Petroclival meningiomas are most commonly found in women around 50 years of age and have the general tendency to grow and affect several cranial nerves. At presentation, many patients complain of headaches, gait disturbances and cranial neuropathies. Treatment options include surgery, with a variety of surgical approaches, and or radiotherapy. Current trends support subtotal resection with postoperative radiotherapy. This review summarizes the literature of petroclival meningiomas, discussing topics including definitions, genetics, common presenting signs and symptoms, imaging characteristics, natural history, common surgical approaches, surgical outcomes, complications, and radiotherapy.
Key points
- •
Approximately 2% of meningiomas are located in the petroclival region, most commonly encountered in women around the age of 50 years.
- •
Preoperative imaging includes computed tomography and MRI, while 4-vessel cerebral angiography is commonly obtained.
- •
Common surgical approaches include retrosigmoid, Kawase, orbitozygomatic, and transpetrosal approaches.
- •
With the tendency to grow and affect several cranial nerves if observed, general current management trends support subtotal resection with postoperative radiotherapy with 10-year progression-free survival around 80%.
- •
Complications include cranial nerve deficits, cerebrospinal fluid leakage, hydrocephalus, and brainstem infarctions.
| CN | Cranial nerve |
| CSF | Cerebrospinal fluid |
| CT | Computed tomography |
| GTR | Gross-total resection |
| IAC | Internal auditory canal |
| KPS | Karnofsky Performance Status |
| NF | Neurofibromatosis |
| WHO | World Health Organization |
Introduction
Petroclival meningiomas are intracranial masses with dural attachments to the petroclival synchondrosis, typically near the upper two-thirds of the clivus. Some authors further delineate petroclival meningiomas as those medial to the cranial nerve (CN) foramina V through XI, while others only consider petroclival meningiomas as those medial to the trigeminal nerve ( Fig. 1 ). With petroclival meningiomas originating near the petroclival suture, given the variety of shapes and sizes, significant neighboring structures can be compromised, including the internal auditory meatus, Meckel cave, cavernous sinus, jugular foramen, parasellar region, foramen magnum, as well as the brainstem, dura, and underlying bone. As such, it is difficult to compare tumor behavior and treatment outcomes between patients and series given the variety of tumor shapes and locations.
Hallpeau is first credited with describing a petroclival meningioma in a 50-year-old woman in 1874, with most subsequent reports describing patients presenting with motor nerve impairments secondary to tumor compression. Almost 80 years later, in 1953, Castellano and Ruggiero first classified posterior fossa meningiomas, describing the posterior portion of the petrous bone as 1 of 5 possible locations of tumor origination. Since then, further classifications have been described as well as an evolution of treatment strategies. In regards to meningiomas at all locations, the World Health Organization (WHO) classifies 16 different subtypes based on histopathology, categorized into 3 grade designations. Although benign (WHO I) tumors constitute 80% to 90% of all meningiomas, atypical (WHO II) tumors constitute 4.7% to 7.2%, and anaplastic or malignant (WHO III) tumors constitute 1.0% to 2.8%, recurrence and rates of mortality increase as the tumor grade increases. What follows is a literature review regarding the presentation, natural history, treatment, and outcomes of petroclival meningiomas.
Introduction
Petroclival meningiomas are intracranial masses with dural attachments to the petroclival synchondrosis, typically near the upper two-thirds of the clivus. Some authors further delineate petroclival meningiomas as those medial to the cranial nerve (CN) foramina V through XI, while others only consider petroclival meningiomas as those medial to the trigeminal nerve ( Fig. 1 ). With petroclival meningiomas originating near the petroclival suture, given the variety of shapes and sizes, significant neighboring structures can be compromised, including the internal auditory meatus, Meckel cave, cavernous sinus, jugular foramen, parasellar region, foramen magnum, as well as the brainstem, dura, and underlying bone. As such, it is difficult to compare tumor behavior and treatment outcomes between patients and series given the variety of tumor shapes and locations.
Hallpeau is first credited with describing a petroclival meningioma in a 50-year-old woman in 1874, with most subsequent reports describing patients presenting with motor nerve impairments secondary to tumor compression. Almost 80 years later, in 1953, Castellano and Ruggiero first classified posterior fossa meningiomas, describing the posterior portion of the petrous bone as 1 of 5 possible locations of tumor origination. Since then, further classifications have been described as well as an evolution of treatment strategies. In regards to meningiomas at all locations, the World Health Organization (WHO) classifies 16 different subtypes based on histopathology, categorized into 3 grade designations. Although benign (WHO I) tumors constitute 80% to 90% of all meningiomas, atypical (WHO II) tumors constitute 4.7% to 7.2%, and anaplastic or malignant (WHO III) tumors constitute 1.0% to 2.8%, recurrence and rates of mortality increase as the tumor grade increases. What follows is a literature review regarding the presentation, natural history, treatment, and outcomes of petroclival meningiomas.
Genetics
The neurofibromatosis 2 (NF2) gene on chromosome 22q is the most common genetic alteration in meningiomas, most frequently leading to a nonfunctional merlin protein. Studies show that loss of heterozygosity of chromosome 22 occurs between 40% and 72% of sporadic meningiomas. Nonetheless, NF2 mutations occur equally between meningioma tumor grades. Other mutations include 1p deletions, which are co-deleted with chromosome 22q in 67% of meningiomas and are associated with progression and recurrence. Tissue inhibitor of metalloproteinase 3 is another commonly altered gene, found to be hypermethylated in 67% of anaplastic meningiomas, inactivating its tumor suppression activity, compared with only 17% of benign meningiomas. With other epigenetic changes, He and colleagues found that CDKN2 and TP73 gene hypermethylation in meningiomas interacts with the p53 cell cycle regulation, preventing normal cell cycle checkpoint function. Despite these findings, further studies are ongoing to determine factors or profiles that help predict growth and treatment outcomes.
Presentation
Roughly 20% of intracranial masses are meningiomas, 10% of which are located in the posterior fossa, with about 2% of all meningiomas located in the petroclival region. Others estimate that petroclival meningiomas account for 0.15% to 0.4% of all intracranial tumors. They are more frequently found in women, ranging in ratios with men from 1.3 to 5.7:1, but generally around 3:1. The average age at presentation is between 47.8 and 54.4 years.
Studies report a variety of presenting symptoms, including headache, facial numbness, dizziness, and gait disturbances, with many patients also exhibiting facial weakness, hearing impairment, and diplopia. Depending on the report, upwards of 90% of patients in some studies have presented with headaches or gait disturbances, while reports as high as 89% of patients have cranial neuropathies at baseline, with CN V most commonly affected.
Initially, poor outcomes were associated with surgical resection; thus, to help compare postoperative outcomes, several studies report performance scores and assessments, including the Karnofsky Performance Status (KPS) score, the Glasgow Outcome Scale, the modified Rankin scale, and the Petroclival Meningioma Impairment Scale. Of the studies that report preoperative KPS scores, scores range from 74.2 to 85.3. Not surprisingly, Van Havenbergh and colleagues found a significant inverse correlation between absolute tumor diameters or tumor volumes and KPS scores.
Imaging
Initially roentgenograms were used to assess skull-base erosion, while cerebral angiography was used to differentiate petroclival meningiomas from intracranial chordomas and brainstem gliomas. The advent of computed tomography (CT) imaging allowed better identification and categorization of all intracranial lesions, with Mayberg and Symon classifying posterior fossa meningiomas based on their site of origin in 1986. On CT imaging, all meningiomas tend to appear slightly hyperdense (70%–75%) to isodense (25%) with broad-based dural attachments. Furthermore, calcification and cyst formation are noted in about 20% of cases, while hyperostosis is seen in 20% to 40%.
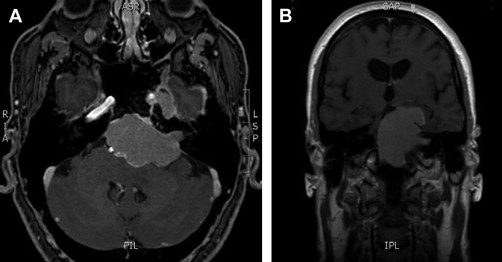
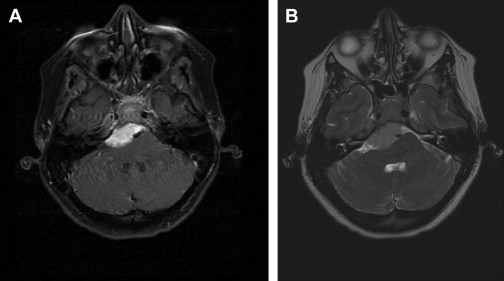
In 1987, the first report describing MRI for preoperative evaluation of petroclival meningiomas was published. On MRI, all meningiomas on T1-weighted imaging appear slightly hypointense to isointense, while variably isointense to hyperintense on T2-weighted imaging ( Fig. 2 ). In addition, several imaging characteristics are associated with meningiomas, such as peritumoral edema and a “dural tail,” the latter of which occurs in 35% to 80% of tumors, best appreciated with the administration of gadolinium ( Fig. 3 ). Many studies have reported on MRI in predicting tumor resectability, with edema on T2-weighted imaging suggesting brainstem adherence or invasion, or loss of an arachnoid plane on T1-weighted or T2-weighted imaging indicating pial invasion, findings which would suggest a more difficult resection ( Fig. 4 ).
In addition to preoperative CT and MRI, many groups still use preoperative 4-vessel cerebral angiography to assess the intracranial vasculature. In one of the largest studies to date, Natarajan and colleagues obtained preoperative cerebral angiography on all patients, embolizing 61%. However, most groups will only obtain angiography if the cavernous sinus and the carotid or basiliar arteries are involved, and thus, assess if preoperative embolization may facilitate surgical resection ( Fig. 5 ).
Natural history
The risks, benefits, and alternatives of treating petroclival meningiomas must be weighed against their natural history. Van Havenbergh and colleagues retrospectively reviewed 21 patients with petroclival meningiomas who underwent no treatment for a minimum of 4 years, and an average of almost 7 years. They found that 76% of tumors demonstrated growth on imaging, with 50% of the original asymptomatic patients exhibiting at least one CN deficit, and 20% of those patients with at least one CN deficit developing additional CN involvement. Furthermore, by using either CT or MRI to determine the tumor-equivalent diameter and tumor volume, they found that the overall tumor diameter and tumor volume growth rates were 0.81 mm/y and 0.81 cm 3 /y, respectively. These growth rates pale in comparison with a previous study reviewing the postoperative courses of 38 patients who underwent subtotal resection of petroclival meningiomas without further treatment, reporting tumor diameter and volume growth rates of 3.7 mm/y and 4.94 cm 3 /y, respectively. Despite the different growth rates, without intervention, petroclival meningiomas are expected to grow.
Treatment
With the propensity for patients with petroclival meningiomas to present with significant complaints and the tendency for the tumors to grow, there are many studies discussing the variety of treatment options. Although initial reports demonstrated significant morbidity and mortality, with the advent of microsurgical techniques as well as radiotherapy, either modality alone, or together, has greatly reduced the morbidity and mortality in treating these lesions. Table 1 summarizes all studies reporting at least 50 cases of petroclival meningiomas with surgical intervention.



