FIGURE 6.1 Cochlear Malformations.
Drawings were made from coronal CT scans. (From Jackler RK, Luxford WM, House WF. Congenital malformations of the inner ear: a classification based on embryogenesis. Laryngoscope. 1987;97(suppl 40):2 and Flint PW, Haughey BH, Lund VJ, et al. Cummings Otolaryngology—Head and Neck Surgery. 6th ed. Philadelphia, PA: Saunders; 2015.)
• Aqueduct anomalies:
• Normally 0.4-1.0 mm in diameter when measured halfway between the common crus and its external aperture
• Enlarged vestibular aqueduct (Fig. 6.2) is the most common identified temporal bone abnormality in children imaged for SNHL; defined by vestibular aqueduct size of >1 mm at the midpoint and >2 mm in diameter at the operculum; progressive and sudden decrements in hearing with approximately 40% eventually developing profound SNHL; the likelihood of hearing loss progression increases as the size of the vestibular aqueduct increases; type of hearing loss can be SNHL, mixed, or purely conductive9
• Enlarged cochlear aqueduct: usually 3-4 mm in diameter and ranges from 1 to 10 mm; significance is controversial
• Internal auditory canal (IAC) abnormalities
• Narrow IAC: <3 mm; if facial function is present, then CNVIII will most likely be absent; magnetic resonance imaging (MRI) of the temporal bone should be ordered to determine further the presence of the cochlear nerve
• Widened IAC: >10 mm is associated with a cerebrospinal fluid (CSF) gusher in the cochlear implantation and stapedectomy
Joint Committee on Infant Hearing Position Statement for Neonatal Hearing Screening: Birth to 28 Days
• Recommends universal newborn screening before hospital discharge; infants who pass the neonatal screening but have a risk factor should have at least one diagnostic audiology assessment by 24 to 30 months of age; if risk criteria are met, recommend additional testing later, even if the newborn screening was passed
• Prematurity
• Family history of childhood SNHL
• Congenital infections/sepsis
• Low Apgar scores
• TORCH (Toxoplasmosis gondii, other viruses, rubella, Cytomegalovirus [CMV], and herpes simplex)
• Craniofacial abnormalities
• Low birth weight
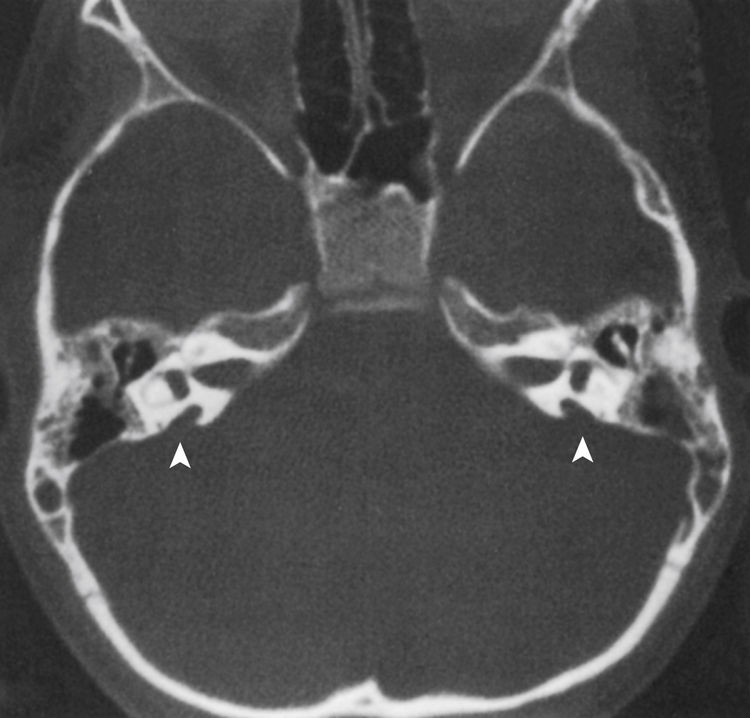
FIGURE 6.2 Bilateral enlargement of the vestibular aqueducts (arrowheads) as seen on an axial CT scan. (From Flint PW, Haughey BH, Lund VJ, et al. Cummings Otolaryngology—Head and Neck Surgery. 6th ed. Philadelphia, PA: Saunders; 2015.)
• Bacterial meningitis
• Ototoxic antibiotics (gentamicin/tobramycin)
• Hypoxemia
• Encephalopathy
• Loop diuretics (furosemide/Lasix)
• Mechanical/assisted ventilation
• Stigmata of a known syndrome associated with hearing loss
Joint Committee on Infant Hearing Position Statement for Infants (29 Days To 2 Years) Hearing Screening (Table 6.1)
• Separate risk criteria for infants: different from newborns (may need earlier and more frequent testing)
• Persistent otitis media with effusion (OME) for at least 3 months
• Parent concern regarding hearing, speech, language, or developmental delay
• Head trauma resulting in skull fracture
• Family history of delayed-onset hearing loss
• Neonatal intensive care unit (NICU) stay >5 days
• Extracorporeal membrane oxygenation history
• Presence of neurodegenerative disorders
• Meningitis
• Chemotherapy medications with potential ototoxicity
• Childhood infections associated with SNHL (meningitis and CMV)
Methods of Audiologic Evaluation (Newborn to 48 Months)
1. Auditory brainstem response (ABR), also known as a brainstem auditory evoked response test
a. For hearing screens: automated ABR (A-ABR) or screening (S-ABR) systems test for the presence or absence of wave V at soft stimulus
i. Stimulus is usually click stimuli at 35-40 dB, with no operator interpretation.
ii. Results are given as Pass or Refer for each ear.
iii. It is a highly effective screening with sensitivity/specificity of 96-98%, but it does not rule out minimal or mild hearing loss.
b. Diagnostic ABR: Used when hearing loss is suspected because of an abnormal A-ABR screening result (OR absent otoacoustic emissions (OAEs) screening result; see OAE section).
i. Used to determine frequency-specific hearing thresholds, as well as type of hearing loss (sensorineural, conductive, or mixed)
ii. Child must be completely asleep throughout testing; often requires sedation after 6 months of age
iii. An ABR is not a “functional” test of hearing, but it is an estimated hearing test in which the child does not actively participate; there is no cortical processing; results should always be confirmed or supported by behavioral testing when possible (see Behavioral auditory testing section).
2. OAEs for hearing screens or as part of an audiologic test battery (Note: can only be used as a screen for well babies, not NICU babies)
a. OAEs test cochlear outer hair cell function; if present, cochlear outer hair cell function is normal and normal-to-near-normal hearing is assumed; there are two types of OAEs:
i. Transient evoked OAE (TEOAE)
(1) Click stimuli at 80-86 dB; typically only tests a small range of frequencies
(2) May be present/pass even with mild hearing loss (about 30 dB)
ii. Distortion product OAE (DPOAE)
(1) More frequency-specific compared with TEOAE and can test a wider range of frequencies
(2) May be present even with mild hearing loss (about 30 dB)
b. Factors that may adversely affect testing:
i. Debris or cerumen in the external auditory canal (EAC)
ii. Poor probe fit because of stenotic canal
iii. Middle ear effusion (MEE) or any conductive component
iv. Patient compliance—patient must be relatively quiet and still throughout testing
c. OAE testing may miss auditory neuropathy spectrum disorder: in this case, children will have present OAEs, but an abnormal ABR
3. Behavioral auditory testing
a. For infants/children of 6 months and older corrected age
c. Generally three types of test methods depending on age/developmental status:
i. Visual reinforcement audiometry (VRA)
(1) Child must be at least 6 months corrected age
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree