Fig. 38.1
The typical appearance of “adenoid facies” with increased anterior facial height, narrow facial width, open-mouthed posture, and an incompetent and short upper lip. However, these facial features are not always diagnostic of the respiratory pattern since patients who breathe with their lips separated may actually be oral-nasal or nasal breathers as well as oral breathers

Fig. 38.2
The typical pinched nose appearance in a mouth-breathing patient

Fig. 38.3
Sagittal occlusal relationship in mouth-breathing patients is said to include a Class II molar occlusion with increased overjet and protruding maxillary anterior teeth

Fig. 38.4
A posterior crossbite and an anterior open-bite malocclusion in a mouth-breathing patient. The posterior crossbite is suggested to be due to transverse maxillary deficiency caused by an imbalance of forces between the muscle forces acting on these structures. The open bite is caused by extruded molar teeth due to an open-mouthed posture in response to an increased nasal resistance

Fig. 38.5
The V-shaped maxillary arch with deep palatal vault

Fig. 38.6
The extended head position of a mouth-breathing child. Necessity of airway maintenance dictates the head and neck posture in these patients
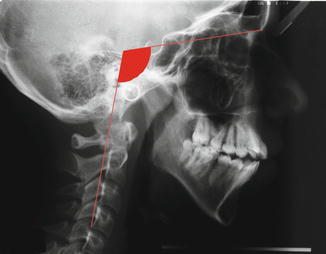
Fig. 38.7
Lateral cephalometric radiograph of the patient in Fig. 38.6. Note the dental protrusion and downward-backward rotation of the mandible in addition to the extended head position
Despite many attempts to establish a cause-and-effect relationship between nasal respiratory impairments and dentofacial deformities, the issue is still controversial within orthodontics and otolaryngology. The most prevalent view among clinicians is that a change in the mode of respiration, such as mouth breathing due to an inadequate nasal airway, could cause changes in craniocervical posture, maxillomandibular relationship, and position of the tongue. This in turn could affect dentofacial growth and positions of the teeth. However, clinicians from both sides of controversy can find ample evidence in the literature supporting their opinions, and the results of studies relating dentofacial features with respiratory pattern are far from being conclusive.
Since there are treatment decisions that revolve around the degree of interplay between nasal obstruction and dentofacial development, the relationship must be further elucidated. If nasal obstruction has an effect on dentofacial development, early treatment for removal of the cause of this obstruction would be necessary. On the other hand, if dentofacial growth and development is not significantly affected by the respiratory mode, then treatment of nasal obstruction in order to prevent abnormal orofacial development would not be indicated.
In this chapter, we examine the possible interactions among respiratory mode and dentofacial growth and development by reviewing both sides of the controversy with special emphasis on questions such as:
Does impaired nasal breathing always result in complete mouth breathing with possible negative effects for the dentofacial complex?
What are the effects of mouth breathing on craniocervical posture, maxillomandibular relationships, facial morphology, tongue position, and occlusal features?
Does reversing the mode of respiration from oral to nasal allow proper growth and of craniofacial and dentofacial complex?
Do orthodontic treatment mechanics have a role in normalizing the breathing pattern?
38.2 Respiratory Pattern
The relationship between mouth breathing and dentofacial growth is still being debated after more than a century. Despite the existence of an extensive body of literature on this subject, the inconclusive results so far may be explained by different population selection criteria and the various diagnostic methods used for differentiating mouth breathers from nasal breathers. In order to determine this assumed relationship, the meaning of the term mouth breathing needs to be clearly established.
Human neonates are obligatory nasal breathers (Moss 1965). After birth, the maintenance of airway by correct posturing of the mandible and the tongue is necessary for survival. James and Hastings (1932) examined 53 infants, aged from 1 to 14 days, and found that most of the infants in their study with lips-apart posture achieved an oral seal by putting the tip of their tongue between the lips and their respiration was through the nose. Later, growth changes make it possible to breathe through the mouth. Although humans are primarily nasal breathers, when the need for air increases, mode of breathing changes from nasal to partially oral. In healthy adults, the switch from nasal to oronasal breathing occurs when ventilatory exchange rates above 40–45 L/min are reached (Niinimaa et al. 1981). This shift is transient, and when the need for air decreases back to normal, the individual goes back to nasal breathing. Human nasal passages also exhibit spontaneous changes in unilateral nasal airway resistance as a result of alternate nasal congestion and decongestion on opposing sides of the nose. This nasal cycle is said to last between 4 and 6 h, but fluctuations in nasal patency from 10 min to several days have been shown to occur (Huang et al. 2003; Chaaban and Corey 2011).
Mouth breathing can be defined as a shift from nasal respiration to oral respiration or mixed respiration due to obstruction or restriction on any part of the airway. Causes of such a nasal obstruction followed by a transition to mouth breathing can be adenoid or tonsil hypertrophy, chronic and allergic rhinitis, nasal traumas, congenital nasal deformities, foreign bodies, polyps, and neoplasms (Schlenker et al. 2000). It has been reported that when any of these factors increases the nasal resistance and pressure, the patients sometimes break the anterior and posterior oral seals resulting in oral respiration (Rodenstein and Stanescu 1984). It is also possible for mouth breathing to occur as the result of habit, with or without any impairment of the upper airway (Fields et al. 1991).
Treatment of dentofacial deformities caused by mouth breathing should be preceded by a thorough ENT examination to determine whether the cause is habitual or obstructive. If the cause is habitual, the treatment goal is to obtain a lip seal and force the patient to breathe through the nose. However, in cases of mouth breathing due to respiratory obstruction, the treatment should focus on relieving the obstructive cause.
Various diagnostic methods have been used in research to determine respiratory mode (James and Hastings 1932; Paul and Nanda 1973; Humphreys and Leighton 1950; Rasmus and Jacobs 1969; Melsen et al. 1987; Woodside and Linder-Aronson 1979; Bresolin et al. 1983; Miller 1949). Others have used the presence of adenoids (Tarvonen and Koski 1987; Sosa et al. 1982) without determining the respiratory mode. Most of these diagnostic tests have been indicated to be inconsistent and lacking in sensitivity and specificity (Ung et al. 1990; Vig et al. 1991). With the improvements in physiologic diagnostic methods, rhinometric measurements such as nasal resistance came to be widely used in research. However, associations between nasal resistance and respiratory mode were reported to be variable and weak (Warren et al. 1991; Vig and Zajac 1993; Ellingsen et al. 1995). Advances in respirometric techniques made it possible to measure the volume of nasal and oral airflow simultaneously which provided valuable information in this controversial area. Gurley and Vig (1982) suggested a technique for the simultaneous measurement of nasal and oral respiration which is called Simultaneous Nasal and Oral Respirometric Technique (SNORT). This technique measured the ratio of oral to nasal airflow and made the quantification of normal and abnormal respiratory modes possible. Other techniques were used to determine the dimensions of nasal airway impairment (Warren et al. 1984, 1986, 1988). Hairfield et al. (1987) reported a mean cross-sectional nasal area of 0.65 cm2 in adults. Warren et al. (1988) suggested that if nasal size falls below 0.4 cm2, most individuals will become oral breathers to some extent. These values would probably be smaller in children since several studies have indicated that nasal cross-sectional area increases with growth (Vig and Zajac 1993; Laine and Warren 1991; Crouse et al. 1999).
Perhaps the most significant finding of these studies is that one should be careful when classifying patients as oral breathers. Even in a population referred with an impaired airway, there will be oral, nasal-oral, or total nasal breathers as well as habitual oral breathers with adequate nasal airways. There are no clear cutoff points to determine the mode of breathing, and oral or nasal respiration seems to be a transient phenomenon in many individuals (Shanker et al. 2004). Since the intensity of functional changes is important in the magnitude of growth alterations, the question becomes if partial airway obstruction can lead to reflex adaptive changes that cause dentofacial deformities.
Another important factor to consider is the age at which dentofacial growth changes and breathing mode are evaluated. In order for any functional change to have a significant effect on facial growth, it must start early and be effective for a long time, especially during the peak growth period. However, cross-sectional studies that investigate subjects before or a long time after their growth spurts may not show any differences between groups because in younger subjects the growth changes would not have occurred yet, whereas in older subjects nasal airway may no longer be compromised due to growth changes in nasopharynx and lymphoid tissue.
Individuals also differ from each other in terms of adaptation and compensation processes. Several morphological factors may determine the extent of postural response to an inadequate airway. Subjects with compromised oropharyngeal airways due to size and shape of soft palate or tongue may give more exaggerated responses to a decrease in nasal airflow. The dentofacial changes observed in these individuals might be more pronounced. However, if the oropharyngeal airway is clear, only a slight parting of the lips may be enough to increase airflow (Bailey et al. 1996).
The extent of dentofacial changes due to any functional disturbance will be determined by multiple factors. Among these factors the age of the patient, the duration of the habit, and individual variations should be considered while making treatment decisions.
38.3 Physiologic and Dentofacial Effects
38.3.1 A Review of Early Literature
The influence of nasal respiratory function on the growth and development of craniofacial structures was first generated over a century ago by anecdotal reports describing the effects of “mouth breathing” on dental and facial morphology.
In 1872, Tomes (1872) described the dentofacial changes associated with chronic nasal airway obstruction, citing the lips-apart posture as the cause for decreased pressure on the incisors and proclined anterior teeth. He also coined the term “adenoid faces” to describe the associated facial changes.
In 1925, Dr. Edward H. Angle reprinted a book by George Catlin entitled “The Breath of Life (All Life on Earth is Breath, All Else on Earth is Death).” This book by Catlin advocated the superiority of nasal breathing over mouth breathing in sleep and described the consequences of habitual mouth breathing on teeth and facial features (Goldsmith and Stool 1994). Dr. Angle (1900) was also a firm believer in these concepts and stated in his textbook:
When there is normal nasal respiration and normal relations of the dental arches, the teeth, and the muscles, the conditions are such as to perfectly maintain the equilibrium and the mutual support necessary to the normal development of the teeth and jaws. Should nasal obstruction occur in the developing child, inducing habitual mouth-breathing, immediately the equilibrium is disturbed, the lips and muscles are placed on a different tension, and pressure upon the arches, instead of being equal, is localized, being greater than normal at some points and less at others. No matter how strenuously it may be denied, malocclusion of the teeth and abnormalities in the formation of the bones of the jaws naturally follow. The undeveloped nose and adjacent region of the face, the vacant look, the short upper lip, the open mouth, and irregular teeth of the mouth-breather are common sights familiar to all.
Later other reports reiterated the relationship between altered dentofacial form and mouth breathing. Chronic nasal allergies were suggested to cause paranasal depression, V-shaped palate, and proclination of the maxillary incisors (Duke 1930; Balyeat and Bowen 1934). Cohen (1937) attributed mouth breathing due to allergies to high-arched and narrow palates, a flat and narrow face, and some type of orthodontic deformity (although he did not classify which type). Subtelny (1954) theorized that enlarged adenoids will cause a separation of the lips, downward and forward movement of the tongue away from the soft palate, depression in the position of the mandible, constriction of the maxillary arch, and a Class II division 1 type of malocclusion due to procumbent maxillary anterior teeth. Paul and Nanda (1973) also found a tendency toward Class II malocclusion with an increase in overbite and overjet in mouth-breathing subjects when compared to nasal breathers.
Different theories were proposed to explain the relationship between respiratory mode and possible dentofacial changes. Morrison (1931) suggested that the oral airstream in mouth-breathing individuals caused the negative pressure between the tongue and palate to be lost hindering normal downward palatal descent. James and Hastings (1932) proposed that the loss of the normal pressure in the mouth due to an impairment of the airway is associated with impaired action of the tongue, lips, cheeks, and other forces acting on the jaws. They considered the impaired and misdirected action of these forces as the reason for the deformities of the jaws. A clearer understanding of these effects was possible when Moss (1962) developed the “functional matrix theory.” This theory was based on the principle that the skeletal unit in the functional craniofacial component provides protection and mechanical support for its specific functional matrix and grows in response to the functional demands of surrounding tissues and structures. According to Moss’s theory nasal breathing allowed proper growth and development of craniofacial and dentofacial complex (Moss 1969). Later, Solow and Tallgren (1976) found an association between the posture of the head and cervical column and craniofacial alterations seen in mouth-breathing patients. These results led to an alternative explanation known as “Soft Tissue Stretching Hypothesis” (Solow and Kreiberg 1977). This theory suggested that nasal obstruction caused extension of the head and that this postural change causes soft tissue stretching causing differential forces to act on skeleton causing morphological changes. Hence, the existence of a relationship between respiratory mode and dentofacial growth changes was widely accepted, and early treatment of allergies and removal of adenoid tissue before the eruption of permanent teeth were suggested to prevent the alterations in dental arches (Subtelny 1954; Marks 1965).
However, there were others who were skeptical of such wide acceptance of a possible relationship between oral respiration and growth changes. Kingsley (1889) considered the deep and narrow palate a congenital morphological trait rather than the results of a muscle imbalance due to mouth breathing. Gwynne-Evans and Ballard (1959) observed the relationship between jaw form, soft tissue morphology, and upper respiratory conditions for more than 15 years and concluded that mouth breathing does not result in deformities of the jaws, malocclusion, or adenoidal facies. Other authors reported that more than 50 % of the patients who were characterized as mouth breathers had Class I occlusions and no specific malocclusion pattern was correlated with mouth breathing (Howard 1932; Leech 1958; Huber and Reynolds 1946).
Since then, investigators have attempted to look more critically at the issue through experimental models and clinical research with objectively defined criteria for mouth breathing. Harvold (1968) used the rhesus monkey, Macaca mulatta, as a model in his experiments to test the connection between neuromuscular activity and skeletal morphogenesis. He anchored a piece of plastic in the palatal vault between the molars and found that the mandible moved lower and the tongue moved forward resulting in an anterior open bite. This study was followed by another one in which the animals were induced to lower their mandibles by fitting an acrylic block in the palatal vault (Harvold et al. 1972). After 6 months there was a significant increase in face height in experimental groups. They concluded that any factor, such as mouth breathing, that lowers the postural position of the mandible could also increase the face height. They tested their hypothesis by blocking nasal inhalation with silicone nose plugs in growing monkeys (Harvold et al. 1973, 1981). Radiographic, electromyographic, and dental cast measurements showed increased face height, decreased maxillary and mandibular intercanine distance, decreased maxillary dental arch length, steeper mandibular plane, larger gonial angle, altered muscle activity, and changes in the morphology of the tongue in the experimental group. The pattern of maintaining an airway differed between monkeys. Those that kept their mouths constantly open by lowering the mandible and protruding their tongues developed more severe malocclusions than those that rhythmically opened and closed their mouths with respiration.
The altered muscle activity in the rhesus monkeys due to forced oral breathing was further explored in other studies (Miller et al. 1982; 1984; Vargervik et al. 1984). These experiments documented changes in neuromuscular recruitment patterns resulting in changed function and posture of the mandible, tongue, and upper lip with considerable variation among the animals and concluded that nasal obstruction can induce neuromuscular changes which extend beyond the period of obstruction and remain even after nasal breathing is established.
More recent animal studies also found that nasopharyngeal respiratory obstruction was associated with downward and backward rotation of the mandible, upward and backward growth of the condyle, divergent gonial angle, anterior open bite, spaced dental arch in the lower anterior region, and a reduction in the height of the maxilla (Yamada et al. 1997; Scarano et al. 1998).
These experimental findings corroborated the previous data on the relationship between mouth breathing and an increase in facial height. However, it should be kept in mind that the results of these animal studies cannot be readily extrapolated to humans. Total nasal obstruction, as induced by researchers in these experiments, is extremely rare in humans. The oropharyngeal structures also differ between the species. Thus, the postural changes that occur in animals due to forced oral breathing may not be the same in humans.
Early clinical studies on humans generally used lateral cephalograms to evaluate dentofacial changes and the upper airway. Linder-Aronson (1970) studied 162 children aged 6–12 years. Half of these children were determined to need adenoidectomies, while the other half were controls. The patients were examined with respect to nasal airflow, breathing pattern, and dentofacial morphologic variables. He reported a significant relationship between enlarged adenoids determined by cephalometric x-rays and certain craniofacial changes, including low tongue position, mouth breathing, narrow maxillary arch, crossbite, and retroclined maxillary and mandibular incisors. In 1974, he examined a group of Swedish children before and after adenoidectomies and compared them to controls with respect to changes in cephalometric measurements. He reported that the patients in adenoidectomy group had increased anterior facial height, maxillary constriction, and retroclined incisors compared to controls. After their adenoidectomies, upper airway obstruction was resolved in these patients and their growth pattern became horizontal (Linder-Aronson 1974).
Hannuksela (1981) compared allergic and nonallergic children and reported a tendency toward clockwise rotation of the mandible and retroclined mandibular incisors. However, further evaluation of this population revealed no significant differences in the occlusion between groups (Hannuksela 1983). Other cephalometric studies also failed to show a relationship between the airway space or adenoid size and malocclusion (Sosa et al. 1982; Mergen and Jacobs 1970).
Lateral cephalograms were readily available to orthodontists and valuable in determining dentofacial changes. They were also recommended for assessing adenoid size (Shapiro and Shapiro 1984). However, since lateral cephalograms are two dimensional and unable to provide volumetric data, their reliability in determining airway size and adenoids have been criticized (Vig and Hall 1980; Maw et al. 1981).
With the development of respirometric techniques, a more objective classification of respiratory patterns became possible. Vig et al. (1981) reported higher nasal resistance in increased facial height groups compared with controls, but they found no significant differences in the nasal volume flow rate between groups. Fields et al. (1991) also concluded that subjects with long faces had a significantly smaller component of nasal airflow. Warren and Spalding (1991) suggested that high airway resistance due to nasal impairment may cause an exaggerated postural response if there is a low drape to the velum, the pillars form a posterior curtain, the tonsils are enlarged, or the posterior portion of the tongue is carried high.
The early clinical studies that used lateral cephalograms and/or other respirometric techniques showed that the relationship between dentofacial growth and development and respiratory mode is variable and multifactorial.
38.3.2 Current Perspective
Heredity and environmental factors are both effective in the development of dental arches and postnatal determination of craniofacial features. One of the most important environmental factors is the predominant respiratory pattern. Nasal breathing is associated with normal posture of the tongue and lips and normal muscle activity. If there is nasal obstruction, this would likely affect the muscle forces acting on the dentofacial region. This change in muscular action may cause abnormal facial growth and development. It has been shown that during oral breathing masseter muscle activity is inhibited (Ono et al. 1998). Increased airway resistance also stimulates mechanoreceptors in the upper airway and increases the activities of the genioglossus and mylohyoid muscles due to forward positioning of the tongue and opening of the mouth to maintain the airway (Song and Pae 2001).
Today, it is accepted that growth occurs under the control of both genetic and environmental factors. Genetics act on cartilages and the bones respond to the changes in these cartilaginous structures. The growth and needs of the soft tissue matrix also cause reactive changes in both the bone and the cartilage.
Long-term mouth breathing seems to affect the occlusion and facial morphology during periods of rapid growth. However, not every patient has the same growth changes due to oral breathing. The heritable characteristics of anatomical structures also seem to play a role in determining which patients will be most affected. In some patients a slight opening of the lips may be enough to provide the necessary airway, while in others a more exaggerated postural response of the mandible, tongue, and head will be necessary. Children with narrow facial patterns also may be more susceptible to growth changes due to mouth breathing than children with broad facial features. It is also possible for patients with a vertical facial growth pattern to be more likely to be mouth breathers. The severity of the obstruction will also determine if the child is a chronic mouth breather or a partial one. If the obstruction is severe, the changed postural responses will be in place longer causing more extensive growth changes in dentofacial structures.
If the patient has morphologic risk factors in the oropharynx such as enlarged tonsils, a large tongue, or a long soft palate, the postural response necessary to open the airway will be more pronounced and the risk for developmental disturbance will be greater.
The most common cause of oral breathing in children is enlarged pharyngeal lymphoid tissue. The enlargement of these tissues may adversely affect pharyngeal patency (Gross and Harrison 2000). Normally, the size of the adenoid tissue is dependent on the associated skeletal structures. However, abnormal growth of this tissue may predispose the patient to upper airway obstruction causing oral respiration. As a matter of fact, any reason that causes nasal resistance to increase for long periods of time, such as allergies or nasal septal deformity, has the potential to cause chronic oral respiration.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


