity and an iatrogenic keratitis sicca.12 Of course, contact lenses can aggravate the already dry eye, which, in turn, can limit contact lens wear.
Contact Lens Options
In light of the aforementioned alterations in corneal structure and function, it is understandable why contact lens fitting can be such a challenge. Contact lenses can be prescribed for visual restoration as early as 3 months post-PK on clear grafts.13 The course of suture removal is
highly dependent on the individual surgeon, but the presence of sutures should not be a contraindication to contact lens fitting. While a suture may complicate corneal topography, a contact lens fit can be highly successful, without increased risk of complications.
highly dependent on the individual surgeon, but the presence of sutures should not be a contraindication to contact lens fitting. While a suture may complicate corneal topography, a contact lens fit can be highly successful, without increased risk of complications.
Gas Permeable Contact Lenses
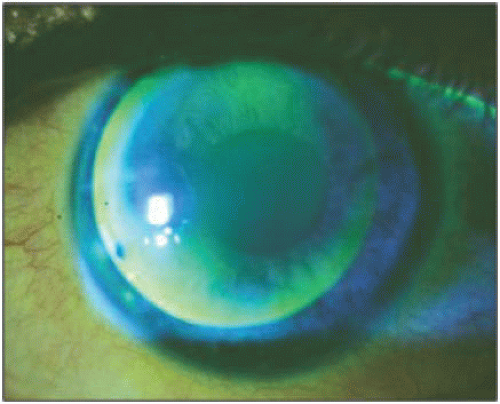
GP lenses are the most frequently prescribed contact lenses after PK, largely because of their ability to mask significant irregular astigmatism as well as to provide for an excellent physiologic response. However, given the often unusual post-PK topography, achieving an adequate fit can be difficult (Fig. 19.1).
Lens Materials:
The excellent oxygen transmission, good surface characteristics, and flexure resistance of most fluoro-silicone/acrylate (F-S/A) lens materials make this category a reasonable choice for post-PK fitting. An ultrathin, hyper Dk material is a reasonable option when considering maximum oxygen transmissibility; however, the highly flexible nature of this material still places it as a second choice behind lower Dk F-S/A materials.
Overall Diameter:
The concept of a small diameter (7.0-8.0 mm) GP fit within the graft-host junction has been abandoned in recent years as poor comfort, inconsistent positioning, and easy displacement often prevails. Today’s post-PK GP lenses are often 9.5 to 12.0 mm in diameter. In addition, several mini-scleral and semi-scleral designs have been introduced with diameters often in the 13.5- to 19-mm range. This larger diameter philosophy provides for better centration and stability, even in those patients manifesting unusual topographies or graft tilt. Of course, larger diameters often require nontraditional optical zone and peripheral curve relationships.
Optical Zone Diameter:
GP optical zone diameters should be as large as possible to facilitate centration and minimize glare, but not so large as to result in harsh bearing, minimal movement, or lens adherence. In those situations, in which a large diameter (>10.5 mm) is necessary for lens centration and stability, a disproportionately small (<8.5 mm) optical zone diameter may be necessary to mitigate against a steep sagitta with attending tear stagnation.
Base Curve Radius:
A reasonable starting point for post-PK GP fitting is to select a base curve radius that straddles the keratometric measurements.14 Fluorescein evaluation is employed to refine the base curve radius to achieve a divided support fit. In recent years, corneal topography has been recommended as an alternate means for base curve radius selection. In this approach, the contact lens clinician selects the base curve radius based on the average dioptric
value at approximately 3 mm from the topography map’s center.15 When using this approach, it is prudent to select the dioptric value from sagittal maps. While spherical base curve radius GP lenses are still used in post-PK fitting, back surface low aspheric lenses represent the majority of designs in use today in those patients with atypical topographies. The back surface aspheric geometry provides for a smoother transition from lens center to edge, resulting in a more even fluorescein pattern. On rare occasions, a bitoric GP design is indicated. This design is usually reserved for those patients with significant amounts of regular astigmatism where the astigmatism is on the host as well as the graft, and for whom spherical or aspheric designs prove inadequate. Of course, the caveat for prescribing a bitoric is that the astigmatism must be regular and symmetric. If corneal topography reveals major meridians that are not orthogonal, a back surface toric is contraindicated. Likewise, a bitoric lens will not remain stable if the periphery of the lens does not land on a toric peripheral cornea. Therefore, in these cases, a nontoric base curve with a toric periphery should be considered.
value at approximately 3 mm from the topography map’s center.15 When using this approach, it is prudent to select the dioptric value from sagittal maps. While spherical base curve radius GP lenses are still used in post-PK fitting, back surface low aspheric lenses represent the majority of designs in use today in those patients with atypical topographies. The back surface aspheric geometry provides for a smoother transition from lens center to edge, resulting in a more even fluorescein pattern. On rare occasions, a bitoric GP design is indicated. This design is usually reserved for those patients with significant amounts of regular astigmatism where the astigmatism is on the host as well as the graft, and for whom spherical or aspheric designs prove inadequate. Of course, the caveat for prescribing a bitoric is that the astigmatism must be regular and symmetric. If corneal topography reveals major meridians that are not orthogonal, a back surface toric is contraindicated. Likewise, a bitoric lens will not remain stable if the periphery of the lens does not land on a toric peripheral cornea. Therefore, in these cases, a nontoric base curve with a toric periphery should be considered.
Peripheral Curve Systems:
There is no consistent relationship between lens base curve radius and peripheral curves in post-PK fitting. In most patients, peripheral curve radii and widths are secondary to overall diameter, optical zone diameter, and base curve radius in facilitating lens centration and movement. Occasionally, a very large diameter lens may result in peripheral lens binding, in which case a series of flatter and wider peripheral curves is warranted. Conversely, in a proud graft or plateau-type graft, a traditional peripheral curve system might result in excessive edge lift. In these cases, a bicurve (base curve and one peripheral curve) or even reverse geometry (secondary curve steeper than base curve) may be necessary. Fortunately, many GP laboratories have the ability to fabricate nontraditional peripheral curve systems.
Lens Thickness:
Consistent with our goals of maximizing oxygen transmission and minimizing lens mass, it is recommended to select the thinnest design possible. However, given the unusual topography and significant astigmatism associated with PK, clinicians must balance thinness with flexure and adherence resistance.
Fitting:
Corneal topography systems can aid in lens fitting. The newer topographers have been shown to evaluate a large enough area of the cornea for better visualization of the corneal shape.16 By analyzing the topography results, initial lens selection can be limited to only those designs that will seem most compatible with the corneal shape.
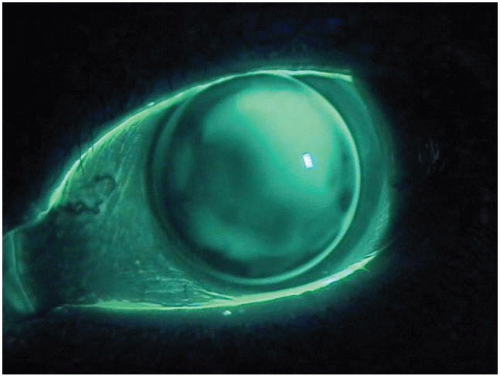
If the steepest area of the graft is inferior, a minus carrier lenticular or flatter posterior lens curvature may need to be incorporated into the lens design to aid in a lid attachment fit, as well as alignment in the flatter superior cornea. If the steep area of the graft is either nasal or temporal, a relatively successful option for lens stability is a larger overall diameter. A large overall diameter will aid in lens centration and pupillary coverage. Finally, if the steepest part of the graft is superior, increasing the mass of the lens with a prism ballast, high specific gravity lens, and/or a nonlenticular design can improve lens centration.17 The authors have had good success with an intralimbal design in PK fitting (Fig. 19.2).
Although GPs provide excellent astigmatism correction and physiologic response, occasionally, lens instability or intolerance will prevail. In this situation, the patient might be best served with a soft or hybrid contact lens.
Soft Contact Lenses
Although used less frequently, soft contact lenses (SCLs) offer certain distinct advantages. In those situations in which the patient manifests an atypical corneal topography or graft tilt, an SCL often provides much improved contact lens stability and comfort. Unfortunately, these patients can also manifest a significant amount of astigmatism, thereby necessitating spectacle overcorrection. Additionally, PK patients wearing SCLs must be more carefully monitored for corneal edema, neovascularization, infiltrates, and papillary conjunctivitis.
Lens Materials:
As is often the case in postsurgical contact lens endeavors, the clinician must balance oxygen transmission with acceptable surface characteristics. Over the past several years, silicone hydrogel lenses have shown good efficacy and safety as therapeutic lenses,18,19,20 and several have Food and Drug Administration (FDA) therapeutic approval. Bandage contact lenses are frequently used to splint compromised corneas. Oxygen is required to create the energy necessary for cellular division, synthesis of proteins and lipids, maintenance of pH/osmotic balance, and general repair. Irregular corneas can be extremely difficult to fit with silicone hydrogel lenses because of extreme curvature changes. Excessive movement, edge standoff, and fluting are common. Low oxygen transmission may stress an already compromised endothelium, whereas excessive movement may insult fragile or damaged epithelium. Silicone hydrogel madeto-order (MTO) lenses are customizable to both the fit and power needs of the patient, as well as maintaining a higher level of oxygen transmission.
Bandage contact lenses are frequently worn overnight during the healing process (see Chapter 11). Silicone hydrogel MTO lenses are currently only FDA approved for daily wear; prescribing overnight wear would be considered an off-label use. In some cases, overnight wear is unavoidable, such as in bullous keratopathy and other critical/sight-threatening diseases.18,19,20 Some corneas have a higher than average requirement for oxygen. In these patients, extended wear with silicone hydrogel lenses may have a potentially irreversible effect on corneal homeostasis. The doctor should consider the risks and benefits, and discuss the off-label use with the patient, before sending the patient out with extended wear silicone hydrogel MTO lenses.
Silicone hydrogel lenses have a stiffer modulus of rigidity. Unlike thin disposable hydrogel lenses, these stiffer lenses are more significantly affected by base curve, corneal diameter, peripheral asphericity, and overall sagittal height of the cornea. Surprisingly, however, many high plus or high minus patients switching from custom HEMA designs complain of increased floppiness with subsequent difficulty in handling the custom silicone hydrogel lenses.
While stock silicone hydrogel lenses are designed to fit the majority of patients, similar to the empirical fitting of disposable hydrogel lenses, silicone hydrogel MTO lenses are best fit through trial lenses to achieve optimal fitting characteristics and power determination. Complications, ranging from discomfort to superior arcuate lesion and giant papillary conjunctivitis, may be related to less than ideal fits.21 It is critical to select the appropriate diameter and base curve to ensure alignment to the cornea, especially in higher-power lenses, which tend to have even less flexibility. The base curve is selected after the diameter, since diameter will affect the overall sagittal depth of the contact lens. Flat lenses may not drape well on the cornea and can result in edge standoff and edge fluting. A steeper lens will typically be more comfortable; however, it may result in fluctuating vision if there is too much vault.
The lens should settle for a minimum of 10 minutes on the cornea to allow for osmotic equilibrium. Some patients may report mild lens awareness because of the stiff modulus of the lens.
This awareness is normal and generally quickly recedes. If the discomfort persists, it is important to check to make sure the lens is not inverted. The patient will also complain of discomfort if the lens is too flat and moves excessively; consider a larger, steeper lens in this case.
This awareness is normal and generally quickly recedes. If the discomfort persists, it is important to check to make sure the lens is not inverted. The patient will also complain of discomfort if the lens is too flat and moves excessively; consider a larger, steeper lens in this case.
The lens is evaluated for corneal coverage and lens movement. The lens should exhibit 0.2- to 0.3-mm movement and have good limbal coverage in all gazes. A silicone hydrogel lens should be fit slightly loose, compared to some HEMA-based lenses, to allow for tear exchange behind the lens. A tight lens will exhibit decreased tear exchange. Retention of debris, cells, and microorganisms has been implicated in the development of inflammatory and infectious adverse events.22
If the sagittal depth of the cornea (caused by either an unusual corneal diameter, large or small or a steep or flat base curve) does not match the sagittal depth of the lens, the edge of the lens will produce a gap. If a gap, or “fluting,” is present, the lens should not be dispensed since the lens will be uncomfortable because of lens edge awareness. In higher powers, a gap may induce cylinder across the entire lens, which will result in inadequate vision and challenging overrefractions.
Initial powers may be based on the patient’s vertexed spectacle prescription or the current HEMA contact lens. A slight modification in prescription after the patient wears the lens is expected. Silicone hydrogel MTO lenses have aspheric optics and are also affected by a lacrimal lens power; therefore, do not assume the patient’s current contact lens power will be optimal for a silicone hydrogel MTO lens. The power requirement for a silicone hydrogel MTO lens may be −0.25 to −0.50 D higher for myopic prescriptions and +0.25 to +0.50 D less for hyperopic prescriptions than the patient’s current contact lens power.
Lens Design:
Although clinicians have previously embraced the concept of prescribing standard thickness lenses to mask corneal astigmatism, there is very little evidence of this being practiced today with the advent of disposable lenses with high oxygen permeability (silicone hydrogels). Therefore, a thinner, more oxygen permeable design with adjunct spectacle overcorrection is preferable.
Certain PK patients may benefit from a toric SCL. This is acceptable if the patient achieves reasonable vision with a standard refraction, and does not manifest irregular astigmatism. A diagnostic lens fitting, overretinoscopy, and subjective overrefraction are mandatory to identify those patients who are destined to fail with this option. There are several silicone hydrogel toric lenses available today, including silicone hydrogel MTO lenses, with MTO toric lenses to be introduced in the very near future.
Piggyback Lenses
When a GP or SCL lens alone does not suffice, a combination of the two may be indicated. The concept of “piggybacking” a GP over an SCL has long been recognized as a niche application in specialty contact lens fitting. In this approach, an SCL is used for surface smoothing while the GP provides visual restoration.
Lens Materials:
The potential for hypoxia is significant when one considers the oxygen transmissibility limitations of each material as well as the barrier effect. Therefore, high Dk materials should be routinely prescribed. This would include a silicone hydrogel soft lens and a hyper Dk GP lens material. During lens adaptation, the clinician must monitor corneal health and adjust wearing time accordingly.
Lens Design:
SCL selection should be governed by each patient’s prescription and topography. Piggybacking is an area where silicone hydrogels have substantial benefits, since a double lens system further reduces the oxygen flux to the cornea. However, daily disposable lenses offer substantial convenience and cleanliness. The power of the piggyback contact lens can be used to alter the fit of the GP lens. A plus lens will “steepen” the base curve of the eye. This creates a more prolate
surface and is beneficial for a postsurgical/oblate cornea where centration of a GP lens may be difficult. Patients who manifest a “sunken” or plateau graft are best served by a moderate plus lens, thus addressing the anticipated need for hyperopic correction and providing an apex on which to center the GP. It can also be used with an existing GP fit to create a flatter lens-to-surface relationship, thereby “loosening” the GP lens. This is particularly beneficial in cases of a “proud” or steep graft. A myopic prescription will create a less prolate surface, useful, for example, on keratoconic patients, who are highly prolate. It will also “steepen” the lens-to-cornea relationship, effectively creating a “tighter” fit. In either of these situations, the value of incorporating a portion of the refractive power into the SCL lessens the thickness of the overlying GP.
surface and is beneficial for a postsurgical/oblate cornea where centration of a GP lens may be difficult. Patients who manifest a “sunken” or plateau graft are best served by a moderate plus lens, thus addressing the anticipated need for hyperopic correction and providing an apex on which to center the GP. It can also be used with an existing GP fit to create a flatter lens-to-surface relationship, thereby “loosening” the GP lens. This is particularly beneficial in cases of a “proud” or steep graft. A myopic prescription will create a less prolate surface, useful, for example, on keratoconic patients, who are highly prolate. It will also “steepen” the lens-to-cornea relationship, effectively creating a “tighter” fit. In either of these situations, the value of incorporating a portion of the refractive power into the SCL lessens the thickness of the overlying GP.
The underlying SCL should be fit to center well and demonstrate optimal to excessive movement. Excessive movement is critical, as the GP will inevitably lessen SCL movement. Once a satisfactory SCL fit is obtained, over-keratometry is performed and serves as a starting point for GP selection. Averaging flat and steep keratometry is a good starting point for base curve radius selection or using the best fit sphere from the topographer. Final base curve radius, overall diameter, optical zone diameter, peripheral curve radii and widths, and power are determined by diagnostic fitting. High molecular weight sodium fluoride can be used to assess the GP-SCL relationship. The clinician should be careful to avoid a tightly fit GP, as this often traps interfacial debris. In the case where the GP is fit before piggybacking, an SCL can be added to increase lens comfort and wearing time or incorporate small refractive changes. It is imperative that the GP-SCL relationship remain as described above in both fitting scenarios.
It is generally accepted that any complication that occurs with either an SCL or a GP can develop with a piggyback combination. This is not entirely true, as GP peripheral corneal staining does not occur with piggyback combinations. However, papillary conjunctivitis, corneal edema, neovascularization, lens adherence, acute red eye, infiltrates, infection, and graft rejection can result from piggyback lens applications.
An SCL specifically designed for piggyback applications has been available for several years. Marketed as Flexlens Piggyback Lens (X-Cel Contacts), this midwater SCL lens has a partial thickness insert cut out of the center. The Flexlens concept allows for the GP to be fit within the “cut-out,” thereby facilitating centration. However, this lens has a low oxygen permeability, increasing the likelihood for corneal edema to occur, which should be taken into consideration before fitting.
Hybrid Lenses
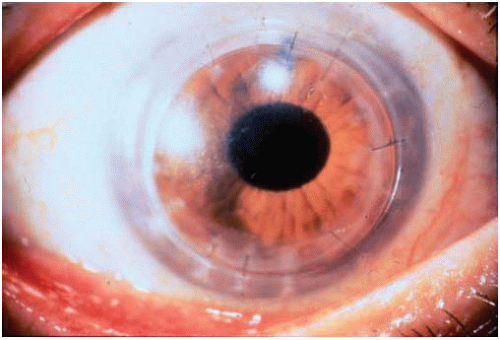
A relatively new entry in PK management involves the use of a hybrid design. This design fuses a GP center with an SCL skirt in an effort to provide good comfort and vision. Because of performance limitations (i.e., poor fitting characteristics, limited oxygen transmission, tearing at rigid-soft lens junction), the previous hybrid lens SoftPerm (Ciba Vision) is not regularly utilized. However, a new hybrid lens, SynergEyes, has recently entered the market. SynergEyes has an F-S/A center with a Dk of 100 (i.e., Paragon HDS100, Paragon Vision Sciences) and a poly-HEMA hydrophilic skirt (Fig. 19.3).
The SynergEyes lens has been found to allow significantly more oxygen to reach the cornea during wear than the SoftPerm lens at the central cornea, as well as 2.0 mm and 4.5 mm temporal to the central cornea.23 The larger overall diameter, larger central optical zone, and GP peripheral curve provide a wider range of applications for the hybrid lens. Most recently, the SynergEyes PS lens has been introduced. This specific design is recommended for oblate corneas resulting from postrefractive surgery, ocular trauma, and postpenetrating keratoplasty.
Considerable debate exists regarding the risks and benefits of hybrid lenses in PK management. Lens adherence is relatively common and can result in corneal edema, neovascularization, epithelial erosion, acute red eye, infiltrative keratitis, and graft rejection. In addition, this lens can be difficult to handle; therefore, it is best inserted using the forefinger and the middle finger to cradle the lens. Likewise, although tearing at the GP-SCL junction is not as common as it is with
the SoftPerm lens, it is still recommended to push the lens onto the conjunctiva (where it is less adherent) before pinching it off of the eye. However, hybrid lenses offer excellent centration and stability as well as moderate astigmatism correction and provide an option for patients who experience discomfort or a poor lens-to-cornea fitting relationship with a GP lens. Our experiences with SynergEyes have been generally favorable; however, peripheral corneal/limbal compression accompanied by trapped debris can result in inflammatory events if the lens tightens over time. Therefore, certain precautions must be taken. The proper base curve selection is determined by diagnostic fitting, with each trial lens allowed to equilibrate for at least 15 minutes. Regardless of a good visual response and positive patient acceptance, adequate lens movement is essential.
the SoftPerm lens, it is still recommended to push the lens onto the conjunctiva (where it is less adherent) before pinching it off of the eye. However, hybrid lenses offer excellent centration and stability as well as moderate astigmatism correction and provide an option for patients who experience discomfort or a poor lens-to-cornea fitting relationship with a GP lens. Our experiences with SynergEyes have been generally favorable; however, peripheral corneal/limbal compression accompanied by trapped debris can result in inflammatory events if the lens tightens over time. Therefore, certain precautions must be taken. The proper base curve selection is determined by diagnostic fitting, with each trial lens allowed to equilibrate for at least 15 minutes. Regardless of a good visual response and positive patient acceptance, adequate lens movement is essential.
▪ RADIAL KERATOTOMY
Once the predominant mode of refractive surgery, RK has been relegated to a secondary status because of the widespread popularity of excimer laser-based procedures. At its height, RK was performed on approximately 250,000 Americans annually.24 Although deemed relatively safe and effective by the Prospective Evaluation of Radial Keratotomy (PERK) study, RK has nonetheless been recognized for significant shortcomings.25 Of primary concern is the incidence of residual refractive error, irregular astigmatism, diurnal fluctuations, progressive hyperopia, and glare.
Contact Lens Rationale
Although some patient symptoms are effectively managed by intermittent spectacle lens wear, many are best suited for contact lens wear. Once used regularly to address procedure-related micro- and macroperforations as well as persistent epithelial defects, bandage contact lenses are rarely used today. Refinement in surgical techniques, improved instrumentation, and the use of nonsteroidal anti-inflammatory drugs (NSAIDs) postoperatively have significantly lessened the need for bandage lenses. Occasionally, however, bandage lenses are employed to modulate refractive outcome. In those patients who are initially undercorrected, a bandage lens may be beneficial.26 When worn on an extended wear basis, a bandage lens can increase peripheral corneal edema, spread the RK incisions, and possibly enhance the myopic effect. This strategy, however, is not without risk. The patient must be closely monitored for neovascularization, epithelial erosion, and signs of infiltrative keratitis.
Special Considerations
As is true of any corneal surgical procedure, RK can profoundly alter structure and function. Certainly, the topographic changes can provide a compelling argument for prescribing contact lenses. Conversely, the anatomic and physiologic alterations make contact lenses a riskier
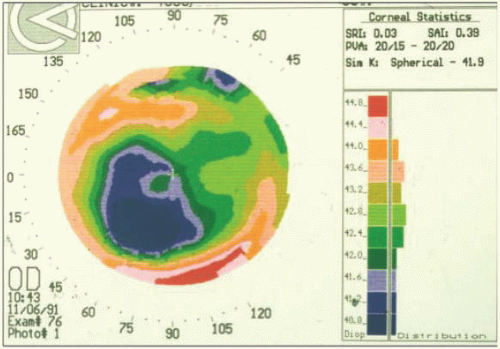
endeavor. The topographic changes can both support clinical suspicion as well as provide insight into contact lens fitting. Indeed, the idea of RK is to surgically induce a central corneal flattening accompanied by myopia reduction. Unfortunately, the degree of flattening is sometimes unpredictable and radially asymmetric. The net effect is residual myopia, unanticipated hyperopia, or induced astigmatism. Additionally, the post-RK topography can be complicated by an optical zone decentration (Fig. 19.4). Optical zone decentration has been associated with diurnal visual fluctuation and can complicate contact lens fitting, as the corneal apex is no longer centered.
endeavor. The topographic changes can both support clinical suspicion as well as provide insight into contact lens fitting. Indeed, the idea of RK is to surgically induce a central corneal flattening accompanied by myopia reduction. Unfortunately, the degree of flattening is sometimes unpredictable and radially asymmetric. The net effect is residual myopia, unanticipated hyperopia, or induced astigmatism. Additionally, the post-RK topography can be complicated by an optical zone decentration (Fig. 19.4). Optical zone decentration has been associated with diurnal visual fluctuation and can complicate contact lens fitting, as the corneal apex is no longer centered.
The anatomic and physiologic changes associated with RK can be as challenging as the topographic alterations. The success of RK is, at minimum, partially because of the way in which the cornea heals. Initially, epithelial swelling is followed by hyperplasia into the wound margin. This epithelial “plug” interferes with normal stromal architecture, resulting in the desired flattening. Unfortunately, it is this epithelial “plug” that places the RK patient at greater risk while wearing contact lenses. Indeed, even after the RK incision has healed, it is more susceptible to neovascularization, epithelial erosion, and infiltrative keratitis. Finally, the RK incision often violates endothelial integrity. Fortunately, endothelial cell loss secondary to RK is often limited to the incision sight and is not widespread. However, the potential for endothelial cell loss underscores the importance of optimizing oxygen transmission.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree