17
Philosophy of Cholesteatoma Management
The effective control of acute otitis media with antibiotic therapy has significantly reduced the number of cases of acute coalescent mastoiditis. However, the widespread use of antimicrobials has not been as effective in decreasing the incidence of chronic mastoiditis due to cholesteatoma or in eliminating its complications.
Cholesteatoma, a destructive process that involves the middle ear and mastoid, is a common otologic disorder. This lesion, which histologically consists of squamous keratinizing epithelium, resembles normal skin. However, the biological hallmarks of cholesteatoma, specifically invasiveness, unrestrained proliferation, aggressiveness, and recidivism, suggest a fundamental alteration in the normal biology of one or more of the cellular constituents of cholesteatoma (i.e., fibroblasts and keratinocytes).1–5
The otologic surgeon has the option of using one of several operative approaches to treat cholesteatoma. The selected surgical technique must provide the necessary exposure to permit complete removal of cholesteatoma, thus effectively minimizing the postoperative incidence of residual disease. Additionally, the surgeon must consider the patient’s eustachian tube function and assess various anatomical factors to avoid recurrent disease. Thus a method for avoiding recidivism (i.e., residual plus recurrent cholesteatoma) must be established. Postoperatively, the ear must be stable, dry, and trouble free. Finally, a serviceable hearing level should be achieved in the operated ear.
This chapter outlines the authors’ preoperative management of patients with cholesteatoma and clinical approach for selecting the most appropriate operative procedure.
■ Preoperative Management of Chronic Mastoiditis Caused by Cholesteatoma
Generally, a cholesteatoma is a slowly enlarging process. However, when water gets into an ear with a cholesteatoma, the growth and the desquamation of keratin are accelerated. Retention of this cheesy white material is associated with growth of this pathological process and its erosion into surrounding structures. Furthermore, this moist keratin material is a good media for bacterial and fungal growth, which predisposes the patient to develop a superimposed secondary acute ear infection that is usually characterized by the presence of granulation tissue, a foul-smelling discharge, and, occasionally, ear pain. Frequently, Pseudomonas or a fungus will be cultured from the ear canal, but it remains controversial whether they represent the primary infectious organism or, more likely, saprophytes growing in a moist environment. Consequently, when a person with a cholesteatoma gets water in the ear during bathing or swimming or when the ear becomes moist in association with an upper respiratory infection, a secondary acute infection will frequently occur. These exacerbations can usually be controlled during an office visit. The ear is examined using an operating microscope, and any keratin debris is meticulously removed. Granulation tissue should be excised and its vascular base neatly cauterized. Topical eardrops with an acidic pH and an adequate course of a systemic broad-spectrum antibiotic or antifungal medication should be prescribed. Control of the superficial secondary infection that diminishes vascularity prepares the ear for surgery, which is the definitive treatment of cholesteatoma.
■ Operative Management
The primary goal of the surgical treatment of chronic mastoiditis due to cholesteatoma is its complete eradication to provide the patient with a safe, dry ear. This can be accomplished by meticulously removing all of the cholesteatoma, diseased bone, granulation tissue, and irreversibly diseased mucosa. An important but secondary goal is to improve or preserve the hearing acuity by restoring an aerated middle ear cleft and reconstructing the tympanic membrane and the ossicular mechanism. An additional goal is to minimize the need for long-term care of the operated ear and concern about getting water in the ear when bathing or swimming.
The procedures used for treating cholesteatoma may be divided into two broad categories. One is a canal wall up (CWU) or closed technique, in which an air-containing mastoid and an external ear canal are preserved (Fig. 17–1). The second category is canal wall down (CWD) or open technique, in which the posterior canal wall is removed and the mastoid marsupialized into the enlarged ear canal, thus eliminating the need to aerate itvia the middle ear cleft (Fig. 17–2). Regardless of which procedure is used, the primary criterion for a successful result should be the permanent eradication of the cholesteatoma. The selection of a specific operative technique should be determined by the extent of the cholesteatomatous invasion in conjunction with a clinical assessment of eustachian tube function, the degree of mastoid pneumatization, and the anatomical configuration of the patient’s mastoid.
In our management scheme, assessment of eustachian tube function is a critical, though admittedly illusive, determination. We feel that if tubal function is inadequate, CWU procedures are likely to develop recurrent disease and will fail. Can an operation that preserves the contours of the external auditory canal and reconstructs the hearing mechanism be considered a success if the cholesteatoma recurs, thereby requiring CWD revision surgery?
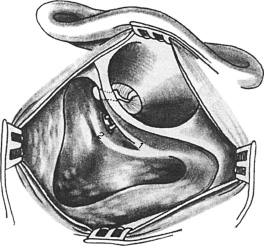
FIGURE 17–1 Canal wall up technique. A mastoidectomy has been performed in which the canal wall has been preserved. The posterior middle ear has been entered by drilling between the chorda tympani (1) and facial nerve(2).
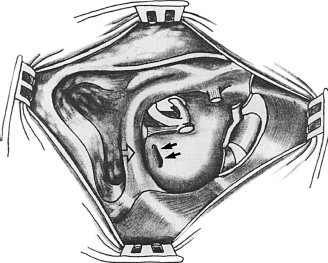
FIGURE 17–2 Canal wall down technique. The posterior canal wall has been lowered down to the vertical facial nerve (open arrow). The mastoid is marsupialized into the external ear canal. All accessible air cells have been meticulously exenterated. Skeletonizing the vertical portion of the facial nerve unroofs the sinus tympani (solid double arrows).
Three clinical indicators have been identified that we have found useful for assessing eustachian tube function in patients undergoing surgery for cholesteatoma. The first is the otoscopic appearance of the tympanic membrane. A normal pars tensa suggests that the eustachian tube effectively ventilates the middle ear cleft and therefore might function adequately enough to aerate the mastoid and support a CWU procedure. This is often encountered in ears with an attic–antral block in which otoscopic pathological changes are localized to the pars flaccida. In these ears the presence of a middle ear effusion behind an otherwise normal pars tensa presents a dilemma. It may indicate that tubal function will be inadequate to ventilate the mastoid if the canal wall is preserved. However, in some instances the eustachian tube dysfunction may have been caused by correctable abnormalities that produce occlusion of the middle ear tubal aperture. Examples of reversible processes are acute inflammatory mucosal changes, a prolapse of the cholesteatoma that blocks the lumen, or an inflammatory synechial band. In such cases with a middle ear effusion, a CWU procedure could be considered. Alternatively, the observation of a severely retracted pars tensa suggests that the patient has had inadequate eustachian tube function and therefore is a poor candidate for a CWU technique.
The second clinically useful indicator of eustachian tube function is mastoid cellular development. The presence of a large pneumatized temporal bone, especially if aerated, suggests good eustachian tube function and encourages the authors to consider a CWU procedure. In ears with an attic–antral block, it is not uncommon to observe fluid or cholesterol granulomatous disease in a well-developed cellular mastoid. Because this can be surgically corrected, it would still allow the authors to perform CWU surgery. In contradistinction, a contracted sclerotic mastoid would be one of the factors that would encourage us to select a CWD operation, especially given that the resulting mastoid bowl would be small and easy to care for postoperatively.
The third clinical clue used to assess eustachian tube ventilation is the status of the middle ear mucosa. A normal, thin translucent middle ear mucosa indicates that the middle ear cleft ventilation has been normal and is a good indicator that CWU surgery can be successfully performed. Hyperplastic, polypoid, irreversibly diseased middle ear mucosa or adhesive-type changes in which squamous epithelium lines the promontory indicate that eustachian tube function has been compromised. Furthermore, middle ear mucosal abnormalities that are diffuse and extend to involve the mastoid are suggestive that the existing eustachian tube dysfunction may not be correctable. In such cases, the authors favor a CWD procedure.
Ultimately, the selection of an operative technique is multifaceted and is made during the operative procedure. It is based on an accurate intraoperative assessment of the extent of cholesteatomatous involvement. The surgeon, during the operative procedure, given an individual patient’s middle ear and mastoid anatomical configurations, must determine which procedure to choose to gain the exposure necessary to completely eradicate the disease process. This is done in conjunction with the clinical assessment of eustachian tube ventilation already described.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


