Chapter 50 Postoperative Management of Differentiated Thyroid Cancer
![]() This chapter contains additional online-only content, available on expertconsult.com.
This chapter contains additional online-only content, available on expertconsult.com.
Thyroid tumors are the most common endocrine neoplasms. The treatment of a patient with differentiated thyroid cancer usually consists of surgical resection, followed by medical therapy and regular follow-up. In the following discussion, we review the features of differentiated thyroid carcinomas and the consensus and controversies in their management, based on recent guidelines.1
Classification of Thyroid Tumors
Histologic Classification
Lesions of follicular cell origin constitute more than 95% of thyroid cancers and are classified into papillary, follicular, poorly differentiated, and anaplastic carcinomas.2,3 The remainder of thyroid cancers is largely made up of tumors exhibiting C-cell differentiation. Nonepithelial thyroid tumors are rare and mainly include malignant lymphomas, true sarcomas, and malignant hemangioendotheliomas. Finally, blood-borne metastases to the thyroid may in rare cases cause clinically detectable thyroid enlargement.
Staging of Thyroid Carcinoma
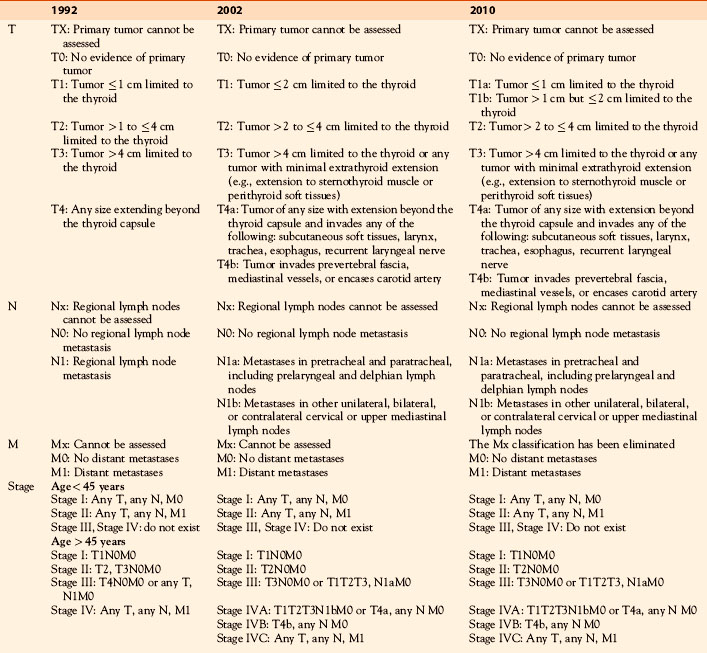
The International Union Against Cancer (UICC) and the American Joint Committee on Cancer (AJCC) have agreed on a staging system in thyroid cancer.4,5 As stated by the AJCC, “the principal purpose served by international agreement on the classification of cancer cases by extent of disease was to provide a method of conveying clinical experience to others without ambiguity.” The AJCC is based on the TNM system, which relies on assessing three components: (1) the extent of the primary tumor (T), (2) the absence or presence of regional lymph node metastases (N), and (3) the absence or presence of distant metastases (M). The TNM system allows a reasonably precise description and recording of the anatomic extent of disease and provides a reliable estimate of the risk of dying from thyroid cancer, not necessarily risk of recurrence. With the pathologic classification (pTNM) that is based on surgical pathology data, a precise size can be assigned to the primary tumor, extrathyroid invasion is demonstrated, and the histology is unequivocally identified.
A previous classification dating back to 1992, the primary thyroid tumor (T) status was defined according to the size of the primary lesion: T1, greatest diameter 1 cm or smaller; T2, larger than 1 cm but not larger than 4 cm; T3, larger than 4 cm; T4, direct (extrathyroidal) extension beyond the thyroid capsule.4 The 2002 TNM classification extended the T1 group to include tumors no larger than 2 cm,5 and distinguished between T4a (theoretically resectable) and T4b (unresectable) tumors, for which treatment options and prognosis differ. The most recent TNM classification, published in 2010, defines microcarcinomas as not larger than 1 cm, now classified as T1a, from other small tumors, larger than 1 cm but no larger than 2 cm, now classified as T1b.6 This distinction is based on the excellent prognosis of microcarcinoma and on recent data showing that microcarcinoma may be treated with lobectomy or total thyroidectomy with no difference in prognosis, whereas for tumors larger than 1 cm, lobectomy seems to convey a higher risk of recurrence and mortality.8,9 The most recent classification also subdivides T categories into Ts, solitary tumors, and Tm, multifocal tumors, with the largest tumor focus determining the numerical level of the T stage (the sizes of the foci are not added together).
The classification of regional disease has remained the same over the years, distinguishing only N0 and N1, because of the low impact of nodal disease on overall prognosis. For pathologic N staging, ordinarily six lymph nodes should be found at pathology to qualify for the definition of N0 (although there are few data on central compartment neck dissection supporting this number) and even for smaller number of nodes removed, the pN0 classification still holds. In addition, the prognostic difference between central lymph node metastases and other regional metastases (Na versus Nb) has yet to be validated. In one study, for example, the risk of persistent or recurrent disease appeared to be related to the involvement of the central neck compartment, the number of involved lymph nodes, and the number of lymph nodes with extracapsular spread.7 Currently, it is not possible to ascertain whether the modifications included in the 2010 TNM classification will significantly improve its prognostic value or will have a clinical impact on therapeutic strategies.
For purposes of analysis, TNM stage-groups have been described (Table 50-1). The age of the patient is included because of its importance in predicting the behavior and prognosis of thyroid cancer. The stage grouping has not changed from the 2002 classification. According to this staging classification, all patients younger than age 45 years are in stage I, unless they have distant metastases, in which case they are in stage II. Stages III and IV do not exist in this age group. In young patients and especially in children, however, the risk of recurrence is high and may be underestimated by the TNM staging system. For older patients (age 45 years or more) the tumor and node stages have a larger effect on prognosis, most likely in part because of the tumor behavior in this age group. Patients with widespread nodal disease are in stage IVA.
Papillary Thyroid Carcinoma (PTC)
![]() Please see the Expert Consult website for more discussion of this topic.
Please see the Expert Consult website for more discussion of this topic.
The incidence rates of thyroid carcinomas in the United States have increased from 3.6 per 100,000 in 1973 to 8.7 per 100,000 in 2002. This trend appears to be continuing10 and has been reported in most industrialized countries. Almost the entire change has been attributed to an increased incidence of papillary thyroid cancer, and 87% of the rising incidence consisted of cancers measuring 2 cm or smaller. The apparent increasing incidence of thyroid carcinomas may be caused by the more extensive use of neck ultrasonography and early diagnosis and treatment with diagnosis of smaller and smaller tumors,11 but other factors may also be involved.
Clinical History
Although PTCs can occur at any age, most occur in patients between 30 and 50 years of age (mean age, 45 years).12,13 Women are affected more frequently (female predominance, 60% to 80%). Most primary tumors are 1 to 4 cm in size. PTC is frequently multifocal when it occurs in a single lobe, and it is bilateral in 20% to 80% of cases, depending on whether or not the thyroid was meticulously examined. Extrathyroidal invasion of adjacent soft tissues is present in about 15% (range 5% to 34%) at primary surgery, and about one third of PTC patients have clinically or ultrasonographically evident lymphadenopathy at presentation. About 35% to 50% of excised neck nodes have histologic evidence of involvement, and in children nodal involvement may be present in up to 90%. Only 1% to 7% of PTC patients have distant metastases (DM) at diagnosis. Spread to mediastinal nodes is usually associated with extensive nodal involvement in the neck.
Only a fraction (~ 15%) of patients with PTC are likely to experience relapse of disease, which is located in the neck for three fourths of these patients, and more frequently in lymph nodes than in the thyroid bed or in soft tissue; 80% of recurrences occur during the 5 first years of follow-up. Even fewer patients (~ 5%) have a lethal outcome. Among those with lethal PTC, 20% of deaths occur in the first year after diagnosis, and 80% of the deaths occur within 10 years.12–16
Cox model analysis and stepwise variable selection has led to a final prognostic model that includes five variables: distant metastases (DM), age, completeness of resection, local invasion, and size (MACIS). The final score is calculated as follows: 3.1 (if age 39 years or younger) or 0.08 (if age 40 years or older) × age + 0.3 × tumor size (in centimeters) + 1 (if tumor not completely resected) + 1 (if locally invasive) + 3 (if DM are present). The MACIS scoring system permits identification of groups of patients with different risks of dying from PTC. Twenty-year cause-specific survival rates for patients with MACIS scores of less than 6, 6 to 6.99, 7 to 7.99, and 8 + were 99%, 89%, 56%, and 27%, respectively (p < .0001). When cumulative mortality from all causes of death was considered, approximately 85% of PTC patients with MACIS scores below 6 had no excess mortality over rates predicted for control subjects in the general population.13
Follicular Thyroid Carcinoma (FTC)
FTC is “a malignant epithelial tumor showing evidence of follicular cell differentiation but lacking the diagnostic features of papillary carcinoma.”2,3 FTC is a relatively rare neoplasm whose identification requires invasion of the capsule of the tumor or blood vessel invasion (see Chapter 20, Follicular Thyroid Cancer). In epidemiologic studies, FTC represented 5% to 50% of differentiated thyroid cancers and was more common in areas with iodine deficiency. Owing to a combination of changing diagnostic criteria and an increase in the incidence of PTC associated with dietary iodine supplementation, the diagnosis of FTC has decreased in frequency.
![]() Please see the Expert Consult website for more discussion of this topic.
Please see the Expert Consult website for more discussion of this topic.
The microscopic appearance of FTC varies from well-formed follicles to a predominantly solid growth pattern. FTC is best divided on the basis of degree of invasiveness into minimally invasive and widely invasive. There is little overlap between these two types. Minimally invasive FTC is an encapsulated tumor whose growth pattern resembles that of a trabecular or solid, microfollicular, or atypical adenoma. The diagnosis of malignancy depends on the demonstration of blood vessel, capsular invasion, or both. The criteria for invasion must therefore be strict. Blood vessel invasion is almost never seen grossly. Microscopically, the vessels “should be of venous caliber, be located in or immediately outside of the capsule and contain one or more clusters of tumor cells attached to the wall and protruding into the lumen.”2 Interruption of the capsule must involve the full thickness of the capsule to qualify as capsular invasion. The diagnosis of malignancy of these tumors may be difficult and not reproducible among pathologists. Immunohistochemistry with markers such as TPO, Galectin 3, or HMBE1 may help for this purpose, but these techniques do not reliably improve the accuracy of pathology in case of suspicious findings. Global gene expression studies with microarray technology demonstrate different profiles between papillary carcinoma and follicular tumors, but the reported distinction between follicular adenomas and minimally invasive follicular carcinoma with the expression study of a limited number of genes needs confirmation. In contrast, the rare widely invasive form of FTC can be distinguished easily from benign lesions. Although the tumor may be partially encapsulated, the margins are infiltrative even on gross examination and vascular invasion is often extensive. The structural features are variable, but a follicular element is always present. When follicular differentiation is poor or absent, or in the presence of trabecular, insular, or solid components, the tumor is classified as a poorly differentiated carcinoma.17
Focal or extensive clear-cell changes can occur. A rare clear-cell variant of FTC has been described in which glycogen accumulation or dilatation of the granular endoplasmic reticulum is responsible for the clear cells. When more than 75% of cells in an FTC exhibit Hurthle cell (or oncocytic) features, the tumor is classified as a Hurthle cell (HCC) or an oncocytic carcinoma or an oxyphilic variant FTC.2,3
Natural History
FTC tends to occur in older people, with a mean age of over 50, increasing to 60 years for oxyphilic FTC. As in most thyroid malignancies, women outnumber men by more than 2 to 1. Most patients with FTC present with a painless thyroid nodule, with or without background thyroid nodularity. Lymph node metastases to the neck in FTC are so rare that “wherever they are observed, the alternative possibilities of follicular variant papillary carcinoma, oncocytic carcinoma, and poorly differentiated carcinoma should be considered.”3
The nodal recurrence rate for FTC is the lowest for any differentiated thyroid carcinoma, being around 2% at 20 postoperative years, and is higher in patients with Hurthle cell carcinoma, increasing to approximately 15%. Local recurrences at 20 years occur in approximately 20% of FTCs and 30% of Hurthle cell carcinomas, and DM rates are around 25%. The death rates tend to parallel the curves for development of DM, and cause-specific survival rates approximate 80% at 20 postoperative years.18,19
The risk factors that predict outcome in FTC are largely the same as in PTC: increasing age of the patient, DM at presentation, large tumor size, and the presence of local (extrathyroidal) invasion. The pTNM risk group categorization has proved to be useful in FTC. In addition, vascular invasiveness, lymphatic involvement at presentation, DNA aneuploidy, and oxyphilic histology are potential prognostic variables unique to FTC. The importance of vascular invasion is underscored by a study showing that FTC patients with minimal capsular invasion and no evidence of vascular invasion had 0% cause-specific mortality at 10-years of follow-up.20
Poorly Differentiated Carcinoma
A recent study has proposed new diagnostic criteria for poorly differentiated carcinoma17: (1) solid, trabecular, and insular pattern of growth; (2) absence of the conventional nuclear features of papillary carcinomas; (3) presence of at least convoluted nuclei, mitotic activity > 3 × 10 HPF, and tumor necrosis. Most such tumors are larger than 5 cm in diameter at diagnosis, with extrathyroidal extension and blood vessel invasion. The mean age at diagnosis is around 55 years, and the female/male ratio is approximately 2:1. Poorly differentiated carcinoma is aggressive, with frequent neck recurrence and distant metastases in bones and lungs, and it is often lethal. Radioiodine uptake is rarely present, and FDG uptake on positron emission tomography (PET) scan is frequently high. Production of Tg can be demonstrated by immunohistochemistry, but its detection in blood tests may be lower than for differentiated carcinomas. In one series, 56% of patients died from their tumor within 8 years of initial therapy.21
Surgical Treatment of Thyroid Carcinoma
![]() Please see the Expert Consult website for more discussion of this topic.
Please see the Expert Consult website for more discussion of this topic.
Surgical Treatment of Thyroid Carcinoma
Factors that influence the optimal extent of surgery include the histologic diagnosis, the size of the original lesion, the presence of lymph node and distant metastases, and the patient’s age (see Chapter 30, Principles in Thyroid Surgery). Obviously, the surgeon and the surgical team must be appropriately skilled in thyroid surgery, and the goal of surgery should be to remove all the malignant neoplastic tissue present in the neck. Therefore, a preoperative ultrasound examination of the thyroid gland and of neck lymph node areas should be routinely performed, and detected lesions be adequately resected.1
In the case of PTC and FTC, total thyroidectomy is recommended for the majority of patients.1 Total thyroidectomy reduces the recurrence rate,8,9 compared with more limited surgery, possibly because many PTCs are both multifocal and bilateral. Removal of all of the thyroid gland facilitates postoperative remnant ablation with 131I and follow-up with serum thyroglobulin.
For extremely low-risk patients (i.e., those with unifocal and intrathyroidal papillary thyroid microcarcinoma, < 1 cm in diameter), a lobectomy may be an appropriate primary surgical procedure.1 A completion thyroidectomy should be offered to patients who have undergone a unilateral lobectomy for a supposedly benign tumor that proves to be a cancer and for whom a total thyroidectomy would have been recommended had the diagnosis been available before the initial surgery.1 This includes all patients with thyroid cancer except those with unifocal and intrathyroidal micro PTC.
In the absence of metastatic nodes detected clinically or ultrasonographically, a prophylactic or elective dissection of the central compartment is still controversial and may be performed, especially for larger, higher-risk tumors (T3, T4).1 Although prophylactic lymph node dissection has not been shown to improve the recurrence or survival rates, several arguments support its routine use in patients with papillary carcinomas. These include the fact that histologic evidence of lymph node metastases is present in up to two thirds of PTC patients, of whom more than 80% have involvement of the central compartment. Lymph node metastases are difficult to detect by palpation or by ultrasound in lymph nodes located behind the great vessels or in the paratracheal groove, and preoperative neck ultrasound detects only half of involved lymph nodes. The knowledge of initial lymph node status is a requisite for TNM classification, is useful for tailoring indications of postsurgical radioiodine administration,22 and helps in the interpretation of any abnormality in the neck identified during the subsequent postoperative follow-up. The major drawback of adding prophylactic lymph node dissection to total thyroidectomy is that it may increase the morbidity rate. Therefore, it may be best performed by high-volume surgeons.
In recommending surgery, the endocrinologist should discuss potential operative complications with the patient. Unilateral lobectomy virtually never causes permanent hypocalcemia but can cause temporary vocal cord paralysis in as many as 3% of patients. Total thyroidectomy causes temporary hypocalcemia in 7% to 10% of patients and permanent hypocalcemia in 0.5% to 1%. The risk of hypoparathyroidism should be reduced by identifying parathyroid glands, possibly aided by intraoperative intravenous methylene blue administration and certainly, if viability is in doubt, by autotransplanting the parathyroid glands. The experience of the surgeon is important in terms of minimizing morbidity such as vocal cord paralysis and in terms of the finer technical points of thyroidectomy, including preservation of the external branch of the superior laryngeal nerve, which is involved in the fine regulation of voice pitch. Permanent vocal cord paralysis in expert series occurs in less than 1% of patients but may severely affect quality of life. Specific treatment of this complication with different types of laryngeal surgeries (vocal fold medialization thyroplasty, intracordal injection of autologous or synthetic materials, or other techniques) significantly improves voice and quality of life, and patients should be referred to a specialist in this type of laryngeal surgery for management.23
Postoperative Management
Iodine 131 Therapy
131I is an effective agent for delivering high radiation doses to the thyroid tissue with low spillover to other portions of the body. The radiation dose to the thyroid tissue is related to the tissue concentration of iodine, the ratio between the total tissue uptake and the volume of functional tissue, and the effective half-life of 131I in the tissue. Thyroid tissue is able to concentrate iodine only after thyroid-stimulating hormone (TSH) stimulation, but even after optimal TSH stimulation, iodine uptake in neoplastic tissue is always lower than in normal thyroid tissue and may not be detectable in about one third of cases (see Chapter 51, Postoperative Radioactive Iodine Ablation and Treatment of Differentiated Thyroid Cancer).24
131I therapy is a complement to total thyroidectomy in selected patients and should not be considered as a therapeutic means to justify incomplete and insufficient surgery. It is given postoperatively for three reasons. First, it destroys normal thyroid remnants (this is termed ablation), thereby increasing the sensitivity of subsequent 131I total-body scanning and the specificity of measurements of serum Tg for the detection of persistent or recurrent disease. Second, it may destroy occult or known microscopic carcinoma, thereby potentially decreasing the long-term recurrence rate. Finally, it makes it possible to perform a postablative 131I total-body scan, a sensitive tool for detecting persistent carcinoma.1,25
Postoperative 131I therapy should be used selectively, and not all patients with a diagnosis of follicular cell–derived thyroid carcinoma benefit from routine postoperative radioiodine therapy. In very low risk patients, the long-term prognosis after surgery alone is so favorable that 131I ablation is not recommended. Routine prophylactic lymph node dissection in all PTC patients also permits selected T1N0 patients to avoid radioiodine administration.22 However, patients with persistent disease and those who are at high risk of recurrence (Table 50-2) are routinely treated with 131I because such therapy can potentially decrease both recurrence and death rates. Young children are also usually candidates for postoperative radioiodine therapy because they may have extensive neck lymph node involvement and in such case frequently harbor pulmonary metastases that may not be detectable with standard radiographs or even with computed tomography (CT) imaging of the chest. Finally, in the other patients, there is currently no evidence that it may improve the long-term outcome, especially if surgery has been complete.
Table 50-2 Indications for 131I Treatment in Patients with Papillary, Follicular, or Hurthle Cell Thyroid Carcinoma after Initial Definitive Near-Total Thyroidectomy
| Very low risk patients: T< 1 cm, unifocal, intrathyroid, and N0: |
| High-risk patients: T2-4, extensive N1, M1, PTC patients with MACIS scores of 6+, or any thyroid cancer patient with incompletely resected disease: |
| Low-risk patients: all the other patients |
FTC, follicular thyroid carcinoma; HCC, Hurthle cell carcinoma; MACIS, metastasis, age, completeness of resection, invasion, and size; PTC, papillary thyroid carcinoma; pTNM, pathologic-tumor-node-metastasis; Tg, thyroglobulin.
Postoperatively, no levothyroxine (LT4) treatment is given for 4 to 6 weeks, but triiodothyronine (LT3) can be substituted for at least 3 to 4 weeks and then discontinued for 2 weeks before radioiodine studies. At that time, the serum TSH level should be greater than an empirically determined level of 25 to 30 mU/L. At this level of TSH, an undetectable serum Tg level indicates a very low risk of finding of persistent disease or subsequent recurrence.25 Intramuscular injections of rhTSH (0.9 mg for 2 consecutive days, with 131I administered 1 day after the second injection) given while continuing LT4 treatment may achieve an effective stimulation of radioiodine uptake by normal thyroid remnants, with ablation rates similar to those obtained with withdrawal.27 Its use prevents hypothyroidism and maintains quality of life, induces a lower radiation exposure to the body, and permits an earlier discharge from the hospital.28,29 In addition, short-term recurrence rates have been found to be similar in patients prepared with thyroid hormone withdrawal or rhTSH, even in those with initial lymph node involvement.30 rhTSH is approved for remnant ablation in the United States, Europe, and many other countries around the world.
In case of an incomplete thyroidectomy, neck uptake may be measured with a tracer activity of 131I or 123I, but the activity used should be small enough to avoid stunning—that is, a decrease of thyroid uptake with the subsequent high activity of radioiodine—that is possibly due to a decrease in NIS (sodium/iodide symporter) expression in irradiated cells.31,32 High uptake (> 10%) and high risk of persistent disease should lead to completion surgery. 131I therapy can be administered to patients for whom surgery can be considered complete, with no such pretherapy scanning because of its low impact on the decision to ablate, because of concerns over 131I-induced stunning, and because usually 24-hour uptakes are considerably less than 10%.33
A total body scan is performed 3 to 7 days after the treatment activity and is highly informative in patients with a low uptake (< 1%) in the thyroid bed. Additional metastatic foci have been reported in 10% to 26% of patients scanned following high-dose radioiodine treatment as compared with the diagnostic scan. 131I single-photon emission computed tomography (SPECT)/CT fusion imaging may provide superior lesion localization after remnant ablation.34,35
Total ablation (defined as no visible uptake) may be verified by a 131I total-body scan 6 to 12 months later, typically with 2 to 5 mCi (74 to 185 MBq). However, a follow-up 131I total body scan is no longer routinely performed when the postablation scan has been informative (low uptake of remnants only), because it does not afford any further information as to prognosis.36 Successful ablation is currently defined as an undetectable serum Tg level following rhTSH stimulation and a normal neck ultrasonography, usually performed 9 to 12 months after ablation.1,25 Total ablation is achieved after the administration of either 100 mCi (3700 MBq) or 30 mCi (1100 MBq) in more than 80% of patients who had at least a near-total thyroidectomy, after preparation with either withdrawal or rhTSH.37 After less extensive surgery, ablation is achieved in only two thirds of patients with 30 mCi (1100 MBq). Therefore, a near-total or total thyroidectomy should be performed in all patients who are to be treated with 131I. In addition, in high-risk patients, a high activity (100 mCi or more) should be administered with the aims of ablating normal thyroid remnants and irradiating residual neoplastic tissue. Total ablation requires that a dose of at least 300 Gy (30,000 rad) be delivered to thyroid remnants.38 In certain cases, dosimetric study can allow a more precise estimate of the 131I dose to be administered while avoiding the administration of excessive activities.39
External Beam Radiation Therapy
External beam radiation therapy to the neck and mediastinum is indicated only for older patients (> 45 years) with extensive PTC in whom complete surgical excision is impossible and in whom the tumor tissue does not take up 131I (see Chapter 52, External Beam Radiotherapy for Thyroid Malignancy).40,41 Retrospective studies have shown that in these selected patients, radiotherapy decreases the risk of neck recurrence. The target volume encompasses the thyroid bed, bilateral neck lymph node areas, and the upper part of the mediastinum. Typically, 50 Gy (5000 rad) are delivered in 25 fractions over 5 weeks, with a boost of 5 to 10 Gy applied to any residual macroscopic focus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree